 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

On a sunny morning in Poway, a little boy named Gavin scampers around his backyard as his mother looks on. To the unassuming eye, this lean, blue-eyed towhead looks like any other fit four-year-old. But upon closer inspection, one might notice the sun glinting off his small silver anklet; when Gavin clambers up the side of his wooden play set, a white adhesive bandage can be seen on the back of his arm; as he wriggles his way down the plastic slide, his shirt rides up, revealing a tiny fanny pack around his waist. Each item is part of a collection of equipment that helps keep Gavin alive.

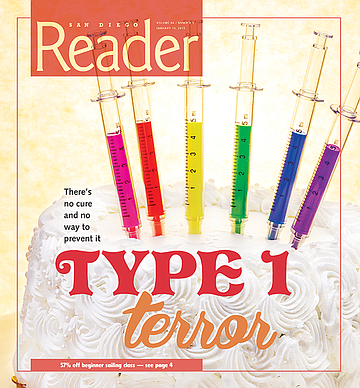
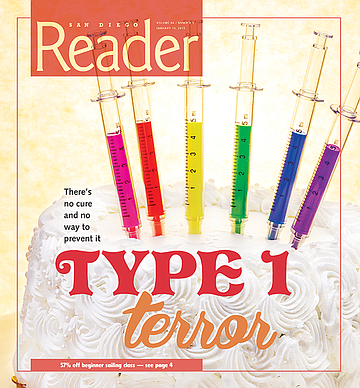
Gavin has type 1 diabetes. Unlike type 2, a metabolic disorder often related to poor diet and lack of exercise, type 1 is an autoimmune disease. There is no cure and no known way to prevent it. Nor is there a way to predict who will get it or when. “Gavin was a healthy, thriving baby,” says Sage Pierce, Gavin’s mother. “I breastfed him until he was a year old and then fed him organic baby food. He was a pretty darn healthy kid — no colds, no ear infections, nothing.”

When Gavin was 14 months old, Pierce started noticing “weird” things. “He would wake up in the morning and his lips would be blue.” When she asked her pediatrician about this, she was told her son might be cold in the morning. A few months later, Gavin began wetting his diaper three or four times a night. “Like, dripping wet, we’d have to change the sheets,” Pierce remembers. “I thought, Is this normal? I’m a new parent, I have no idea.” The doctor recommended larger diapers.
Commonly referred to as T1D, type 1 diabetes lies dormant until it is triggered, most often by something as simple as a cold. When we get sick, our immune system responds by leaping into action and killing the invading cells. For people with type 1 diabetes, this process malfunctions and the immune system targets, attacks, and kills crucial beta cells, which are the only cells in our bodies that create insulin, the hormone that delivers the precious energy source, glucose (i.e., sugar), to the cells. Without insulin, glucose builds up in the blood, depriving most cells and organs in the body of the energy they need to continue functioning. As a result, the body believes it is starving and begins processing fat for fuel, which creates acidic biproducts known as ketones. As these ketones build up, the body tries to rid itself of the extra toxins, primarily through urine. If the level of ketones gets too high, the consequences are dire: one could fall into a diabetic coma, or die.
What Pierce did not know at the time, was that Gavin was exhibiting the most common symptom of life-threateningly high blood sugar: excessive thirst, followed by frequent urination. The disease itself (technically known as diabetes mellitus) is named after this symptom. Diabetes comes from the Greek word for “siphon,” and mellitus from the Latin word for “honey.” In China, diabetes was dubbed the “sweet urine disease” after it was observed that sugar-loving insects such as ants were attracted to some people’s urine.
When Gavin was 18 months old, he traveled with his family to Detroit for a wedding and caught a terrible cold. Upon returning home, he was constantly thirsty. “He’d drink a whole sippy cup and then ask for another one,” Pierce says. “It got to the point where I emailed the doctor and said, ‘Something’s not right.’ We brought him in for blood tests on a Friday, when there weren’t any doctors, just the lab, and then we went home for the weekend, like it was no big deal.”
On Monday, November 14, 2011, Pierce received a call on her cell phone while she was at work. It was a nurse, informing her that Gavin’s test results indicated he was diabetic and she needed to bring him to Rady Children’s Hospital immediately.
Pierce, an executive producer for NBC San Diego, recalls that moment.
“I was sitting there in the newsroom, like, what? In my mind, diabetes meant type 2 — my grandmother died of type 2. I was, like, This kid’s skinny, he eats healthy, what the hell? My stomach was just falling and I was crying at my desk. I called my husband, and he didn’t even know type 1 was a thing.”
At the hospital, Pierce, her husband Mike, and Gavin sat in a room as blood and urine tests were processed. “I don’t think Mike knew of the severity of what was coming, but I knew — I saw those five doctors talking in the other room and I started panicking.” One of the doctors returned to explain that Gavin’s blood sugar level was 700 milligrams per deciliter and that it was supposed to be around 100. “There was no outward indication, nothing,” Pierce says of Gavin’s appearance at the time. “He was acting normal — exploring the office, looking at planes out the window. And they were telling us he needed to be admitted.”
At 18 months old, Gavin was one of the youngest people to be diagnosed with type 1 diabetes in San Diego County. Failing to choke back her tears, Pierce weeps openly as she recalls what happened next.
“They were putting an IV in him, and there he was, in his diaper, and they strapped down his arms and legs, and he was crying. The doctor said his blood sugar was so high he could go into diabetic ketoacidosis, which meant he could go into a coma or die. I remember running into the bathroom and throwing up, because I just didn’t know what was going on with my baby.”

“When I have my initial meeting with a family, I have several objectives,” says Dr. Michael Gottschalk, chief of the pediatric endocrinology division at Rady Children’s Hospital. “One is to help them understand the basic physiology of what diabetes means — how blood sugar is regulated, what you need the glucose for, why it’s important — to help them understand what’s going on from a biological point of view. That also then helps segue into what needs to be done in terms of treatment, that we need to replace insulin that the body’s no longer able to make.”
Gavin was admitted, and for the following three days, a physician, nurse, dietician, and endocrinologist set about educating Pierce and her husband.
“They said, ‘Your job as parents is now going to change — you’re not just feeding and clothing your child every day, you now have to keep your child alive every day.’ They told us we’d need to test his blood-sugar level every three hours, and I said, ‘You mean while we’re in the hospital?’ And the doctor said, ‘No. Forever.’ I said, ‘I need to prick my little guy’s fingers every three hours? Every day?’ He has these little tiny fingers, and now there’s a little IV running through his arms, and he’s wearing a little tiny gown; I see this picture in my head of my child — my beautiful, healthy child — and my world has been turned upside down.”
The dietician explained that, from that moment on, every carb the toddler ingested would need to be accounted for.
“I told them, ‘But he’s a baby! What if he drops half a cup of Cheerios? How do I know how many Cheerios dropped?’ And she said, ‘This is going to be the biggest challenge for you.’”
“Families know right away that this is a lifelong situation, that it’s not something that’s going to go away,” says Gottschalk. Most people, upon receiving a life-altering diagnosis, naturally go through a grieving process. Once families begin to learn about managing the disease, Gottschalk says, “the biggest concern almost every parent has is that if the glucose goes too low and is not providing enough energy to the brain, the child can pass out or have a seizure. The parents’ biggest fear is that this might happen in the middle of the night, when the child is sleeping.”
