 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

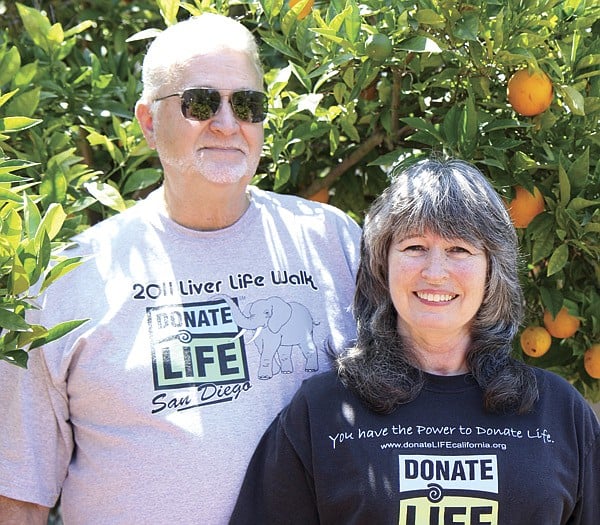
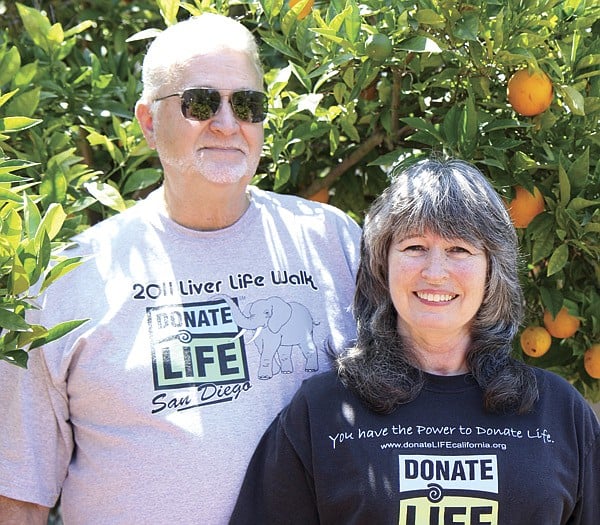
Michael McCrerey wanted to die at home. In the four years since he’d been diagnosed with liver disease, he’d been hospitalized at least a dozen times (six in the past 12 months), his abdominal cavity had been flooded with toxic fluid, and he’d shrunk from a beefy six-foot-four, 225-pound hunk of a man to a sack of bones weighing 135 pounds.
Michael’s wife Rita documented the whole ordeal. In the living room of his donor Mario Pinedo’s childhood home in National City, she heaves a large white binder into her lap, opens it, and flips to a picture of her husband at Scripps Green Hospital. Though Michael was 62 at the time, the combination of his sunken cheeks, the wheelchair, and the hospital gown ages him a good 25 years. When Rita passes the picture around the room, three of Mario’s sisters marvel at the difference between the Michael in the picture and the Michael sitting now in a chair against the far wall, beefy and healthy again, a somewhat bored look on his face.

“We got married in 1973,” Rita says. “Fool that I am. I should’ve read the fine print.”
The women laugh. The corner of Michael’s mouth twitches, but he doesn’t smile.
In 1977, after 11 years as a California Highway Patrol officer, Michael was forced to retire at 33 due to an on-the-job injury — a herniated disc. He had always wanted to be a policeman, and the retirement “pulled the carpet from under him,” Rita says. So he took to golf and scotch.
“We always liked our cocktails,” Rita says with a smirk. “Back in those years, they were doing lots of happy hours, and you could practically go have dinner with the hors d’oeuvres and that kind of thing. So he wound up having liver disease because he fell into the habit of drinking a lot.”
The average human liver weighs 2 1/2–3 1/2 pounds. The largest solid organ in the body, it performs essential functions, including detoxification of the blood and the metabolization of fats and proteins. In October 2002, Michael received his first diagnosis of cirrhosis, a disease in which scar tissue replaces healthy liver tissue, resulting in the liver’s inability to function. Cirrhosis is not reversible, and Michael’s doctor told him it was likely he would one day need a transplant. While Rita initiated the process of obtaining referrals and taking other necessary steps to get him on the transplant list, Michael went from sick to sicker, eventually developing ascites.
“[Ascites] is when your liver’s not processing the bile or liquid that it’s supposed to be processing to get your bloodstream cleaned up, so it oozes out and becomes liquid in the cavities,” Michael explains from across the room. “It balloons your stomach right out to where it looks like you swallowed a beach ball. I mean, huge and tight.”
Several times, the fluid caused Michael’s lungs to collapse.
“See. This is what his stomach looked like,” Rita says. She flips to a picture of Michael, ancient-looking and skinny, save for the giant stomach. “We went in, and they take a nice, big, long needle, poke it in your gut, and drain out the fluid.”
