 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

A thin column of steam rises from a 12-ounce styrofoam bowl of artichoke-and-kale soup cooling on a dinner cart in the break room of Dr. Patrick Yassini’s office, which is located next to Sharp Coronado Hospital. It’s a scene familiar to many doctors — just moments ago, Dr. Patrick Yassini rushed out to attend to a patient.
Unlike other doctors, however, Yassini is off to see one patient only. He does not feel the mounting pressure to process, examine, diagnose, and get that patient out the door so he can move on to the other five or six patients in adjacent exam rooms or out in the waiting room. This is because Yassini practices medicine at his own pace — anywhere between a few seconds for a prescription refill, to a ten-minute visit, to an hourlong session which might include a full exam, tests, even time to chat and answer questions about more than what hurts at the moment.
The present visit is brief. After a quick question from a patient and a look at the vitals, Yassini returns to the break room. He sits in a chair in the corner. Cradling the bowl of soup in one hand, he blows on it, and, half smiling, gingerly spoons a bit of the soup into his mouth.
Yassini is a family doctor, and he calls his practice Total Priority Care. He offers a raft of services, everything from sports and occupational medicine to weight management and skin care. Yassini examines mostly Coronado residents, youngsters, young adults, career-makers, homemakers, retirees — practically anyone with a pulse. This, for Yassini, is the perfect clientele. Rather than work with insurance companies, he charges patients an annual membership fee according to a sliding scale based on age. The scale starts at $1200 for patients 18 or younger and tops out at $2400 for patients 50 and over. Yassini is one of a handful of direct-pay doctors in San Diego intent on sheering off the rivets from boilerplate “patient care” with a new model of medicine based on an old set of criteria.
What these doctors practice has been described in different ways — concierge, subscription-based, direct-pay — but whatever it’s called, Yassini hopes his patients see this not as savvy pay-as-you-go lip-service but as part of a sincere effort to let the physician’s healing hands do the talking when it comes to quality healthcare.
With this approach, Yassini explains, doctor and patient agree to bypass the insurance system — any insurance system, private or government-sponsored. Wishing a polite yet firm pox on both their houses, Yassini enters into a one-on-one financial and medical relationship with his patients. He offers a third voice in the debate over healthcare by delivering a calculus of liberal personal care and conservative financial management, which, proponents claim, yields better results.
Come as you are
Yassini’s practice is on Coronado’s south end, in a medical park located on the same palm- and live-oak-shaded street as Sharp Coronado Hospital. Up two half-flights of stairs, there is a spacious waiting room surrounded by a suite of doctors’ offices. These have been leased by independent and group practices.

While the chairs in the waiting area are three-quarters full this morning, none outside Yassini’s reception window are occupied.
At the front desk, Yassini’s two staff members greet patients on their way in. Denise Lloyd and Haifa Libed serve double-duty as nurses and receptionists, and, in Lloyd’s case, triple duty as bookkeeper for the practice.
It’s midmorning and Yassini is seeing his first patients of the day. Among them is retired special-needs teacher Lee Booth, who has been coming to Yassini since the day he saved her life.
A resident of Scripps Ranch, Booth is a small woman with a fierce smile and gentle grayish-blue eyes that seem to say I’m still alive, and, well, that’s all there is to it.
“I was brought into the emergency room here with a failed liver and kidney, at Dr. Yassini’s request,” she explains. A special-education teacher at Decatur High School in Seattle, Booth fashioned a career out of making herself clear to students. Upon retirement in 1992, she was drawn south to San Diego’s better weather.
Her husband, Booth says, began to see Yassini as his personal physician soon after the couple arrived in San Diego. Hearing good reports about the new doctor, Lee was considering switching when events forced the issue.
“I was going to switch over to Dr. Yassini even before this all happened,” she says.
“This all” is Lee’s way of describing the liver and kidney failure, an alcohol-induced crisis, which, compounded by diabetes, crippled her body’s filtration systems and nearly killed her. Almost as an aside, she mentions that she’s a breast-cancer survivor.
”When I came into the emergency room, the doctors told me they probably couldn’t keep me alive through the day. So, it was ten days in the hospital and the understanding that they were going to do a transplant — which I ended up not having.”
A recovering alcoholic, Booth says that excessive consumption induced her body’s various organs to put up a white flag against the daily abuse.
“I was told that, if I ever had another drink, I wouldn’t be alive, and I was lucky that they got me through that.”
Other doctors, she claims, never picked up on the heavy alcohol use that increased after she retired from teaching.
“It was a daily thing that went on mainly in the nighttime because, obviously, I was a teacher and would work. Then, when I retired, it was pretty much from eight in the morning onward.”
Lee says it wasn’t AA or rehab that eased her down the road to recovery; it was Dr. Yassini’s custom-made treatment program. From the moment he met her in the emergency room, he’s helped her every step of the way.
“In rehab centers or AA, you deal with the emotions. But there’s a lot going on medically, which is why they’re thinking relapses are happening so much [among alcoholics]. People don’t get retrained in their thinking and don’t understand what’s going on in the thought processes when you’re drinking that much.”
Through Yassini’s approach to medicine, Lee has also been able to avoid the forest of red tape that usually accompanies the sort of treatment she sought for her alcoholism.
“Being able to see him every week — even every day, if I needed to — that just wouldn’t have happened,” she says of the doctors she had in Seattle. “And that’s not even considering insurance coming in and saying, ‘Well, if you’re not dying, we ain’t going to pay for it,’ so you’d have to have their approval, as well.”
Healthy style
As I’m talking with Lee, Yassini pokes his head into the exam room to greet his patient.
“Good to see you,” he says. His words to Lee are neither forced nor rushed.
“Good to see you, Doctor,” she replies with an exuberant smile.
“Today, Lee is in for a check-up, is all,” Yassini announces. He sits on the edge of the exam chair.
Yassini offers patients a “Lifestyle Program,” which enlists the aid of lifestyle coaches on everything from diet to exercise to vitamin supplements. He says the default position of most insurance companies would discourage patients from taking advantage of this program.
“Unfortunately, our insurance-reimbursement system does not allow us to use lifestyle decisions. They encourage us to use drugs instead.” Yassini glances over at Lee. “Having this kind of relationship with patients allows me to work for them again, and make the best recommendations, not necessarily the ones that are favorable to the reimbursement system.”
The current system, with its high turnover and low expectations, can make even well-intentioned doctors nothing more than pharmaceutical vending machines.
“Drugs are cheaper and faster when you only have five or ten minutes with a patient,” Yassini says. “You don’t even want to start talking about anything important, like the patient’s mood. Sometimes, we need hours to discuss the things going on in our lives that are affecting our health. I know doctors — I’ve been there — with a busy schedule and 40 patients to see in a day; you just do not want to ask that question. It’s easier to write the prescription for Prozac and send them on their way.”
Yassini’s comments strike a bell for Lee, who has seen firsthand the inflated worth of pharmaceuticals.