For over two years, Pierce would wake up every three hours to test Gavin’s blood sugar. Now he wears a glucose monitor that sounds an alarm if his levels get too high or low. Pierce describes one recent middle-of-the-night scare. “It was 4 a.m., and his blood sugar was at 80 but falling fast, so Mike ran in and gave him a couple of glucose tablets. He had to wake him up and say, ‘Hey, baby, we need to give you a snack; your blood sugar’s low.’ And Gavin just chews in his sleep. He kind of knows. He’s such a good boy; he never refuses it.” If Gavin’s blood sugar spikes too high in the middle of the night, he needs to be given an injection of insulin.
Gottschalk explains that when a person with type 1 diabetes is replacing insulin, it’s for three reasons: “One, is to provide insulin at the time you’re eating for the glucose derived from carbohydrates in the diet to enter the cells of the body to use as energy. The second reason to take insulin would be any time you have high blood sugar and you want to bring that number down with an immediate infusion of insulin. The third is that, when we’re not eating, we need to continue to supply the bloodstream with glucose as an energy source — there are parts of the body that only use glucose for energy, and the brain is one of them. We store some of that glucose in our liver for later use, and when we’re not eating, the liver pumps glucose back into the blood so there is always a constant supply, either coming from food in our diet or our liver. But the liver left to its own has no self-control. It would pump out glucose all the time. The insulin puts a brake on that. Once you’ve absorbed all that glucose, insulin lets its foot off the brake.”
Pierce and her husband have what they call “carbuments,” a word that is recognized among the type 1 diabetes community, all of whom speak the jargon known as “diabetonese.” These arguments over how to manage their son’s carb intake boils down to two opposing approaches to managing blood-sugar levels: “I would prefer to have Gavin higher because I freak out when he’s low, and my husband prefers him a little bit lower because if you’re high, that can lead to organ failure later on.”
Mr. and Mrs. Pierce have worked hard to overcome the strain Gavin’s illness has put on their relationship.
“We’ve had points where we didn’t know how we were going to make this work,” says Sage Pierce. “When your whole existence as a couple is taking care of your child, your texts to each other are, ‘What’s his number, how many carbs, okay, love you.’ We’ve had a lot of friends, type 1 families, separated or get divorced.”
Approximately three million Americans suffer from type 1 diabetes; 85 percent of them are adults. That amounts to just under 10 percent of all diabetics, the majority of whom are type 2.
“With type 2, you can still make insulin,” Gottschalk explains. “And there are lots of other therapies, a whole variety of pills; even cactus juice can help.”
Gottschalk is careful to warn patients and their families about harmfully inaccurate advice they’re likely to get from family members and friends whose only experience has been with type 2.
“It’s been my experience that once a family gets diagnosed, a relative might say, ‘I had an uncle who drank cactus juice, or ate cinnamon bark, and their diabetes got better. And some of that does work in type 2, but none of it works in type 1. [The two types] may share the same name, but the treatments are significantly different.”
Another misconception, Gottschalk explains, is that years ago, type 1 and 2 were referred to as “juvenile diabetes” and “adult diabetes.” “That’s no longer true,” he says. “Fifty percent of patients develop type 1 before age 18, but a significant portion [the other 50 percent] develop it as adults. Likewise, now there are children who develop type 2. The distinction between children and adults doesn’t exist.”

In January 2014, 30-year-old Victoria Ross went to see her doctor about a persistent sinus infection she’d been battling for two months. She was also preparing for her wedding day.
“I was exercising and dieting like crazy, and losing a lot of weight,” Ross remembers. “I went from a size 13 to a size 5 in, like, three months. I was thinking, Man, this thing’s working, I’m doing something right.” But then coworkers began to make comments. “They were to the effect of, ‘Hey, I know you’re dieting, but I think maybe you should stop; you’re almost losing too much weight.’”
When Ross followed up with her primary doctor about the sinus infection the following month, she mentioned her coworkers’ comments and asked for his opinion. He told her she was still within the healthy range but that he was going to run some tests to be sure. The following day, Ross checked the lab results on the Kaiser Permanente website.
“I’m looking at all these numbers and I don’t know what they are,” she recalls. According to the site, the normal range for blood-glucose levels was 70 to 120. “Mine read 600. I thought maybe they put the decimal in the wrong spot. I called the hospital, hoping someone could explain it to me, but I was told the doctor’s office was closed over the weekend and I’d have to try back on Monday.”
But on Monday, Ross’s primary-care physician called her first. “Once the doctor’s office found out about it, they were really upset that someone didn’t call me right away,” she says. “He said I needed to stop what I was doing immediately and come to the hospital. He said, ‘Don’t drive yourself. I want someone else to drive you in,’ and I was, like, How can I get someone to drive me from Poway to Mission Valley? That’s stupid. So I drove myself.”
Ross then spent “an entire, mortifying, traumatizing day” in the hospital. “I was sitting there with an IV in my arm, starving — I couldn’t eat anything for, like, six hours — to bring my blood sugar down.” She was diagnosed as having type 2 diabetes and was sent home with a prescription for Metformin, a medication used to treat type 2 diabetes. The pill works by reducing liver-produced sugars and dialing up the body’s responsiveness to insulin. But this does nothing for people with type 1 diabetes, who need more insulin. The doctor gave Ross a meter to check her blood level. Later that day, after Ross had had a chance to eat (she went to Souplantation for tomato soup and tuna pasta salad, which she thought at the time was a low-carb meal), her doctor called to ask what her blood sugar level was. “I told him it was almost 300 after I ate, and he said I needed to come back in.”
Back at the hospital for the second time that day, Ross was tested for C-peptide, a protein that is produced along with insulin and used as a marker to determine how much insulin the pancreas is producing. When the results were in, it was determined that type 2 had been a misdiagnosis — Ross had type 1 diabetes.
The doctor told Ross that this new diagnosis meant she couldn’t take the pills he’d prescribed earlier and that she’d need to start injections.
“There was no training, no, ‘Here’s how you do it.’ I was, like, ‘I have to give myself the injection? Where?’ And he said, ‘In the stomach.’” Ross went to the pharmacy and asked for help. “I said, ‘I don’t know how to do this, I’ve never done it, and I have to do it tonight.’ And the pharmacist actually opened the box and unfolded the directions and just read them to me. I was, like, are you kidding me? I’d been at Kaiser for a full 24 hours at this point. My husband, who was my fiancé at the time — you’ve never met a more patient person — he almost totally lost it on the pharmacist. It was pretty upsetting. We took the [insulin] and left.”
Of her husband, Ross says, “It was right before the wedding, and he was kind of overwhelmed by it, thinking, Oh, my God, I don’t know if I can deal with this. He went to counseling before I did.”
Since then, he has been committed to the relationship, and even accompanies Ross to a support group for adults with type 1 diabetes.
When asked the date of her diagnosis, Ross does not hesitate in responding: February 28. She has yet to experience her first “diaversary” but she is aware of the term used by the type 1 diabetes community to refer to the anniversary of the day someone is diagnosed. Gavin’s diaversary is November 14, which happens to fall on World Diabetes Day.