The first time the doctors drained Michael’s fluid, they told him he’d probably be in again in a month, and then again the month after that. But it would be another 14 months before he had to be drained again. Later, however, as his illness progressed, he went to Kaiser’s Otay Mesa gastroenterology department every Tuesday, and each time, the doctors drained 20–22 pounds of liquid from his body. That’s the equivalent of three to four two-liter bottles of soda. Every week.
“They’d suck it all out of there,” Rita says, “and when he’d come out, of course, [his stomach] would be all flat.”

Michael sits stoically, nodding every now and again. Rita’s women friends raise their eyebrows and shake their heads in sympathy. Rita doesn’t have the patience for boo-hooing, though. Once, when faced with a condescending Kaiser administrator who said something to the tune of “I know you love your husband, but there’s nothing I can do,” Rita replied, “Don’t give me that ‘woe is me, poor little wife’ stuff. This is business.” And then she proceeded to school him about a thing called “denial of medical care,” for which she would not hesitate to sue if he didn’t find a way to help her husband.
Rita’s binder, her facts, and her big silent man are all part of what she calls her “dog and pony show.”
“I’m the dog, he’s the pony,” she says.
Eventually, Michael’s loss of liver function also meant that toxins such as ammonia, which are normally made harmless by the liver, began to build up in his body. This resulted in hepatic encephalopathy, a disorder of the brain that often causes confusion and altered levels of consciousness.
“It’s like your brain waves would say, ‘I’m going to have a cup of tea,’ and then you would do something totally different,” Rita says. “He would use the TV remote and think it was the lamp or the phone.”
Along with the confusion, the encephalopathy also scrambled Michael’s personality.
“One of the special little fun side effects was that he became a secret shopper,” Rita says. “A shopaholic.”
At the time, Rita worked an express mail route for the United States Postal Service. Because she had a flexible manager who allowed her to eat lunch at home, she was able to check on Michael every day. One day, one of her neighbors stopped her and asked if she realized that packages arrived via FedEx, UPS, or DHL at her house almost daily, sometimes two or three boxes at a time. Rita was shocked. She’d never seen any of the packages.
“I was home one day, and I heard the delivery truck, so I hid and kind of watched from by the door,” Rita says. “[Michael] got the item, the delivery guy left, and he closed the door, picked up the box, and went scurrying down the hall to hide it like a damn chipmunk. He hid it in the closet. I didn’t realize that, for a year, he’d been buying things from catalogs and on the internet. Anything that said you’d get something for free, anything like free shipping, it was a trigger for him.”
By the time Rita found out about it, Michael had spent $80,000 on towels, socks, underwear, toaster ovens, comforter sets, shirts and pants, one or two of every color. Over time, Rita did see and question some of Michael’s purchases, but when she asked about them he snapped at her, saying he could buy what he wanted as long as he was paying for it. He used credit cards, and the more he spent, the more credit he was offered by the credit card companies. Michael retrieved the mail before Rita came home. He also hid much of what he bought in his closet, which Rita never looked in, and in the closet of the guest room, and under beds.
“We have ten comforter sets. There are two of us!” Rita says. “We have so many towels and sets of sheets, I had to give hundreds away. And anything with an eagle. He decided he loved eagles.”
“I’d always liked them,” Michael says. “But before then, I’d never had to have them.”
Rita nods. “Yeah. He spent $80,000 on stupid stuff.”
In early 2006, after four years of gathering information and documenting evidence, Rita’s tenacity secured Michael a spot on the transplant list and a contract at Scripps Green. On February 10, he went in for a transjugular intrahepatic portosystemic shunt (TIPS) procedure, in which a bypass relieves the pressure of the fluid going through the liver. Although normally an outpatient procedure, blood infections landed Michael in intensive care for two weeks. During those two weeks, he was a backup for two livers (he was second in line for a transplant — twice), but the infections made him ineligible.
“He was on lots of monitors, and he was always making those alarms go off,” Rita says. “When he was in intensive care, it was like he was a dead guy.”
By that point, Rita and Michael were exhausted and ready to accept Michael’s death as imminent. Against the advice of doctors, as well as her own wishes for Michael to die in the hospital so he could be an organ donor, Rita brought him home and set up a hospital bed in the living room.
“I didn’t want to die in the hospital,” Michael says. “I just wanted to pet my cat, watch the big-screen TV, and die [at home].”
∗ ∗ ∗
A pizza, fruit, and cake buffet has been set up in the fourth-floor conference room at the Lifesharing office on Camino del Rio South. People file into the room, put their bags down on their chosen chairs, and fill their plates. When I sit at the large oval table (it won’t be big enough for the 20-some-odd people who show up for tonight’s meeting) between two women, the one on my left asks, “What do you have?” I don’t understand the question until she explains that she’s had her new liver six and a half years. I inform her I have all my original organs and that I’m here researching an article.