“It’s a huge problem,” she says. “In my AA group, I think I’m the only one not on Valium or Vicodin. But it’s so easy, like you said, because, what with the [limited] time that a doctor usually has with a patient, it’s easier just to give them something, a drug of some sort.”
Father and son
Yassini came down to the U.S. from north of the border in 1987. His parents were Iranian immigrants to Canada, and his father, Dr. Hossein Yassini, had finished his internship in Toronto. For 35 years, Yassini’s father, now retired, made a living in and around Wheeling, West Virginia, present at the births, deaths, illnesses, and recoveries of the rich, poor, and in-between.
“I grew up at a time when my father was the family doc in town,” Yassini tells me in the office’s break room. “He delivered babies and ran into the hospital in the middle of the night to take out people’s appendix. He made regular rounds at the hospital and the nursing homes, and people would knock on his door in the middle of the night and phone him at all hours of the day.”
Because his father’s devotion to his patients often evolved into friendship, interruptions dogged the normal rhythm of family life.
“Every time we went out to eat, or to a party, or even to the park, my father would run into patients who would say ‘hi’ to him and ask him to take a look at something,” Yassini recalls. “He was very giving with his time and his art, and I saw the impact he made on people’s lives. I’m sure that shaped me.”
After four years of medical school, followed by five years in residency, Yassini discovered that the world of medicine he’d left behind in West Virginia seemed to have been abandoned by the rest of the world, too.
“Nine years after entering medical school, I’m walking out into the real world, and I found that the practice of medicine was totally foreign to me. It’s nothing like what my dad did. Nothing at all.”
One of Yassini’s receptionists pokes her head in to announce another patient’s arrival. Yassini gestures for me to follow him down the hall to an exam room.
Extra innings
With other business to attend to, Yassini leaves me with the second patient of the day, Phil Kincaid, who makes it clear that, as far as he’s concerned, Yassini has found the perfect niche.
Kincaid stands at six-foot-four inches in height — he looks as if he’s confident he’s earned his relaxed yet jovial self-possession through nine decades of practice.
“I’m 91…and a half!” he exclaims. He laughs.
A retired lineman for Sempra Gas and Electric, Kincaid last saw a regular paycheck 30 years ago, and he attributes any extra innings he gets to play in this life to Yassini’s ministrations.
“He’s kind of a holistic doctor, and not only that, he’s a good friend and a good person, and I just can’t say enough about him,” Kincaid says. “I don’t think, honestly, I’d be here if it wasn’t for him helping me along.”
One of Yassini’s first patients to subscribe to Total Priority Care, Kincaid considers it a hit.
“You pay about $200 a month, $2400 a year,” he explains. “For that, he’ll see me any time of the day or night, and he’ll come to my house, come down here at different times of the day or the night. And if I make an appointment, I can get right in. They take care of me right now, and that’s a big relief. Although I have Medicare and other programs, this is extra. I’m more than willing to pay for it.”
The door swings open, and Yassini enters the exam room.
“Hi, Patrick,” Kincaid says, the smile returning to his face.
“Hello, Phil. How are you doing?”
“Well, I’m here,” he says, as if the act of living were the greatest medical feat he’s ever heard of.
In a way, it is. A while back, Kincaid explains, he began experiencing problems with balance and having headaches.
“So, Dr. Yassini said that it’s better to get a scan of your head,” Kincaid recalls. “They checked it out and found this tumor there. I met with the doctor who was going to take care of this, and I asked Dr. Yassini to come down with me. My son was also there, and they told me what the problem was and told me how they’re going to fix it. They’re going to zap it off, they told me — so I had five treatments and it’s gone. It’s gone — the tumor is completely gone. I had a check-up a year afterward, and it’s still gone. I’m going in for another one pretty soon to check it again.”
“We had to coordinate care with a radiation oncologist, a regular oncologist, and a neurologist,” Yassini says. “That’s not an easy feat, staying in contact, and making sure everyone is communicating and understanding everyone. That takes time.”
The breaking point
Until five years ago, Yassini tolerated the typical, grueling medical schedule. Then, one day, in a moment of clarity, he realized he didn’t have to do it.
“I remember exactly what happened,” he says. “It was a month that everyone got paid but me. I was trying to explain to my wife why I didn’t bring home any money that month, and the question she asked was, ‘Do you realize you’re working about 80 hours a week?’ It just hit me at that point. I said to myself, This is ridiculous; I’ve been working for free for a month! The midlevels got paid, the staff got paid, the rental owners got paid, the utilities got paid — everyone got paid but me. I was working 80 hours a week to maintain everyone else’s job.”
As we head down the hall to see another patient, Yassini says that, these days, his usual workload is a handful of patients and a few afternoon home visits a day.

Time and time again
Like Yassini, internal and holistic-medicine specialist Dr. Pamila Brar has given up the hectic pace of the turnstile approach to medicine to embrace the most important ally of any doctor.
“Time is the currency of excellence,” she says, quoting direct-pay pioneer Steven Knope. Brar has taken this adage as her mantra.
“I remember hearing that expression and feeling so frustrated, because that was the one thing I didn’t have in my practice — time.” We are in her office at Scripps Memorial Hospital in La Jolla. “These patients would wait to see me for months, and there were patients of mine who were elderly people, hobbling along in their walkers and going to see their doctor, and I only had 15 minutes [with them]. I felt so terrible that I wasn’t able to sit with them and talk about what was happening in their lives.”
A New Orleans native with elegant Indian features, Brar sits behind her office desk with relaxed confidence. Fixing her gaze on the ceiling, she seems to consider every angle of each question.
“Sometimes, it’s just the listening that helps people,” she says. “When my time is so greatly restricted, that restriction interferes with my ability to be present and to provide the best service for my patients.”
Charging a fee similar to Yassini’s, Brar asks for $2500 for individuals, $4500 for couples. She offers a reduced fee based on a sliding scale for children of patients — from $500 for children ages 15–18, to $2000 for children over 35.
After finishing her residency in 1998, Brar entered what she calls “a more standard, large medical group.” For nine years, she put time in with Scripps Medical Clinic Group of San Diego, averaging 15–30 patients a day. Her appointment book was filled three months in advance, and she often worked from 7:00 a.m. to 7:00 or 8:00 p.m., five days a week. Looking back, while she acknowledges that parts of the experience were “gratifying,” she describes the constant high volume of patients visiting the office as a “treadmill.”
“When my patients needed me, I was fully booked up,” she says. “Often, they would end up in urgent care. It was a very frustrating way to practice.”
In 2007, the group sought to alleviate the high volume in the exam rooms by adopting the concierge model Brar practices today. Two years later, having learned the value of keeping the patient front and center, she opened a solo practice.
Brar went from 3000 patients a year to 300 patients in a short time span. It was a drastic change, but the results were remarkable. For what she’d lost in volume of patients, she more than made up in more reasonable work hours.
“The flip side,” she says, “the difficult side of this sort of practice is that you are on call pretty much 24 hours a day. So, you trade the pace for being available all the time. But it’s much better for me.”