Heidi Calabrese, founder of SDT1D, a Facebook group for type 1 diabetics in San Diego, believes the diaversary is something to celebrate.
“We joke about it and say, ‘This is how many years we’ve been giving diabetes the finger,’” she says. On his diaversary each year, Calabrese’s eight-year-old son Andrew, who was diagnosed in 2010, receives a gift and gets to pick the restaurant the family will dine at that night.
“I know for a lot of parents, it’s hard for them. They were in tears. For us, it’s definitely a day of reflection and also a day to celebrate how long we’ve stayed on top of this; like, let’s look at the fact that we’re extremely fortunate we’ve had our son alive for four more years.”
Though Pierce provided Gavin with his favorite movie and dinner (Wreck It Ralph and pizza) to celebrate his third diaversary, she prefers to not remember that harrowing diagnosis day. In retrospect, she is grateful for the support she received from the Rady Children’s Hospital staff. Unlike Ross, who was initially misdiagnosed and then later left to fend for herself, Sage Pierce and her husband were extensively trained. The family was not released until the staff was confident that Gavin’s parents were capable of caring for him.
“The hardest part in the hospital was the second day when the nurse said, ‘We’re not giving the shots anymore, you are,” Pierce recalls. “I couldn’t do it. I was scared. I saw his little thighs and said, ‘I can’t put that in there.’”
It was five months before Sage Pierce began to feel comfortable giving Gavin his injections. Her husband handled the shots for their first week at home until, finally, the night came when he was out and she had to do it herself.
“I felt like a drug dealer. You’re exhausted, emotional, and trying to pull exactly 4.5 units while your hands are shaking, and thinking, Oh, my God, if I’m off by half a unit it could send him too low. I’d have to hold him down to give him a shot and he’s screaming, ‘Why, Mommy, why!’ and you just want to cry, and I say, ‘Because, honey, we love you, and you have diabetes, and this is your medicine.’”
From her struggles, Pierce has taken away one realization: “I have more strength than I ever thought I could. There’s nothing I wouldn’t do for Gavin. If I could give him my pancreas, I would. But that’s not possible.”
The father of a child with Type 1 diabetes installs a new blood glucose monitor on his son's arm as part of a diabetes management program that keeps him alive.
Gavin wears a continuous glucose monitor manufactured by Dexcom, Inc., which is headquartered in San Diego. The adhesive patch on the back of his arm is used to hold his monitor’s sensor (a small wire inserted into the skin) in place. The wire reads his glucose levels and relays that information to the attached transmitter, which is then picked up on the receiver, a phone-sized device that Gavin carries around with him in his fanny pack. The Dexcom sends a reading every five minutes, which Pierce says is “handy, because you might not know when you’re dropping or getting too high until it’s too late.” It is the receiver that sounds the alarm if his blood sugar levels are rising or falling too fast.
A group of “D-dads” (fathers of children with diabetes) recently came together to hack and reverse-engineer continuous glucose monitors so that they could monitor their kids’ glucose levels remotely. They created a hashtag, #WeAreNotWaiting, to develop and share a new open-source app called Nightscout, also known as CGM — for continuous glucose monitoring — in the Cloud.

Calabrese’s husband, Jason, is a software developer who does coding for Nightscout in his spare time. “Parents were tired of waiting on the FDA and on companies that are making this type of thing, so they took it upon themselves to create something for personal use,” Calabrese says. When sharing a story about these D-dads on Facebook, Pierce commented, “Who needs governmental agencies when tech-savvy parents, working to keep their children alive and healthy, put their brains together!”
The Facebook group CGMintheCloud, where people go to ask questions and help others with the app, currently has around 8500 members. “The great thing about this community is there’s a lot of support — if someone has a problem, they can post it and people respond immediately with help. It’s very do-it-yourself,” says Calabrese.
It was Jason Calabrese who helped the Pierces set up Nightscout so that Sage and Mike could monitor their son’s blood sugar remotely. After posting in the Facebook group that he was considering the software, Mike received a message from Jason, who provided information on where to go for a discount and then walked him through the setup via Facebook messenger.
This recent development — being able to check on her son from afar — has been a major source of relief for Sage Pierce. “I’ll be at work, in a meeting, and I just click on Nightscout on my phone and be, like, Okay, good, he’s all right. And at night, instead of having to run from the bedroom to look at his Dexcom, we can look from our phone.” Mike can access Gavin’s numbers from the Pebble watch on his wrist.
But this constant awareness has a dark side. On November 4, ten days before Gavin’s diaversary, the Pierces were in the hospital without him, bringing Gavin’s baby sister, Gianna, into the world. Sage Pierce’s parents were staying home with Gavin. In the middle of the night, while she was awake with her newborn in her arms, Pierce checked Nightscout and saw that Gavin’s blood sugar was dropping fast.
“He was at, like, 50, and my mom and dad were there, but neither of them were answering their phone. I called the house phone, but they don’t even know where it’s kept. I was freaking out. I said, ‘Mike, what are we going to do? I think you need to drive home.’”
Sage was about to call the police and ask them to go to the house when her mother finally texted that she’d caught the drop and had already “carbed” Gavin. “I was sitting there in the hospital ready to rip out my hair. My parents just aren’t up to speed on their texting.”
When babysitting Gavin, Sage’s mother sets her alarm every two hours so that she is sure to wake up and check his numbers. On the night of this scare, Gavin’s blood sugar crashed between her alarms.
All around the house are reminders of Gavin’s condition. There is a display monitor for Nightscout on a bookshelf in the living room and another, on an iPad, in the kitchen. In the fridge are insulin bottles cased in individual cozies (they prevent the glass from breaking if they fall). On one counter is what looks like a plastic cooler with a red and yellow biohazard warning on the side; this is the receptacle for used needles and test strips. A medical supply drawer contains test strips, Dexom inserts, a collection of the tablet candy Smarties, and tubes of cake-decorating gel. When Gavin’s blood sugar dips too low, giving him juice or tablets would mean 15 minutes of waiting for the number to rise; whereas something extra sugary, such as the cake-decorating gel, is faster acting. “If he’s at 50 or 60 and sleeping, we’ll just squirt this in his mouth and it takes about five minutes,” Pierce says.
The drawer also contains an item Pierce hopes she never has to use — the glucagon shot. A peptide hormone produced by the pancreas, glucagon is insulin’s opposite, in that it increases, rather than decreases the concentration of sugar in the bloodstream. Pierce explains, “If he’s passed out and we can’t wake him up, we open this, we pop the syringe and give it to him and then call 911.”
Though much of Gavin’s treatment is covered by insurance, there are significant out-of-pocket expenses in the management of type 1 diabetes, especially because many of the newer technologies are not yet covered. The Dexcom itself cost $300, which is a one-time fee, but the sensor must be regularly replaced. The $40 piece is supposed to last a week, but on an active four-year-old, that is reduced to closer to three or four days. Doctor visit copays are $35 and a urinalysis can be up to $300. Add in things such as insulin vials ($60 each), syringes, and lancets, and Pierce estimates she spends about $1300 a month “just on diabetes.”