The woman on my right introduces herself as Mary. While she takes the pineapple off her pizza (“Not kosher,” she says) she explains that her new liver came from a 14-year-old boy named Jonathan. She got two thirds of the liver, and the other third went to a baby. That was 21 months ago.
“Jonathan is my angel,” she says.
At 7:00 p.m., Sharon Ross, director of public relations and community outreach at Lifesharing, asks for a round of self-introductions. Five liver, three heart, four lung, and five kidney recipients state their names and the length of time they’ve had their new organs. Their time from transplant ranges from 3 1/2 weeks to 24 years. Rita sits at one end of the table, next to Letty, one of Mario’s sisters, whom I’d met along with two other sisters at their childhood home back in April. Letty represents one of five donor families in attendance tonight.
Rita and Letty also represent Lifesharing’s current volunteers. They’ll share their experiences with those who have come to learn about volunteering their time with the organization.
Lifesharing is the sole organ-procurement organization for San Diego and Imperial counties, a population of nearly 3.5 million people. This means that every organ transplanted in this area is recovered by Lifesharing.
A total of 58 such organizations exist across the country, 4 in California. All are federally designated, and each is a member of the United Network for Organ Sharing (UNOS), which allocates distribution of organs across the country.
Though it is a commonly held belief that there is one waiting list per organ, and that each organ is flown to wherever the patient at the top of the list happens to be, the list shifts and changes each time an organ is made available. When organs are identified, the procurement organization enters information about the organs into the UNOS computer system and runs the match program. The list of criteria that puts a patient at the top of the list include the matching of organ characteristics (size, blood type, tissue type), medical urgency, time on the waiting list, and distance from donor.
The shortage of available organs, which causes people to use terms such as “miracle” and “hero” in the world of organ donation and transplantation, is due to the fact that it is the particular circumstances of death that make a person eligible to be a donor. Only brain death and cardiac death qualify. In the days before the advancement of legal definitions for brain death, all organ recovery used to be from cardiac death, though that’s now less common. As many as eight organs can be recovered after brain death; after cardiac death, often only the kidneys and liver are recoverable. Of the more than 2 million deaths in the United States each year, less than 1 percent are brain deaths.
Once a hospital patient has been identified as a potential donor, the hospital staff contacts Lifesharing. They send out a “first responder” to evaluate the medical and social history of the patient and follow along as doctors perform tests to confirm brain death.
Billy Snyder, a Lifesharing organ procurement specialist, relates brain death to pregnancy.
“Either you’re pregnant or you’re not. Either you’re brain dead or you’re not,” he says. “There’s no wiggle-worming gray area. When someone’s brain dead, they have complete cessation of their entire brain system and all those functions that go along with it: respiratory drive, pupillary response, cornea response, any pain response, any receptor in the body.”
After brain death has been declared, Lifesharing first tries to place all organs locally. Today, over 1600 people in San Diego are waiting for organ transplants. Because the length of time an organ can live outside the body differs, the allocation varies. For example, hearts and lungs tend to stay local because they have only four or five hours of viability. Kidneys, on the other hand, can last as long as 48 hours with the use of a perfusion pump, which stimulates optimal body function for the kidney and increases the success of its transplant. If someone on the list is a perfect match, that kidney will bypass local transplant centers because it has the best chance of functioning in the body of a person with “zero mismatch.” In other cases, if Lifesharing can’t find a suitable match for organs in San Diego, they expand the search to Los Angeles, Northern California, Arizona, Nevada, and so on.
∗ ∗ ∗
Outside the doors of the conference room, past the reception desk, a narrow hallway leads to the Lifesharing staff offices. The walls of this hallway are hung with five “donor quilts,” each bearing 20 squares dedicated to the dead, whose organs and tissue live on in the bodies of strangers like those around the conference room table.
Crystal, We miss you is embroidered in white thread on a red square.
Sarah Elaine Schonhoff is stitched in green above a picture of a smiling, thin-haired baby, along with the dates 1-21-2004 and 2-10-2006.
The right half of the backside of a pair of jeans (including belt loops to just below the pocket) fills the square next to little Sarah’s. Poker chips and pictures of dice, running shoes, and a tool belt create a collage of significant mementos, along with the words “husband” and “father” spelled out in tiny Travel Scrabble letters.