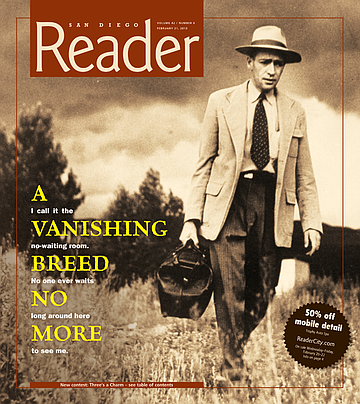
No-waiting room
The direct-pay approach allows a doctor to hang out a shingle on his own terms, as Dr. Martin Schulman has done in a tony strip-mall in Encinitas. His 1048 square feet of rented office space consists of two exam rooms, a back office, a restroom, and a reception area. He shows me a room set aside for a high-powered laser to treat tendonitis, bursitis, and any other “itis” that comes down the pike. (A few months after we spoke, Schulman moved his office a mile south to Cardiff. An even more Spartan setup, the new 165-square-foot digs consolidates exam room and office — desk, exam table, and other accoutrements — into a single space.)
“It’s very much a sideline of what I normally do as a primary-care doc,” he says as we sit in his waiting room — though that’s not what he calls the small atrium on the other side of the reception desk. “I call it the ‘no-waiting room’ — no one ever waits long around here to see me.”
Schulman takes me on a tour. He’s organized everything toward economies of scale, cutting expenses so close to the bone that he’s intimate with the contents of the office’s storage closet.
“I do the cleaning around here,” he says, gesturing at the vacuum and cleaning supplies.
As we round the corner back to the reception desk, Schulman stops short. He picks up and holds out a white cotton laundry bag half filled with patients’ hospital gowns — the kind that show more than they hide.
“It is happenstance that these are here today,” he says with a small, embarrassed shrug. “But I also do the laundry. We don’t go through a lot of the gowns, but when we wash them — well, to have a professional service would be ridiculous, so we just bring them home, and I wash them there.”
Teach and heal
A graduate of UC Berkeley and UC San Diego, Schulman tells me that, after completing his residency at UC Irvine, he joined a three-man private practice.
“I liked the patients,” he says, “I liked the office. I liked everything about it, except, at that time — we’re talking 1989ish — I wasn’t sure about buying into a practice.”
After a year, Schulman and his partners parted amicably — one former partner remains Schulman’s family’s doctor — and for the next 15 years, Schulman worked as a teaching and clinical physician at UCSD.
While Schulman appreciates the work done by doctors who provide a full range of advocacy for their patients, he decided to make his own practice as simple as possible, focusing on keeping overhead down so he could spend more time with the patients. He took on a UCSD teaching position to supplement his income.
He also looked at the higher rates among other direct-pay docs and realized he wanted to keep his charges lower.
“What I ended up with is a bit of a hybrid,” he says. “I knew I needed to have an annual fee, but I didn’t want to be in that $1800 range.”
Schulman charges $800 a year for an individual, $500 for each additional family member; the fee can be paid quarterly, or in a lump sum, and is refundable at any time. He hopes patients see the fee as a rolling investment in the medical practice.
“I do tell patients that, in a sense, they are investing in the practice, and the return on their investment is that they can get me anytime they want,” he says. “They can get in that day, they can be seen on time and after hours. They can reach me on my cell. Basically, patients get all the things you can’t normally get out of a medical practice.”
Schulman dropped Medicare and refuses to contract with insurance companies. He works for cash or credit card. He also takes checks.
“I charge a fair price and get 100 percent of what I charge,” he says, “and I don’t have Blue Cross telling me I only get so much of a percentage out of a charge.”
Without the overhead of an accounts-receivable department, Schulman only needs to reserve a small amount of time for bookkeeping.
“Patients walk out of here with a billing statement that says who they paid, a statement that says ‘Paid in Full’ at the time of service and all the codes they need.”
If patients want to claim services with their insurance company, Schulman says, the codes allow them to go online, download a claim form, and deal directly with their insurance company.
Sticking with it
According to Schulman, once his patients make the commitment to accompany him on his experiment in this alternative medical practice, they tend to stick it out.
“Pretty much whenever patients come in for the meet-and-greet, I can’t think of anyone who hasn’t signed up and stayed,” he says.
His cell phone rings, and Schulman moves with a sure foot around to the other side of the reception desk to take the call. In the meantime, a brunette woman in her late 30s, early 40s enters Schulman’s office. The woman looks healthy and athletic in loose warm-up pants and a matching sweatshirt.
Schulman finishes his call. The woman does not give her name, but Schulman knows her immediately.
“Hi, how are you?” she asks with a smile.
Schulman smiles back. “Hello. What’s up?”
The woman tells Schulman she’s been to the chiropractor and is looking to see if Schulman will fill a prescription.
“Ooh…” It’s half question, half warning that this request is dubious, at best.
She hangs her head in exaggerated shame. “I guess I should come see you first, huh?”
The woman knows how Schulman operates. Walk-in appointments are welcomed, of course, but the office is not a dispensary — not even for subscribers.
“This is a chronic thing,” she says, meaning to shore up her weak case by offering her own diagnosis.
But Schulman will have none of it. “Have we talked about it before?”
“I don’t know.” The woman changes tack. “I don’t care. I’ll see you if I need to.”
“Would that be okay? Even if it’s just a quick look? Would you like to set something up?”
“Sure.” The woman glances at me. “Do you want me to call when you’re less busy?”
“No, no!”
Schulman sets up their meeting for the next day at 1:00, before his daughter’s 3:30 soccer game.
The woman now heads to the door but brings herself up short before opening it. “And would you mind checking something else?” she asks. “I’ve got this spot on my skin. I want to make sure it’s not turning into melanoma.”
Have stethoscope, will travel
One of the more rewarding features of his practice, Yassini says, is the ability to meet his patients — often literally — where they live.
Upon entering Yassini’s office, a patient is welcomed by a framed feature article in a local magazine on Yassini’s special brand of medical practice. The one-page spread hangs on the wall in a frame and includes a picture of Yassini astride an oversized tricycle, the kind used by tourists and taxi drivers in the Philippines. The doctor, however, usually rides around town on a beach bicycle, his medical bag stuffed into one of two large saddle baskets.
The morning’s appointments all met, Yassini explains that afternoons are reserved for house calls. Today, with two home visits on his schedule and a reporter in tow, Yassini decides to take his two-tone gray-and-black Kandi COCO. There are bucket seats for driver and passenger, and a back seat for two more passengers — more than enough room. Advertised as “the cheapest car in the world,” the Chinese-made COCO is an electric car with a top speed of 25 mph and a charge that gives it a 50- to 60-mile range. It is ideal for Yassini’s needs.
We roll at a steady 15 miles per hour along Coronado’s B Avenue. Yassini tacks perpendicular to the traffic on 3rd and 4th streets, then picks his way down side streets, headed to the first of two house calls on the afternoon schedule.