It could be said that Gavin’s young age at the time of diagnosis gives him an advantage, in that he has never known life to be any other way. Pierce says, “I think it’s harder for kids diagnosed at eight or nine, who have been living without all that stuff; that’s a huge change. But when you’re diagnosed younger, this is what they’re used to. It makes me wonder if Gavin thinks every kid has type 1.”
After 30 years of relatively good health, Ross, now 31, is still struggling adjust. “It touches every single part of your life; you don’t realize it,” she says. “If I don’t get enough sleep, the sugars run high; if it’s that time of the month, the sugars run high; being sick, having an infection, varying from the routine, it all has an impact. If I want to sleep in on Saturday, but then sleep in too much, my sugar can go too low.”
Ross says she suffers a tremendous feeling of loss for her former life. “All my thoughts come back to the same thing — I wish I could have the life I had before, I wish I could sleep in, I wish I didn’t have to give myself injections, I wish I could just sit down for a meal at a restaurant without having to go to the bathroom to take a shot — you can’t take it when you order because you don’t know how long it will take for the food to arrive on the table, and by the time I come back, usually the people I’m eating with are, like, halfway done.”
Receiving a diagnosis for a life-threatening disease can be isolating, especially when that disease is misunderstood. When Ross first told friends about her condition, they often responded by saying, “But you don’t look like a diabetic.” At first, Ross would explain, “It’s not curable, not something that can be fixed with behavior — it’s something that happens. It’s an immune problem, and no amount of diet or exercise will change that.”
But she soon began to tire of educating everyone around her. “It just makes me sad that people are not aware. Now I kind of ignore the comments. They just don’t understand.” Left to “flounder” for a few weeks before being enrolled in a diabetes class at Kaiser, Ross took it upon herself to self-educate and found the San Diego chapter of the Juvenile Diabetes Research Foundation, which is the world’s largest organization dedicated to funding type 1 diabetes research. It was there she found and joined the support group, ACT-1 (Adults Conquering Type 1).
“Because type 1 is rare, you don’t run into people who deal with the exact same things we deal with all the time. You just want to feel normal,” Ross explains. “When you go to those meetings and talk to these people and they tell you that you’re normal, you are okay.”
Pierce, who is now a mentor with the foundation, was introduced to the organization while Gavin was still in the hospital. One of the programs they offer is the Bag of Hope.
“It provides a newly diagnosed family with a backpack full of information about type 1 — what it is, what this means for you and your child moving forward,” says Sean McParland, executive director of the foundation’s San Diego chapter. One item in the Bag of Hope is a teddy bear on which children can practice giving injections. For anyone newly diagnosed over 18, the foundation provides an adult tool kit.
“But it’s more than what’s in the bag,” McParland continues. “It’s really the connection to the greater type 1 community.”
The primary reason most people contact the organization is for the mentor program.
“If your three-year-old is diagnosed, we can match you up with another parent who’s been living this life for a number of years, whose child was also diagnosed when they were three.”
Just as she was helped, Pierce now assists other parents with everything from how to handle the realities of snack time at preschool to dealing with the potential sugar crash that can occur after a tantrum. McParland says, “The psychosocial component is so important — to get support from actual people living the life, who have met a lot of these challenges already in their own home.”
At a recent event organized by volunteers at a park in El Cajon, McParland witnessed the benefit of the community coming together.
“There were about 20 people there, and I was on a picnic bench, and this little six-year-old girl came over and she had just met this four-year-old girl.” McParland was sitting beside the four-year-old’s mother, who had called her daughter over because it was time for an injection. When she saw her new friend receiving the shot, the six-year-old said, “‘Oh, you do needles?’ Then the six-year-old pulled up her shirt and revealed her insulin pump. It was pink and decked out with little pink plastic things that looked like diamonds. The four-year-old was, like, what’s that? And the six-year-old started explaining. It made it that much easier for the younger girl’s mom when the time came if she wanted to switch her daughter to the pump.”
When Gavin was diagnosed, one of Sage Pierce’s first requests was to see older children surviving and thriving with type 1.
“There was a woman who was 25 and had had type 1 diabetes for nine or ten years, and I asked if I could meet her,” she remembers. “I just wanted to see her; like, is she okay? What does she look like? Is she normal? I felt so much better when I saw her pump, and she told me she’d just been hiking. A lot of parents — you can hear it in their voice when they’re panicking — they just want to know their kids will be able to reach for their dreams.”
When Pierce is meeting with a family that has a newly diagnosed loved one, she reassures them that it will get easier. “Now it seems like you want to call the doctor for everything, but the more you manage this and learn,” she says, “you’re going to become your child’s doctor, and nurse and dietician and endocrinologist.”
Though Pierce seems to find this empowering, for Ross, being her own doctor is a source of frustration.
“The doctor just says, ‘Here’s a general guideline, and you figure out the dosing from there,’” she says.
Mary Tyler Moore, who was diagnosed with type 1 diabetes at age 34, and who currently serves as international chairman for the Juvenile Diabetes Research Foundation, can relate. She is quoted on the organization’s site: “Both children and adults like me who live with type 1 diabetes need to be mathematicians, physicians, personal trainers, and dietitians all rolled into one. We need to be constantly factoring and adjusting, making frequent finger sticks to check blood sugars, and giving ourselves multiple daily insulin injections just to stay alive.”
As the largest charitable supporter of type 1 diabetes research, the foundation is currently sponsoring $568 million in charitable research in 17 countries. This may seem like a lot, until one considers the fact that the average cost of bringing a new drug to market is $1.3 billion (according to the Tufts Center for the Study of Drug Development).
“People have told me they may be leaving the world of type 1 diabetes research and going into other research because there’s just no funding to keep it going, and clinical trials are very expensive,” says McParland.
The research for a cure focuses on two main approaches: cell-replacement therapy and an artificial pancreas. The problem with cell-replacement therapy is that regardless of how many new beta cells are added, the immune system of a person with type 1 diabetes would still attack and kill them. However, the Juvenile Diabetes Research Foundation has partnered with a company that may have overcome this obstacle. In November 2014, San Diego–based ViaCyte, Inc., a regenerative medicine company, began experimental treatments at University of California San Diego using its proprietary encapsulated cell-replacement therapy.
McParland likens ViaCyte’s encapsulation device to shark-proof cages used by underwater photographers.
“If the photographer is in that cage, he can take photos but the sharks can’t get to him.” Similarly, the encapsulation device is designed to contain insulin-producing beta cells and allow the insulin to be released into the body, all while protecting the beta cells from the body’s immune system. “It’s a pretty revolutionary concept that has been on the drawing board for a long time and now, for the first time, is being tested on people.”
Pierce and Calabrese do their best to keep up with the advances toward a cure. In the meantime, they, along with every other person whose life has been affected by type 1 diabetes, want people to understand not only the severity of the disease, but how different it is from type 2.
“There is so much confusion out there,” says Calabrese. “My son didn’t develop this because we fed him Twinkies and Coke. And he may look like any healthy kid, but if he gets too much insulin, he could pass out or have a seizure or die.”
Sage Pierce wants other parents to realize that any child can contract this disease.
“This can hit anytime, and we don’t know what causes it,” she says. “We don’t have any type 1 in the family, but we have Parkinson’s and arthritis. Some people say it’s environmental. There are all these theories and not one reason. If you study up, you’ll see that in the past couple of years, more and more Caucasians are being diagnosed with type 1. What if it’s something from plastics or something in our food? Who knows? You hope that none of your friends’ kids get it, but in the back of your mind, you know if it happened to your son, it can happen to anyone.”


On a sunny morning in Poway, a little boy named Gavin scampers around his backyard as his mother looks on. To the unassuming eye, this lean, blue-eyed towhead looks like any other fit four-year-old. But upon closer inspection, one might notice the sun glinting off his small silver anklet; when Gavin clambers up the side of his wooden play set, a white adhesive bandage can be seen on the back of his arm; as he wriggles his way down the plastic slide, his shirt rides up, revealing a tiny fanny pack around his waist. Each item is part of a collection of equipment that helps keep Gavin alive.

Gavin has type 1 diabetes. Unlike type 2, a metabolic disorder often related to poor diet and lack of exercise, type 1 is an autoimmune disease. There is no cure and no known way to prevent it. Nor is there a way to predict who will get it or when. “Gavin was a healthy, thriving baby,” says Sage Pierce, Gavin’s mother. “I breastfed him until he was a year old and then fed him organic baby food. He was a pretty darn healthy kid — no colds, no ear infections, nothing.”

When Gavin was 14 months old, Pierce started noticing “weird” things. “He would wake up in the morning and his lips would be blue.” When she asked her pediatrician about this, she was told her son might be cold in the morning. A few months later, Gavin began wetting his diaper three or four times a night. “Like, dripping wet, we’d have to change the sheets,” Pierce remembers. “I thought, Is this normal? I’m a new parent, I have no idea.” The doctor recommended larger diapers.
Commonly referred to as T1D, type 1 diabetes lies dormant until it is triggered, most often by something as simple as a cold. When we get sick, our immune system responds by leaping into action and killing the invading cells. For people with type 1 diabetes, this process malfunctions and the immune system targets, attacks, and kills crucial beta cells, which are the only cells in our bodies that create insulin, the hormone that delivers the precious energy source, glucose (i.e., sugar), to the cells. Without insulin, glucose builds up in the blood, depriving most cells and organs in the body of the energy they need to continue functioning. As a result, the body believes it is starving and begins processing fat for fuel, which creates acidic biproducts known as ketones. As these ketones build up, the body tries to rid itself of the extra toxins, primarily through urine. If the level of ketones gets too high, the consequences are dire: one could fall into a diabetic coma, or die.
What Pierce did not know at the time, was that Gavin was exhibiting the most common symptom of life-threateningly high blood sugar: excessive thirst, followed by frequent urination. The disease itself (technically known as diabetes mellitus) is named after this symptom. Diabetes comes from the Greek word for “siphon,” and mellitus from the Latin word for “honey.” In China, diabetes was dubbed the “sweet urine disease” after it was observed that sugar-loving insects such as ants were attracted to some people’s urine.
When Gavin was 18 months old, he traveled with his family to Detroit for a wedding and caught a terrible cold. Upon returning home, he was constantly thirsty. “He’d drink a whole sippy cup and then ask for another one,” Pierce says. “It got to the point where I emailed the doctor and said, ‘Something’s not right.’ We brought him in for blood tests on a Friday, when there weren’t any doctors, just the lab, and then we went home for the weekend, like it was no big deal.”
On Monday, November 14, 2011, Pierce received a call on her cell phone while she was at work. It was a nurse, informing her that Gavin’s test results indicated he was diabetic and she needed to bring him to Rady Children’s Hospital immediately.
Pierce, an executive producer for NBC San Diego, recalls that moment.
“I was sitting there in the newsroom, like, what? In my mind, diabetes meant type 2 — my grandmother died of type 2. I was, like, This kid’s skinny, he eats healthy, what the hell? My stomach was just falling and I was crying at my desk. I called my husband, and he didn’t even know type 1 was a thing.”
At the hospital, Pierce, her husband Mike, and Gavin sat in a room as blood and urine tests were processed. “I don’t think Mike knew of the severity of what was coming, but I knew — I saw those five doctors talking in the other room and I started panicking.” One of the doctors returned to explain that Gavin’s blood sugar level was 700 milligrams per deciliter and that it was supposed to be around 100. “There was no outward indication, nothing,” Pierce says of Gavin’s appearance at the time. “He was acting normal — exploring the office, looking at planes out the window. And they were telling us he needed to be admitted.”
At 18 months old, Gavin was one of the youngest people to be diagnosed with type 1 diabetes in San Diego County. Failing to choke back her tears, Pierce weeps openly as she recalls what happened next.
“They were putting an IV in him, and there he was, in his diaper, and they strapped down his arms and legs, and he was crying. The doctor said his blood sugar was so high he could go into diabetic ketoacidosis, which meant he could go into a coma or die. I remember running into the bathroom and throwing up, because I just didn’t know what was going on with my baby.”

“When I have my initial meeting with a family, I have several objectives,” says Dr. Michael Gottschalk, chief of the pediatric endocrinology division at Rady Children’s Hospital. “One is to help them understand the basic physiology of what diabetes means — how blood sugar is regulated, what you need the glucose for, why it’s important — to help them understand what’s going on from a biological point of view. That also then helps segue into what needs to be done in terms of treatment, that we need to replace insulin that the body’s no longer able to make.”
Gavin was admitted, and for the following three days, a physician, nurse, dietician, and endocrinologist set about educating Pierce and her husband.
“They said, ‘Your job as parents is now going to change — you’re not just feeding and clothing your child every day, you now have to keep your child alive every day.’ They told us we’d need to test his blood-sugar level every three hours, and I said, ‘You mean while we’re in the hospital?’ And the doctor said, ‘No. Forever.’ I said, ‘I need to prick my little guy’s fingers every three hours? Every day?’ He has these little tiny fingers, and now there’s a little IV running through his arms, and he’s wearing a little tiny gown; I see this picture in my head of my child — my beautiful, healthy child — and my world has been turned upside down.”
The dietician explained that, from that moment on, every carb the toddler ingested would need to be accounted for.
“I told them, ‘But he’s a baby! What if he drops half a cup of Cheerios? How do I know how many Cheerios dropped?’ And she said, ‘This is going to be the biggest challenge for you.’”
“Families know right away that this is a lifelong situation, that it’s not something that’s going to go away,” says Gottschalk. Most people, upon receiving a life-altering diagnosis, naturally go through a grieving process. Once families begin to learn about managing the disease, Gottschalk says, “the biggest concern almost every parent has is that if the glucose goes too low and is not providing enough energy to the brain, the child can pass out or have a seizure. The parents’ biggest fear is that this might happen in the middle of the night, when the child is sleeping.”