At one point during the short trip, Yassini pulls over to the side of the road to take a call on his cell phone. Like a Marcus Welby for the digital age, Yassini talks to another doctor about a patient’s current status in fast snatches of medical jargon. Then we start out again. After a few blocks, we park in a residential area. Yassini grabs his medical bag, a tan leather double-buckled satchel, and we head for his patient’s house.
Vincent Lovejoy’s hospital bed takes up most of the small room where we meet him. Sunlight streams in through a bank of windows, turning the space into a terrarium, but Lovejoy doesn’t seem to mind. The bed reclines at 45 degrees, allowing him a comfortable sitting position.
“This used to be my wife’s garden room,” he says, referring to his late wife. “That’s why there are all the windows. Because it’s closer to the bathroom, they turned it into a sick room for me.”
Lovejoy wears a hospital gown, a sheet pulled to his waist. His feet stick out at the bottom, and the tip of one big toe is in terrible shape — black and blue, and gnarled as a root.
Yassini breaks open his medical bag. He takes Lovejoy’s blood pressure, then listens to Lovejoy’s pulse.
“What’s it like, not being able to put any weight on this hip?” Yassini asks.
“Well, I’ve been walking around on it some.” Lovejoy sounds tentative, as if unsure whether he should have been walking. But Yassini nods and smiles. Lovejoy continues with more confidence. “I’ve been getting exercise. I don’t spend so much time here.”
“After his brand-new hip repair, it slipped a little bit,” Yassini tells me. His voice has an academic tone — this might be how he sounds with residents. “Normally, the reason we repair fractures is so they can walk on them right away and avoid all the things associated with prolonged bed rest, while we’re trying to get the hip repaired. Unfortunately, with Mr. Lovejoy…it was too good to be true. On day three, it started giving him a lot of pain. We X-rayed the hip repair and saw that the hardware had slipped a little bit. Now he has to sit and not put a lot of weight on it for several weeks until it heals up.”
One step at a time
Yassini now attends to Lovejoy’s toe.
“How long have you had this issue here with the tip of this toe?” he asks.
“I’ve had it for awhile, and I’ve wanted to go to the podiatrist, but I’ve been tied up with this accident. So, otherwise…”
“Podiatrists don’t make house calls, do they?” Yassini says, and everyone in the room laughs. “Well, we’ll get you back on your feet in no time, with all the hard work you’re doing. I hear you’re doing very well with the therapy.”
“Oh, good, I’m glad you heard that,” Lovejoy says. “The therapist thinks I’m doing it well.”
The last issue of the visit is the urinary catheter. And, finally, it seems, Yassini gets to the real purpose of his visit.
“I hear you want to keep it in,” he says.
Lovejoy offers what he clearly considers his best argument. “Yes, the reason is, I can’t maneuver to the bathroom yet. So, if I get up to go to the bathroom — well, I can’t do that now.”
Yassini isn’t sold. “How about using the bedside [bed pan] or using a urinal?”
“I use the bedside pan, but the urinal doesn’t work very well.” A sour look passes over Lovejoy’s face. “It’s very messy.”
Yassini’s still not sold. “The longer we keep this [catheter] in, the more dangerous it is [from the risk of infection]. Sooner or later, we have to decide to do something about it.”
Lovejoy offers last argument. “From what the exercise man says, the way I’m going, I’m walking enough I should be able to take the catheter out pretty soon.”
“Do you think ‘pretty soon’ means within a week or two?” Yassini asks.
“I don’t really know.” Now Lovejoy sounds resigned. “I…I imagine a week or two.”
“So, let’s give it a week,” Yassini says. “Okay?”
“At least a week.” Lovejoy’s smile turns into a desperate frown. “Please.”
“We’ll give it a week and touch base,” Yassini reassures him. “And if things are continuing to get better, and if we think within two weeks it’s going to work, we’ll leave it in. Sound good? But if it looks like it’s going to take longer than that, I recommend we take it out as soon as possible. All right?”
Final exam
Yassini grabs his stethoscope. He pulls Lovejoy’s hospital gown away from his chest, stoops, and places the chestpiece over Lovejoy’s heart. Yassini nods at what he hears and returns the stethoscope to his bag. Then he straightens up to deliver a final lesson.
“You can see this is a narrow little room,” he tells me. “So, you can imagine it’s a huge deal to get him into the office. There are stairs, and the orthopedic surgeon said [that Lovejoy’s hip] is toe-touch weight-bearing — he can’t put more than a toe touch on that side, or he runs the risk of slipping it some more.
“[If we have to] get him into a wheelchair and roll him down the stairs, it’s going to be a big deal. He’s not going to be in this [situation] long-term, so there’s no sense in getting him a new house or renting an apartment or putting in a ramp, because this is just temporary. The home visits are the only way to deal with this situation.
“Otherwise, the cost of a paramedic and an ambulance coming here and picking him up and putting him on a gurney and taking him in — look how much that costs. My time is cheap, compared to those guys.”
As if this is news to him, Lovejoy perks up. “How much does it cost?”
“It would probably be about $800, and that’s just for one trip,” Yassini says. “Then they have to wait for you until you’re done with your exam and wait until you come back.”
Yassini reaches into his bag for his ophthalmoscope.
As the doctor begins this final examination of his patient, Lovejoy tells me about his life.
A San Diego native and retired chemical engineer, Lovejoy bought his house from his parents. He estimates it’s about 100 years old. Lovejoy says he enjoys the doctor’s home visits, if only because it avoids the hassle and indignity of being frog-walked from his bed to a wheelchair. Besides, Yassini’s visits remind Lovejoy of his youth.
“When I was growing up, I don’t remember any office calls,” he says. “They always came to your house with the little black bag.”
He glances at Yassini’s bag and, noticing that it’s light brown, shrugs his shoulders and smiles.
“I don’t think I ever went to a doctor’s office when I was growing up,” he says.
In the bag
His day almost over, Yassini relaxes a bit behind the wheel of the COCO and reflects on his reasons for choosing San Diego — more precisely, Coronado — as his base of operations.
“I came here for my residency,” he says as he navigates traffic. “I rented a room over someone’s house here in Coronado and fell in love with the community. It reminded me of the small town in West Virginia where I grew up. I met some of the older doctors who practiced here and realized that, gosh, it’s a lot like the way my dad practiced. So I was kind of excited about it. I thought maybe there was a glimmer of hope that I could have the kind of practice I was intending when I went into medical school.”
We pull into the office suite’s parking lot, and Yassini reaches into the storage space behind the seats to grab his medical bag. He opens it for me. The contents are the tools few people remember — those of a doctor who makes house calls.
“It’s a pretty good bag for what I need,” Yassini says. He points out the mix of newfangled tools and old standbys. “There’s a blood-pressure cuff, a glucose meter, an otoscope for inspecting ears, an ophthalmoscope for the eyes, dressing supplies, a pulse oximeter [to check oxygen levels in the blood] — some swabs, latex gloves. All the basics. I take other things as I need them.”