For over two years, Pierce would wake up every three hours to test Gavin’s blood sugar. Now he wears a glucose monitor that sounds an alarm if his levels get too high or low. Pierce describes one recent middle-of-the-night scare. “It was 4 a.m., and his blood sugar was at 80 but falling fast, so Mike ran in and gave him a couple of glucose tablets. He had to wake him up and say, ‘Hey, baby, we need to give you a snack; your blood sugar’s low.’ And Gavin just chews in his sleep. He kind of knows. He’s such a good boy; he never refuses it.” If Gavin’s blood sugar spikes too high in the middle of the night, he needs to be given an injection of insulin.
Gottschalk explains that when a person with type 1 diabetes is replacing insulin, it’s for three reasons: “One, is to provide insulin at the time you’re eating for the glucose derived from carbohydrates in the diet to enter the cells of the body to use as energy. The second reason to take insulin would be any time you have high blood sugar and you want to bring that number down with an immediate infusion of insulin. The third is that, when we’re not eating, we need to continue to supply the bloodstream with glucose as an energy source — there are parts of the body that only use glucose for energy, and the brain is one of them. We store some of that glucose in our liver for later use, and when we’re not eating, the liver pumps glucose back into the blood so there is always a constant supply, either coming from food in our diet or our liver. But the liver left to its own has no self-control. It would pump out glucose all the time. The insulin puts a brake on that. Once you’ve absorbed all that glucose, insulin lets its foot off the brake.”
Pierce and her husband have what they call “carbuments,” a word that is recognized among the type 1 diabetes community, all of whom speak the jargon known as “diabetonese.” These arguments over how to manage their son’s carb intake boils down to two opposing approaches to managing blood-sugar levels: “I would prefer to have Gavin higher because I freak out when he’s low, and my husband prefers him a little bit lower because if you’re high, that can lead to organ failure later on.”
Mr. and Mrs. Pierce have worked hard to overcome the strain Gavin’s illness has put on their relationship.
“We’ve had points where we didn’t know how we were going to make this work,” says Sage Pierce. “When your whole existence as a couple is taking care of your child, your texts to each other are, ‘What’s his number, how many carbs, okay, love you.’ We’ve had a lot of friends, type 1 families, separated or get divorced.”
Approximately three million Americans suffer from type 1 diabetes; 85 percent of them are adults. That amounts to just under 10 percent of all diabetics, the majority of whom are type 2.
“With type 2, you can still make insulin,” Gottschalk explains. “And there are lots of other therapies, a whole variety of pills; even cactus juice can help.”
Gottschalk is careful to warn patients and their families about harmfully inaccurate advice they’re likely to get from family members and friends whose only experience has been with type 2.
“It’s been my experience that once a family gets diagnosed, a relative might say, ‘I had an uncle who drank cactus juice, or ate cinnamon bark, and their diabetes got better. And some of that does work in type 2, but none of it works in type 1. [The two types] may share the same name, but the treatments are significantly different.”
Another misconception, Gottschalk explains, is that years ago, type 1 and 2 were referred to as “juvenile diabetes” and “adult diabetes.” “That’s no longer true,” he says. “Fifty percent of patients develop type 1 before age 18, but a significant portion [the other 50 percent] develop it as adults. Likewise, now there are children who develop type 2. The distinction between children and adults doesn’t exist.”

In January 2014, 30-year-old Victoria Ross went to see her doctor about a persistent sinus infection she’d been battling for two months. She was also preparing for her wedding day.
“I was exercising and dieting like crazy, and losing a lot of weight,” Ross remembers. “I went from a size 13 to a size 5 in, like, three months. I was thinking, Man, this thing’s working, I’m doing something right.” But then coworkers began to make comments. “They were to the effect of, ‘Hey, I know you’re dieting, but I think maybe you should stop; you’re almost losing too much weight.’”
When Ross followed up with her primary doctor about the sinus infection the following month, she mentioned her coworkers’ comments and asked for his opinion. He told her she was still within the healthy range but that he was going to run some tests to be sure. The following day, Ross checked the lab results on the Kaiser Permanente website.
“I’m looking at all these numbers and I don’t know what they are,” she recalls. According to the site, the normal range for blood-glucose levels was 70 to 120. “Mine read 600. I thought maybe they put the decimal in the wrong spot. I called the hospital, hoping someone could explain it to me, but I was told the doctor’s office was closed over the weekend and I’d have to try back on Monday.”
But on Monday, Ross’s primary-care physician called her first. “Once the doctor’s office found out about it, they were really upset that someone didn’t call me right away,” she says. “He said I needed to stop what I was doing immediately and come to the hospital. He said, ‘Don’t drive yourself. I want someone else to drive you in,’ and I was, like, How can I get someone to drive me from Poway to Mission Valley? That’s stupid. So I drove myself.”
Ross then spent “an entire, mortifying, traumatizing day” in the hospital. “I was sitting there with an IV in my arm, starving — I couldn’t eat anything for, like, six hours — to bring my blood sugar down.” She was diagnosed as having type 2 diabetes and was sent home with a prescription for Metformin, a medication used to treat type 2 diabetes. The pill works by reducing liver-produced sugars and dialing up the body’s responsiveness to insulin. But this does nothing for people with type 1 diabetes, who need more insulin. The doctor gave Ross a meter to check her blood level. Later that day, after Ross had had a chance to eat (she went to Souplantation for tomato soup and tuna pasta salad, which she thought at the time was a low-carb meal), her doctor called to ask what her blood sugar level was. “I told him it was almost 300 after I ate, and he said I needed to come back in.”
Back at the hospital for the second time that day, Ross was tested for C-peptide, a protein that is produced along with insulin and used as a marker to determine how much insulin the pancreas is producing. When the results were in, it was determined that type 2 had been a misdiagnosis — Ross had type 1 diabetes.
The doctor told Ross that this new diagnosis meant she couldn’t take the pills he’d prescribed earlier and that she’d need to start injections.
“There was no training, no, ‘Here’s how you do it.’ I was, like, ‘I have to give myself the injection? Where?’ And he said, ‘In the stomach.’” Ross went to the pharmacy and asked for help. “I said, ‘I don’t know how to do this, I’ve never done it, and I have to do it tonight.’ And the pharmacist actually opened the box and unfolded the directions and just read them to me. I was, like, are you kidding me? I’d been at Kaiser for a full 24 hours at this point. My husband, who was my fiancé at the time — you’ve never met a more patient person — he almost totally lost it on the pharmacist. It was pretty upsetting. We took the [insulin] and left.”
Of her husband, Ross says, “It was right before the wedding, and he was kind of overwhelmed by it, thinking, Oh, my God, I don’t know if I can deal with this. He went to counseling before I did.”
Since then, he has been committed to the relationship, and even accompanies Ross to a support group for adults with type 1 diabetes.
When asked the date of her diagnosis, Ross does not hesitate in responding: February 28. She has yet to experience her first “diaversary” but she is aware of the term used by the type 1 diabetes community to refer to the anniversary of the day someone is diagnosed. Gavin’s diaversary is November 14, which happens to fall on World Diabetes Day.

Heidi Calabrese, founder of SDT1D, a Facebook group for type 1 diabetics in San Diego, believes the diaversary is something to celebrate.
“We joke about it and say, ‘This is how many years we’ve been giving diabetes the finger,’” she says. On his diaversary each year, Calabrese’s eight-year-old son Andrew, who was diagnosed in 2010, receives a gift and gets to pick the restaurant the family will dine at that night.
“I know for a lot of parents, it’s hard for them. They were in tears. For us, it’s definitely a day of reflection and also a day to celebrate how long we’ve stayed on top of this; like, let’s look at the fact that we’re extremely fortunate we’ve had our son alive for four more years.”
Though Pierce provided Gavin with his favorite movie and dinner (Wreck It Ralph and pizza) to celebrate his third diaversary, she prefers to not remember that harrowing diagnosis day. In retrospect, she is grateful for the support she received from the Rady Children’s Hospital staff. Unlike Ross, who was initially misdiagnosed and then later left to fend for herself, Sage Pierce and her husband were extensively trained. The family was not released until the staff was confident that Gavin’s parents were capable of caring for him.
“The hardest part in the hospital was the second day when the nurse said, ‘We’re not giving the shots anymore, you are,” Pierce recalls. “I couldn’t do it. I was scared. I saw his little thighs and said, ‘I can’t put that in there.’”
It was five months before Sage Pierce began to feel comfortable giving Gavin his injections. Her husband handled the shots for their first week at home until, finally, the night came when he was out and she had to do it herself.
“I felt like a drug dealer. You’re exhausted, emotional, and trying to pull exactly 4.5 units while your hands are shaking, and thinking, Oh, my God, if I’m off by half a unit it could send him too low. I’d have to hold him down to give him a shot and he’s screaming, ‘Why, Mommy, why!’ and you just want to cry, and I say, ‘Because, honey, we love you, and you have diabetes, and this is your medicine.’”
From her struggles, Pierce has taken away one realization: “I have more strength than I ever thought I could. There’s nothing I wouldn’t do for Gavin. If I could give him my pancreas, I would. But that’s not possible.”
The father of a child with Type 1 diabetes installs a new blood glucose monitor on his son's arm as part of a diabetes management program that keeps him alive.
Gavin wears a continuous glucose monitor manufactured by Dexcom, Inc., which is headquartered in San Diego. The adhesive patch on the back of his arm is used to hold his monitor’s sensor (a small wire inserted into the skin) in place. The wire reads his glucose levels and relays that information to the attached transmitter, which is then picked up on the receiver, a phone-sized device that Gavin carries around with him in his fanny pack. The Dexcom sends a reading every five minutes, which Pierce says is “handy, because you might not know when you’re dropping or getting too high until it’s too late.” It is the receiver that sounds the alarm if his blood sugar levels are rising or falling too fast.
A group of “D-dads” (fathers of children with diabetes) recently came together to hack and reverse-engineer continuous glucose monitors so that they could monitor their kids’ glucose levels remotely. They created a hashtag, #WeAreNotWaiting, to develop and share a new open-source app called Nightscout, also known as CGM — for continuous glucose monitoring — in the Cloud.

Calabrese’s husband, Jason, is a software developer who does coding for Nightscout in his spare time. “Parents were tired of waiting on the FDA and on companies that are making this type of thing, so they took it upon themselves to create something for personal use,” Calabrese says. When sharing a story about these D-dads on Facebook, Pierce commented, “Who needs governmental agencies when tech-savvy parents, working to keep their children alive and healthy, put their brains together!”
The Facebook group CGMintheCloud, where people go to ask questions and help others with the app, currently has around 8500 members. “The great thing about this community is there’s a lot of support — if someone has a problem, they can post it and people respond immediately with help. It’s very do-it-yourself,” says Calabrese.
It was Jason Calabrese who helped the Pierces set up Nightscout so that Sage and Mike could monitor their son’s blood sugar remotely. After posting in the Facebook group that he was considering the software, Mike received a message from Jason, who provided information on where to go for a discount and then walked him through the setup via Facebook messenger.
This recent development — being able to check on her son from afar — has been a major source of relief for Sage Pierce. “I’ll be at work, in a meeting, and I just click on Nightscout on my phone and be, like, Okay, good, he’s all right. And at night, instead of having to run from the bedroom to look at his Dexcom, we can look from our phone.” Mike can access Gavin’s numbers from the Pebble watch on his wrist.
But this constant awareness has a dark side. On November 4, ten days before Gavin’s diaversary, the Pierces were in the hospital without him, bringing Gavin’s baby sister, Gianna, into the world. Sage Pierce’s parents were staying home with Gavin. In the middle of the night, while she was awake with her newborn in her arms, Pierce checked Nightscout and saw that Gavin’s blood sugar was dropping fast.
“He was at, like, 50, and my mom and dad were there, but neither of them were answering their phone. I called the house phone, but they don’t even know where it’s kept. I was freaking out. I said, ‘Mike, what are we going to do? I think you need to drive home.’”
Sage was about to call the police and ask them to go to the house when her mother finally texted that she’d caught the drop and had already “carbed” Gavin. “I was sitting there in the hospital ready to rip out my hair. My parents just aren’t up to speed on their texting.”
When babysitting Gavin, Sage’s mother sets her alarm every two hours so that she is sure to wake up and check his numbers. On the night of this scare, Gavin’s blood sugar crashed between her alarms.
All around the house are reminders of Gavin’s condition. There is a display monitor for Nightscout on a bookshelf in the living room and another, on an iPad, in the kitchen. In the fridge are insulin bottles cased in individual cozies (they prevent the glass from breaking if they fall). On one counter is what looks like a plastic cooler with a red and yellow biohazard warning on the side; this is the receptacle for used needles and test strips. A medical supply drawer contains test strips, Dexom inserts, a collection of the tablet candy Smarties, and tubes of cake-decorating gel. When Gavin’s blood sugar dips too low, giving him juice or tablets would mean 15 minutes of waiting for the number to rise; whereas something extra sugary, such as the cake-decorating gel, is faster acting. “If he’s at 50 or 60 and sleeping, we’ll just squirt this in his mouth and it takes about five minutes,” Pierce says.
The drawer also contains an item Pierce hopes she never has to use — the glucagon shot. A peptide hormone produced by the pancreas, glucagon is insulin’s opposite, in that it increases, rather than decreases the concentration of sugar in the bloodstream. Pierce explains, “If he’s passed out and we can’t wake him up, we open this, we pop the syringe and give it to him and then call 911.”
Though much of Gavin’s treatment is covered by insurance, there are significant out-of-pocket expenses in the management of type 1 diabetes, especially because many of the newer technologies are not yet covered. The Dexcom itself cost $300, which is a one-time fee, but the sensor must be regularly replaced. The $40 piece is supposed to last a week, but on an active four-year-old, that is reduced to closer to three or four days. Doctor visit copays are $35 and a urinalysis can be up to $300. Add in things such as insulin vials ($60 each), syringes, and lancets, and Pierce estimates she spends about $1300 a month “just on diabetes.”
It could be said that Gavin’s young age at the time of diagnosis gives him an advantage, in that he has never known life to be any other way. Pierce says, “I think it’s harder for kids diagnosed at eight or nine, who have been living without all that stuff; that’s a huge change. But when you’re diagnosed younger, this is what they’re used to. It makes me wonder if Gavin thinks every kid has type 1.”