We part then. But Yassini soon turns back, a glimmer in his eye.
“My goal is to get an ultrasound someday and take it with me.” He pats his bag. “You should see the new ones they have now. They’re only as big as laptops these days.”
97 total votes.


A thin column of steam rises from a 12-ounce styrofoam bowl of artichoke-and-kale soup cooling on a dinner cart in the break room of Dr. Patrick Yassini’s office, which is located next to Sharp Coronado Hospital. It’s a scene familiar to many doctors — just moments ago, Dr. Patrick Yassini rushed out to attend to a patient.
Unlike other doctors, however, Yassini is off to see one patient only. He does not feel the mounting pressure to process, examine, diagnose, and get that patient out the door so he can move on to the other five or six patients in adjacent exam rooms or out in the waiting room. This is because Yassini practices medicine at his own pace — anywhere between a few seconds for a prescription refill, to a ten-minute visit, to an hourlong session which might include a full exam, tests, even time to chat and answer questions about more than what hurts at the moment.
The present visit is brief. After a quick question from a patient and a look at the vitals, Yassini returns to the break room. He sits in a chair in the corner. Cradling the bowl of soup in one hand, he blows on it, and, half smiling, gingerly spoons a bit of the soup into his mouth.
Yassini is a family doctor, and he calls his practice Total Priority Care. He offers a raft of services, everything from sports and occupational medicine to weight management and skin care. Yassini examines mostly Coronado residents, youngsters, young adults, career-makers, homemakers, retirees — practically anyone with a pulse. This, for Yassini, is the perfect clientele. Rather than work with insurance companies, he charges patients an annual membership fee according to a sliding scale based on age. The scale starts at $1200 for patients 18 or younger and tops out at $2400 for patients 50 and over. Yassini is one of a handful of direct-pay doctors in San Diego intent on sheering off the rivets from boilerplate “patient care” with a new model of medicine based on an old set of criteria.
What these doctors practice has been described in different ways — concierge, subscription-based, direct-pay — but whatever it’s called, Yassini hopes his patients see this not as savvy pay-as-you-go lip-service but as part of a sincere effort to let the physician’s healing hands do the talking when it comes to quality healthcare.
With this approach, Yassini explains, doctor and patient agree to bypass the insurance system — any insurance system, private or government-sponsored. Wishing a polite yet firm pox on both their houses, Yassini enters into a one-on-one financial and medical relationship with his patients. He offers a third voice in the debate over healthcare by delivering a calculus of liberal personal care and conservative financial management, which, proponents claim, yields better results.
Come as you are
Yassini’s practice is on Coronado’s south end, in a medical park located on the same palm- and live-oak-shaded street as Sharp Coronado Hospital. Up two half-flights of stairs, there is a spacious waiting room surrounded by a suite of doctors’ offices. These have been leased by independent and group practices.

While the chairs in the waiting area are three-quarters full this morning, none outside Yassini’s reception window are occupied.
At the front desk, Yassini’s two staff members greet patients on their way in. Denise Lloyd and Haifa Libed serve double-duty as nurses and receptionists, and, in Lloyd’s case, triple duty as bookkeeper for the practice.
It’s midmorning and Yassini is seeing his first patients of the day. Among them is retired special-needs teacher Lee Booth, who has been coming to Yassini since the day he saved her life.
A resident of Scripps Ranch, Booth is a small woman with a fierce smile and gentle grayish-blue eyes that seem to say I’m still alive, and, well, that’s all there is to it.
“I was brought into the emergency room here with a failed liver and kidney, at Dr. Yassini’s request,” she explains. A special-education teacher at Decatur High School in Seattle, Booth fashioned a career out of making herself clear to students. Upon retirement in 1992, she was drawn south to San Diego’s better weather.
Her husband, Booth says, began to see Yassini as his personal physician soon after the couple arrived in San Diego. Hearing good reports about the new doctor, Lee was considering switching when events forced the issue.
“I was going to switch over to Dr. Yassini even before this all happened,” she says.
“This all” is Lee’s way of describing the liver and kidney failure, an alcohol-induced crisis, which, compounded by diabetes, crippled her body’s filtration systems and nearly killed her. Almost as an aside, she mentions that she’s a breast-cancer survivor.
”When I came into the emergency room, the doctors told me they probably couldn’t keep me alive through the day. So, it was ten days in the hospital and the understanding that they were going to do a transplant — which I ended up not having.”
A recovering alcoholic, Booth says that excessive consumption induced her body’s various organs to put up a white flag against the daily abuse.
“I was told that, if I ever had another drink, I wouldn’t be alive, and I was lucky that they got me through that.”
Other doctors, she claims, never picked up on the heavy alcohol use that increased after she retired from teaching.
“It was a daily thing that went on mainly in the nighttime because, obviously, I was a teacher and would work. Then, when I retired, it was pretty much from eight in the morning onward.”
Lee says it wasn’t AA or rehab that eased her down the road to recovery; it was Dr. Yassini’s custom-made treatment program. From the moment he met her in the emergency room, he’s helped her every step of the way.
“In rehab centers or AA, you deal with the emotions. But there’s a lot going on medically, which is why they’re thinking relapses are happening so much [among alcoholics]. People don’t get retrained in their thinking and don’t understand what’s going on in the thought processes when you’re drinking that much.”
Through Yassini’s approach to medicine, Lee has also been able to avoid the forest of red tape that usually accompanies the sort of treatment she sought for her alcoholism.
“Being able to see him every week — even every day, if I needed to — that just wouldn’t have happened,” she says of the doctors she had in Seattle. “And that’s not even considering insurance coming in and saying, ‘Well, if you’re not dying, we ain’t going to pay for it,’ so you’d have to have their approval, as well.”
Healthy style
As I’m talking with Lee, Yassini pokes his head into the exam room to greet his patient.
“Good to see you,” he says. His words to Lee are neither forced nor rushed.
“Good to see you, Doctor,” she replies with an exuberant smile.
“Today, Lee is in for a check-up, is all,” Yassini announces. He sits on the edge of the exam chair.
Yassini offers patients a “Lifestyle Program,” which enlists the aid of lifestyle coaches on everything from diet to exercise to vitamin supplements. He says the default position of most insurance companies would discourage patients from taking advantage of this program.
“Unfortunately, our insurance-reimbursement system does not allow us to use lifestyle decisions. They encourage us to use drugs instead.” Yassini glances over at Lee. “Having this kind of relationship with patients allows me to work for them again, and make the best recommendations, not necessarily the ones that are favorable to the reimbursement system.”
The current system, with its high turnover and low expectations, can make even well-intentioned doctors nothing more than pharmaceutical vending machines.
“Drugs are cheaper and faster when you only have five or ten minutes with a patient,” Yassini says. “You don’t even want to start talking about anything important, like the patient’s mood. Sometimes, we need hours to discuss the things going on in our lives that are affecting our health. I know doctors — I’ve been there — with a busy schedule and 40 patients to see in a day; you just do not want to ask that question. It’s easier to write the prescription for Prozac and send them on their way.”
Yassini’s comments strike a bell for Lee, who has seen firsthand the inflated worth of pharmaceuticals.
“It’s a huge problem,” she says. “In my AA group, I think I’m the only one not on Valium or Vicodin. But it’s so easy, like you said, because, what with the [limited] time that a doctor usually has with a patient, it’s easier just to give them something, a drug of some sort.”
Father and son
Yassini came down to the U.S. from north of the border in 1987. His parents were Iranian immigrants to Canada, and his father, Dr. Hossein Yassini, had finished his internship in Toronto. For 35 years, Yassini’s father, now retired, made a living in and around Wheeling, West Virginia, present at the births, deaths, illnesses, and recoveries of the rich, poor, and in-between.
“I grew up at a time when my father was the family doc in town,” Yassini tells me in the office’s break room. “He delivered babies and ran into the hospital in the middle of the night to take out people’s appendix. He made regular rounds at the hospital and the nursing homes, and people would knock on his door in the middle of the night and phone him at all hours of the day.”
Because his father’s devotion to his patients often evolved into friendship, interruptions dogged the normal rhythm of family life.
“Every time we went out to eat, or to a party, or even to the park, my father would run into patients who would say ‘hi’ to him and ask him to take a look at something,” Yassini recalls. “He was very giving with his time and his art, and I saw the impact he made on people’s lives. I’m sure that shaped me.”
After four years of medical school, followed by five years in residency, Yassini discovered that the world of medicine he’d left behind in West Virginia seemed to have been abandoned by the rest of the world, too.
“Nine years after entering medical school, I’m walking out into the real world, and I found that the practice of medicine was totally foreign to me. It’s nothing like what my dad did. Nothing at all.”
One of Yassini’s receptionists pokes her head in to announce another patient’s arrival. Yassini gestures for me to follow him down the hall to an exam room.
Extra innings
With other business to attend to, Yassini leaves me with the second patient of the day, Phil Kincaid, who makes it clear that, as far as he’s concerned, Yassini has found the perfect niche.
Kincaid stands at six-foot-four inches in height — he looks as if he’s confident he’s earned his relaxed yet jovial self-possession through nine decades of practice.
“I’m 91…and a half!” he exclaims. He laughs.
A retired lineman for Sempra Gas and Electric, Kincaid last saw a regular paycheck 30 years ago, and he attributes any extra innings he gets to play in this life to Yassini’s ministrations.
“He’s kind of a holistic doctor, and not only that, he’s a good friend and a good person, and I just can’t say enough about him,” Kincaid says. “I don’t think, honestly, I’d be here if it wasn’t for him helping me along.”
One of Yassini’s first patients to subscribe to Total Priority Care, Kincaid considers it a hit.
“You pay about $200 a month, $2400 a year,” he explains. “For that, he’ll see me any time of the day or night, and he’ll come to my house, come down here at different times of the day or the night. And if I make an appointment, I can get right in. They take care of me right now, and that’s a big relief. Although I have Medicare and other programs, this is extra. I’m more than willing to pay for it.”
The door swings open, and Yassini enters the exam room.
“Hi, Patrick,” Kincaid says, the smile returning to his face.
“Hello, Phil. How are you doing?”
“Well, I’m here,” he says, as if the act of living were the greatest medical feat he’s ever heard of.
In a way, it is. A while back, Kincaid explains, he began experiencing problems with balance and having headaches.
“So, Dr. Yassini said that it’s better to get a scan of your head,” Kincaid recalls. “They checked it out and found this tumor there. I met with the doctor who was going to take care of this, and I asked Dr. Yassini to come down with me. My son was also there, and they told me what the problem was and told me how they’re going to fix it. They’re going to zap it off, they told me — so I had five treatments and it’s gone. It’s gone — the tumor is completely gone. I had a check-up a year afterward, and it’s still gone. I’m going in for another one pretty soon to check it again.”
“We had to coordinate care with a radiation oncologist, a regular oncologist, and a neurologist,” Yassini says. “That’s not an easy feat, staying in contact, and making sure everyone is communicating and understanding everyone. That takes time.”
The breaking point
Until five years ago, Yassini tolerated the typical, grueling medical schedule. Then, one day, in a moment of clarity, he realized he didn’t have to do it.
“I remember exactly what happened,” he says. “It was a month that everyone got paid but me. I was trying to explain to my wife why I didn’t bring home any money that month, and the question she asked was, ‘Do you realize you’re working about 80 hours a week?’ It just hit me at that point. I said to myself, This is ridiculous; I’ve been working for free for a month! The midlevels got paid, the staff got paid, the rental owners got paid, the utilities got paid — everyone got paid but me. I was working 80 hours a week to maintain everyone else’s job.”
As we head down the hall to see another patient, Yassini says that, these days, his usual workload is a handful of patients and a few afternoon home visits a day.

Time and time again
Like Yassini, internal and holistic-medicine specialist Dr. Pamila Brar has given up the hectic pace of the turnstile approach to medicine to embrace the most important ally of any doctor.
“Time is the currency of excellence,” she says, quoting direct-pay pioneer Steven Knope. Brar has taken this adage as her mantra.
“I remember hearing that expression and feeling so frustrated, because that was the one thing I didn’t have in my practice — time.” We are in her office at Scripps Memorial Hospital in La Jolla. “These patients would wait to see me for months, and there were patients of mine who were elderly people, hobbling along in their walkers and going to see their doctor, and I only had 15 minutes [with them]. I felt so terrible that I wasn’t able to sit with them and talk about what was happening in their lives.”
A New Orleans native with elegant Indian features, Brar sits behind her office desk with relaxed confidence. Fixing her gaze on the ceiling, she seems to consider every angle of each question.
“Sometimes, it’s just the listening that helps people,” she says. “When my time is so greatly restricted, that restriction interferes with my ability to be present and to provide the best service for my patients.”
Charging a fee similar to Yassini’s, Brar asks for $2500 for individuals, $4500 for couples. She offers a reduced fee based on a sliding scale for children of patients — from $500 for children ages 15–18, to $2000 for children over 35.
After finishing her residency in 1998, Brar entered what she calls “a more standard, large medical group.” For nine years, she put time in with Scripps Medical Clinic Group of San Diego, averaging 15–30 patients a day. Her appointment book was filled three months in advance, and she often worked from 7:00 a.m. to 7:00 or 8:00 p.m., five days a week. Looking back, while she acknowledges that parts of the experience were “gratifying,” she describes the constant high volume of patients visiting the office as a “treadmill.”
“When my patients needed me, I was fully booked up,” she says. “Often, they would end up in urgent care. It was a very frustrating way to practice.”
In 2007, the group sought to alleviate the high volume in the exam rooms by adopting the concierge model Brar practices today. Two years later, having learned the value of keeping the patient front and center, she opened a solo practice.