After 30 years of relatively good health, Ross, now 31, is still struggling adjust. “It touches every single part of your life; you don’t realize it,” she says. “If I don’t get enough sleep, the sugars run high; if it’s that time of the month, the sugars run high; being sick, having an infection, varying from the routine, it all has an impact. If I want to sleep in on Saturday, but then sleep in too much, my sugar can go too low.”
Ross says she suffers a tremendous feeling of loss for her former life. “All my thoughts come back to the same thing — I wish I could have the life I had before, I wish I could sleep in, I wish I didn’t have to give myself injections, I wish I could just sit down for a meal at a restaurant without having to go to the bathroom to take a shot — you can’t take it when you order because you don’t know how long it will take for the food to arrive on the table, and by the time I come back, usually the people I’m eating with are, like, halfway done.”
Receiving a diagnosis for a life-threatening disease can be isolating, especially when that disease is misunderstood. When Ross first told friends about her condition, they often responded by saying, “But you don’t look like a diabetic.” At first, Ross would explain, “It’s not curable, not something that can be fixed with behavior — it’s something that happens. It’s an immune problem, and no amount of diet or exercise will change that.”
But she soon began to tire of educating everyone around her. “It just makes me sad that people are not aware. Now I kind of ignore the comments. They just don’t understand.” Left to “flounder” for a few weeks before being enrolled in a diabetes class at Kaiser, Ross took it upon herself to self-educate and found the San Diego chapter of the Juvenile Diabetes Research Foundation, which is the world’s largest organization dedicated to funding type 1 diabetes research. It was there she found and joined the support group, ACT-1 (Adults Conquering Type 1).
“Because type 1 is rare, you don’t run into people who deal with the exact same things we deal with all the time. You just want to feel normal,” Ross explains. “When you go to those meetings and talk to these people and they tell you that you’re normal, you are okay.”
Pierce, who is now a mentor with the foundation, was introduced to the organization while Gavin was still in the hospital. One of the programs they offer is the Bag of Hope.
“It provides a newly diagnosed family with a backpack full of information about type 1 — what it is, what this means for you and your child moving forward,” says Sean McParland, executive director of the foundation’s San Diego chapter. One item in the Bag of Hope is a teddy bear on which children can practice giving injections. For anyone newly diagnosed over 18, the foundation provides an adult tool kit.
“But it’s more than what’s in the bag,” McParland continues. “It’s really the connection to the greater type 1 community.”
The primary reason most people contact the organization is for the mentor program.
“If your three-year-old is diagnosed, we can match you up with another parent who’s been living this life for a number of years, whose child was also diagnosed when they were three.”
Just as she was helped, Pierce now assists other parents with everything from how to handle the realities of snack time at preschool to dealing with the potential sugar crash that can occur after a tantrum. McParland says, “The psychosocial component is so important — to get support from actual people living the life, who have met a lot of these challenges already in their own home.”
At a recent event organized by volunteers at a park in El Cajon, McParland witnessed the benefit of the community coming together.
“There were about 20 people there, and I was on a picnic bench, and this little six-year-old girl came over and she had just met this four-year-old girl.” McParland was sitting beside the four-year-old’s mother, who had called her daughter over because it was time for an injection. When she saw her new friend receiving the shot, the six-year-old said, “‘Oh, you do needles?’ Then the six-year-old pulled up her shirt and revealed her insulin pump. It was pink and decked out with little pink plastic things that looked like diamonds. The four-year-old was, like, what’s that? And the six-year-old started explaining. It made it that much easier for the younger girl’s mom when the time came if she wanted to switch her daughter to the pump.”
When Gavin was diagnosed, one of Sage Pierce’s first requests was to see older children surviving and thriving with type 1.
“There was a woman who was 25 and had had type 1 diabetes for nine or ten years, and I asked if I could meet her,” she remembers. “I just wanted to see her; like, is she okay? What does she look like? Is she normal? I felt so much better when I saw her pump, and she told me she’d just been hiking. A lot of parents — you can hear it in their voice when they’re panicking — they just want to know their kids will be able to reach for their dreams.”
When Pierce is meeting with a family that has a newly diagnosed loved one, she reassures them that it will get easier. “Now it seems like you want to call the doctor for everything, but the more you manage this and learn,” she says, “you’re going to become your child’s doctor, and nurse and dietician and endocrinologist.”
Though Pierce seems to find this empowering, for Ross, being her own doctor is a source of frustration.
“The doctor just says, ‘Here’s a general guideline, and you figure out the dosing from there,’” she says.
Mary Tyler Moore, who was diagnosed with type 1 diabetes at age 34, and who currently serves as international chairman for the Juvenile Diabetes Research Foundation, can relate. She is quoted on the organization’s site: “Both children and adults like me who live with type 1 diabetes need to be mathematicians, physicians, personal trainers, and dietitians all rolled into one. We need to be constantly factoring and adjusting, making frequent finger sticks to check blood sugars, and giving ourselves multiple daily insulin injections just to stay alive.”
As the largest charitable supporter of type 1 diabetes research, the foundation is currently sponsoring $568 million in charitable research in 17 countries. This may seem like a lot, until one considers the fact that the average cost of bringing a new drug to market is $1.3 billion (according to the Tufts Center for the Study of Drug Development).
“People have told me they may be leaving the world of type 1 diabetes research and going into other research because there’s just no funding to keep it going, and clinical trials are very expensive,” says McParland.
The research for a cure focuses on two main approaches: cell-replacement therapy and an artificial pancreas. The problem with cell-replacement therapy is that regardless of how many new beta cells are added, the immune system of a person with type 1 diabetes would still attack and kill them. However, the Juvenile Diabetes Research Foundation has partnered with a company that may have overcome this obstacle. In November 2014, San Diego–based ViaCyte, Inc., a regenerative medicine company, began experimental treatments at University of California San Diego using its proprietary encapsulated cell-replacement therapy.
McParland likens ViaCyte’s encapsulation device to shark-proof cages used by underwater photographers.
“If the photographer is in that cage, he can take photos but the sharks can’t get to him.” Similarly, the encapsulation device is designed to contain insulin-producing beta cells and allow the insulin to be released into the body, all while protecting the beta cells from the body’s immune system. “It’s a pretty revolutionary concept that has been on the drawing board for a long time and now, for the first time, is being tested on people.”
Pierce and Calabrese do their best to keep up with the advances toward a cure. In the meantime, they, along with every other person whose life has been affected by type 1 diabetes, want people to understand not only the severity of the disease, but how different it is from type 2.
“There is so much confusion out there,” says Calabrese. “My son didn’t develop this because we fed him Twinkies and Coke. And he may look like any healthy kid, but if he gets too much insulin, he could pass out or have a seizure or die.”
Sage Pierce wants other parents to realize that any child can contract this disease.
“This can hit anytime, and we don’t know what causes it,” she says. “We don’t have any type 1 in the family, but we have Parkinson’s and arthritis. Some people say it’s environmental. There are all these theories and not one reason. If you study up, you’ll see that in the past couple of years, more and more Caucasians are being diagnosed with type 1. What if it’s something from plastics or something in our food? Who knows? You hope that none of your friends’ kids get it, but in the back of your mind, you know if it happened to your son, it can happen to anyone.”
Comments