Brar went from 3000 patients a year to 300 patients in a short time span. It was a drastic change, but the results were remarkable. For what she’d lost in volume of patients, she more than made up in more reasonable work hours.
“The flip side,” she says, “the difficult side of this sort of practice is that you are on call pretty much 24 hours a day. So, you trade the pace for being available all the time. But it’s much better for me.”

No-waiting room
The direct-pay approach allows a doctor to hang out a shingle on his own terms, as Dr. Martin Schulman has done in a tony strip-mall in Encinitas. His 1048 square feet of rented office space consists of two exam rooms, a back office, a restroom, and a reception area. He shows me a room set aside for a high-powered laser to treat tendonitis, bursitis, and any other “itis” that comes down the pike. (A few months after we spoke, Schulman moved his office a mile south to Cardiff. An even more Spartan setup, the new 165-square-foot digs consolidates exam room and office — desk, exam table, and other accoutrements — into a single space.)
“It’s very much a sideline of what I normally do as a primary-care doc,” he says as we sit in his waiting room — though that’s not what he calls the small atrium on the other side of the reception desk. “I call it the ‘no-waiting room’ — no one ever waits long around here to see me.”
Schulman takes me on a tour. He’s organized everything toward economies of scale, cutting expenses so close to the bone that he’s intimate with the contents of the office’s storage closet.
“I do the cleaning around here,” he says, gesturing at the vacuum and cleaning supplies.
As we round the corner back to the reception desk, Schulman stops short. He picks up and holds out a white cotton laundry bag half filled with patients’ hospital gowns — the kind that show more than they hide.
“It is happenstance that these are here today,” he says with a small, embarrassed shrug. “But I also do the laundry. We don’t go through a lot of the gowns, but when we wash them — well, to have a professional service would be ridiculous, so we just bring them home, and I wash them there.”
Teach and heal
A graduate of UC Berkeley and UC San Diego, Schulman tells me that, after completing his residency at UC Irvine, he joined a three-man private practice.
“I liked the patients,” he says, “I liked the office. I liked everything about it, except, at that time — we’re talking 1989ish — I wasn’t sure about buying into a practice.”
After a year, Schulman and his partners parted amicably — one former partner remains Schulman’s family’s doctor — and for the next 15 years, Schulman worked as a teaching and clinical physician at UCSD.
While Schulman appreciates the work done by doctors who provide a full range of advocacy for their patients, he decided to make his own practice as simple as possible, focusing on keeping overhead down so he could spend more time with the patients. He took on a UCSD teaching position to supplement his income.
He also looked at the higher rates among other direct-pay docs and realized he wanted to keep his charges lower.
“What I ended up with is a bit of a hybrid,” he says. “I knew I needed to have an annual fee, but I didn’t want to be in that $1800 range.”
Schulman charges $800 a year for an individual, $500 for each additional family member; the fee can be paid quarterly, or in a lump sum, and is refundable at any time. He hopes patients see the fee as a rolling investment in the medical practice.
“I do tell patients that, in a sense, they are investing in the practice, and the return on their investment is that they can get me anytime they want,” he says. “They can get in that day, they can be seen on time and after hours. They can reach me on my cell. Basically, patients get all the things you can’t normally get out of a medical practice.”
Schulman dropped Medicare and refuses to contract with insurance companies. He works for cash or credit card. He also takes checks.
“I charge a fair price and get 100 percent of what I charge,” he says, “and I don’t have Blue Cross telling me I only get so much of a percentage out of a charge.”
Without the overhead of an accounts-receivable department, Schulman only needs to reserve a small amount of time for bookkeeping.
“Patients walk out of here with a billing statement that says who they paid, a statement that says ‘Paid in Full’ at the time of service and all the codes they need.”
If patients want to claim services with their insurance company, Schulman says, the codes allow them to go online, download a claim form, and deal directly with their insurance company.
Sticking with it
According to Schulman, once his patients make the commitment to accompany him on his experiment in this alternative medical practice, they tend to stick it out.
“Pretty much whenever patients come in for the meet-and-greet, I can’t think of anyone who hasn’t signed up and stayed,” he says.
His cell phone rings, and Schulman moves with a sure foot around to the other side of the reception desk to take the call. In the meantime, a brunette woman in her late 30s, early 40s enters Schulman’s office. The woman looks healthy and athletic in loose warm-up pants and a matching sweatshirt.
Schulman finishes his call. The woman does not give her name, but Schulman knows her immediately.
“Hi, how are you?” she asks with a smile.
Schulman smiles back. “Hello. What’s up?”
The woman tells Schulman she’s been to the chiropractor and is looking to see if Schulman will fill a prescription.
“Ooh…” It’s half question, half warning that this request is dubious, at best.
She hangs her head in exaggerated shame. “I guess I should come see you first, huh?”
The woman knows how Schulman operates. Walk-in appointments are welcomed, of course, but the office is not a dispensary — not even for subscribers.
“This is a chronic thing,” she says, meaning to shore up her weak case by offering her own diagnosis.
But Schulman will have none of it. “Have we talked about it before?”
“I don’t know.” The woman changes tack. “I don’t care. I’ll see you if I need to.”
“Would that be okay? Even if it’s just a quick look? Would you like to set something up?”
“Sure.” The woman glances at me. “Do you want me to call when you’re less busy?”
“No, no!”
Schulman sets up their meeting for the next day at 1:00, before his daughter’s 3:30 soccer game.
The woman now heads to the door but brings herself up short before opening it. “And would you mind checking something else?” she asks. “I’ve got this spot on my skin. I want to make sure it’s not turning into melanoma.”
Have stethoscope, will travel
One of the more rewarding features of his practice, Yassini says, is the ability to meet his patients — often literally — where they live.
Upon entering Yassini’s office, a patient is welcomed by a framed feature article in a local magazine on Yassini’s special brand of medical practice. The one-page spread hangs on the wall in a frame and includes a picture of Yassini astride an oversized tricycle, the kind used by tourists and taxi drivers in the Philippines. The doctor, however, usually rides around town on a beach bicycle, his medical bag stuffed into one of two large saddle baskets.
The morning’s appointments all met, Yassini explains that afternoons are reserved for house calls. Today, with two home visits on his schedule and a reporter in tow, Yassini decides to take his two-tone gray-and-black Kandi COCO. There are bucket seats for driver and passenger, and a back seat for two more passengers — more than enough room. Advertised as “the cheapest car in the world,” the Chinese-made COCO is an electric car with a top speed of 25 mph and a charge that gives it a 50- to 60-mile range. It is ideal for Yassini’s needs.
We roll at a steady 15 miles per hour along Coronado’s B Avenue. Yassini tacks perpendicular to the traffic on 3rd and 4th streets, then picks his way down side streets, headed to the first of two house calls on the afternoon schedule.
At one point during the short trip, Yassini pulls over to the side of the road to take a call on his cell phone. Like a Marcus Welby for the digital age, Yassini talks to another doctor about a patient’s current status in fast snatches of medical jargon. Then we start out again. After a few blocks, we park in a residential area. Yassini grabs his medical bag, a tan leather double-buckled satchel, and we head for his patient’s house.
Vincent Lovejoy’s hospital bed takes up most of the small room where we meet him. Sunlight streams in through a bank of windows, turning the space into a terrarium, but Lovejoy doesn’t seem to mind. The bed reclines at 45 degrees, allowing him a comfortable sitting position.
“This used to be my wife’s garden room,” he says, referring to his late wife. “That’s why there are all the windows. Because it’s closer to the bathroom, they turned it into a sick room for me.”
Lovejoy wears a hospital gown, a sheet pulled to his waist. His feet stick out at the bottom, and the tip of one big toe is in terrible shape — black and blue, and gnarled as a root.
Yassini breaks open his medical bag. He takes Lovejoy’s blood pressure, then listens to Lovejoy’s pulse.
“What’s it like, not being able to put any weight on this hip?” Yassini asks.
“Well, I’ve been walking around on it some.” Lovejoy sounds tentative, as if unsure whether he should have been walking. But Yassini nods and smiles. Lovejoy continues with more confidence. “I’ve been getting exercise. I don’t spend so much time here.”
“After his brand-new hip repair, it slipped a little bit,” Yassini tells me. His voice has an academic tone — this might be how he sounds with residents. “Normally, the reason we repair fractures is so they can walk on them right away and avoid all the things associated with prolonged bed rest, while we’re trying to get the hip repaired. Unfortunately, with Mr. Lovejoy…it was too good to be true. On day three, it started giving him a lot of pain. We X-rayed the hip repair and saw that the hardware had slipped a little bit. Now he has to sit and not put a lot of weight on it for several weeks until it heals up.”
One step at a time
Yassini now attends to Lovejoy’s toe.
“How long have you had this issue here with the tip of this toe?” he asks.
“I’ve had it for awhile, and I’ve wanted to go to the podiatrist, but I’ve been tied up with this accident. So, otherwise…”
“Podiatrists don’t make house calls, do they?” Yassini says, and everyone in the room laughs. “Well, we’ll get you back on your feet in no time, with all the hard work you’re doing. I hear you’re doing very well with the therapy.”
“Oh, good, I’m glad you heard that,” Lovejoy says. “The therapist thinks I’m doing it well.”
The last issue of the visit is the urinary catheter. And, finally, it seems, Yassini gets to the real purpose of his visit.
“I hear you want to keep it in,” he says.
Lovejoy offers what he clearly considers his best argument. “Yes, the reason is, I can’t maneuver to the bathroom yet. So, if I get up to go to the bathroom — well, I can’t do that now.”
Yassini isn’t sold. “How about using the bedside [bed pan] or using a urinal?”
“I use the bedside pan, but the urinal doesn’t work very well.” A sour look passes over Lovejoy’s face. “It’s very messy.”
Yassini’s still not sold. “The longer we keep this [catheter] in, the more dangerous it is [from the risk of infection]. Sooner or later, we have to decide to do something about it.”
Lovejoy offers last argument. “From what the exercise man says, the way I’m going, I’m walking enough I should be able to take the catheter out pretty soon.”
“Do you think ‘pretty soon’ means within a week or two?” Yassini asks.
“I don’t really know.” Now Lovejoy sounds resigned. “I…I imagine a week or two.”
“So, let’s give it a week,” Yassini says. “Okay?”
“At least a week.” Lovejoy’s smile turns into a desperate frown. “Please.”
“We’ll give it a week and touch base,” Yassini reassures him. “And if things are continuing to get better, and if we think within two weeks it’s going to work, we’ll leave it in. Sound good? But if it looks like it’s going to take longer than that, I recommend we take it out as soon as possible. All right?”
Final exam
Yassini grabs his stethoscope. He pulls Lovejoy’s hospital gown away from his chest, stoops, and places the chestpiece over Lovejoy’s heart. Yassini nods at what he hears and returns the stethoscope to his bag. Then he straightens up to deliver a final lesson.
“You can see this is a narrow little room,” he tells me. “So, you can imagine it’s a huge deal to get him into the office. There are stairs, and the orthopedic surgeon said [that Lovejoy’s hip] is toe-touch weight-bearing — he can’t put more than a toe touch on that side, or he runs the risk of slipping it some more.
“[If we have to] get him into a wheelchair and roll him down the stairs, it’s going to be a big deal. He’s not going to be in this [situation] long-term, so there’s no sense in getting him a new house or renting an apartment or putting in a ramp, because this is just temporary. The home visits are the only way to deal with this situation.
“Otherwise, the cost of a paramedic and an ambulance coming here and picking him up and putting him on a gurney and taking him in — look how much that costs. My time is cheap, compared to those guys.”
As if this is news to him, Lovejoy perks up. “How much does it cost?”
“It would probably be about $800, and that’s just for one trip,” Yassini says. “Then they have to wait for you until you’re done with your exam and wait until you come back.”
Yassini reaches into his bag for his ophthalmoscope.
As the doctor begins this final examination of his patient, Lovejoy tells me about his life.
A San Diego native and retired chemical engineer, Lovejoy bought his house from his parents. He estimates it’s about 100 years old. Lovejoy says he enjoys the doctor’s home visits, if only because it avoids the hassle and indignity of being frog-walked from his bed to a wheelchair. Besides, Yassini’s visits remind Lovejoy of his youth.
“When I was growing up, I don’t remember any office calls,” he says. “They always came to your house with the little black bag.”
He glances at Yassini’s bag and, noticing that it’s light brown, shrugs his shoulders and smiles.
“I don’t think I ever went to a doctor’s office when I was growing up,” he says.
In the bag
His day almost over, Yassini relaxes a bit behind the wheel of the COCO and reflects on his reasons for choosing San Diego — more precisely, Coronado — as his base of operations.
“I came here for my residency,” he says as he navigates traffic. “I rented a room over someone’s house here in Coronado and fell in love with the community. It reminded me of the small town in West Virginia where I grew up. I met some of the older doctors who practiced here and realized that, gosh, it’s a lot like the way my dad practiced. So I was kind of excited about it. I thought maybe there was a glimmer of hope that I could have the kind of practice I was intending when I went into medical school.”
We pull into the office suite’s parking lot, and Yassini reaches into the storage space behind the seats to grab his medical bag. He opens it for me. The contents are the tools few people remember — those of a doctor who makes house calls.
“It’s a pretty good bag for what I need,” Yassini says. He points out the mix of newfangled tools and old standbys. “There’s a blood-pressure cuff, a glucose meter, an otoscope for inspecting ears, an ophthalmoscope for the eyes, dressing supplies, a pulse oximeter [to check oxygen levels in the blood] — some swabs, latex gloves. All the basics. I take other things as I need them.”
We part then. But Yassini soon turns back, a glimmer in his eye.
“My goal is to get an ultrasound someday and take it with me.” He pats his bag. “You should see the new ones they have now. They’re only as big as laptops these days.”
97 total votes.