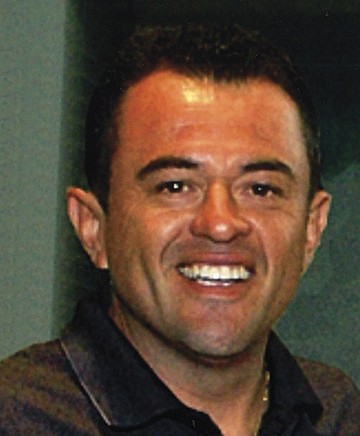
Mario Gerardo Pinedo does not yet have a quilt square. The 39-year-old owner of a National City auto-detailing shop died of a massive brain aneurism in 2006, and his sister, Letty, who sits next to Rita at the Lifesharing volunteer meeting, says the square is something she and her four sisters have been meaning to get around to. During a recent conversation, they did come to a couple of decisions. They want a Chargers background, and something about the Padres, for sure — maybe a picture — and also, perhaps, a couple of lines about Pinedo.
In July 2005, a few days before his 39th birthday, Mario went to the Chula Vista DMV to renew his driver’s license.
“They asked him if he wanted to be an organ donor, and he said yes,” Letty said on the evening we sat together with Rita, Michael, and two of Mario’s other sisters in the Pinedo siblings’ childhood home. “He comes home all excited because he was going to be a donor. My parents were telling him, ‘Are you crazy? You’re 38 years old. What are you thinking?’ And he was, like, ‘When I die, what are they going to do with it? Everything’s going to turn into a worm. I’m going to be eaten up. No. I’m going to give it to somebody. You never know, Mami. You never know whose life you can save.’”
Seven months later while at a Friday-night barbecue, Mario suffered a massive brain aneurism and was admitted to Scripps Chula Vista Hospital around 10:00 p.m. Two days later, he died.
“We all ran to the hospital, though my parents weren’t here. They were in Mexico,” Letty says. “Pretty much right away, [the doctors] told us he was brain dead. At that point, it wasn’t even what are we going to do, it was how are we going to tell our mom, and who’s going to make that call?”

It was at this point that Belen Bell, family-services specialist at Lifesharing, introduced herself to the Pinedo family. The now 57-year-old Bell, fond of brightly colored sweater sets, establishes and maintains eye contact when she explains her job to me one afternoon in another, smaller conference room. It’s been a week since the volunteer meeting.
Although Bell has several responsibilities, one of them is to obtain consent from family members for the procurement of organs. She had been at the hospital following Mario’s case but did not approach the family right away.
“We follow from a distance,” she says. “We check their labs, and we check their neurostats, to see if they’ve worsened or gotten better. We don’t go near the families until the right moment. Never do we want a family to feel that we’re hovering.”
Once a family has been informed by physicians that their loved one is brain dead, they need time to grieve, Bell says.
“What we normally listen for is ‘What is our next step? Should we be looking for a funeral home? What should we do now?’” she explains.
In the case of Mario Pinedo, this happened around 5:30 on Saturday morning, when his sisters began to discuss how they were going to tell their parents that Mario was gone. The first thing Bell did after introducing herself to Mario’s family was to ask after his mother. When his sisters informed her that their mother was in Mexico and didn’t yet know what had happened, Bell told them to call her and tell her that he was ill, not that he was dead, so she wouldn’t go into shock before the long trip home. Bell then helped the sisters decide who would drive to Tijuana to pick their parents up from the airport and drive them back into San Diego.
“She was our savior,” Letty said of Bell during our meeting at the Pinedo home. “We didn’t even look at the doctors. Belen knew all the medical lingo. If we had a medical question, we’d ask her, and in layman’s terms she would tell us what it was. She also spoke Spanish, and maybe that’s one reason why we identified with her.”
Bell’s Spanish was, in fact, the impetus for establishing the family-services department at Lifesharing. Back in 1994, when she was a translator at the Palomar Trauma Center, her current boss came to Palomar as a Lifesharing nurse to ask a family for consent. She needed Bell’s assistance to navigate the Spanish-English language barrier. Bell, daughter of a German mother and a Mexican father, was born in Venezuela, raised in Spain, and had been translating at Palomar for several years.
“At that time, our Hispanic consent rate was atrocious,” Bell says. “Very, very few Hispanic families would ever consent.”
In 2004, before Bell joined the team, the Hispanic consent rate in San Diego was 42 percent; by 2010, it had risen to 71 percent.
Even after Bell explained to Mario’s family that he had the pink dot (on top of the plastic) on his license, his parents took some convincing. Letty believes this was due in part to cultural and religious beliefs that the body must remain intact for burial.
Mario’s sister Lupe says, “I think they thought they’d give him back to us in pieces.”
To be fair, this was two and a half years before Pope Benedict XVI encouraged organ donation, when he stated publicly: “The act of love which is expressed with the gift of one’s vital organs remains a genuine testimony of charity that is able to look beyond death so that life always wins.”
It is also a common myth (one that Lifesharing staff must debunk frequently) that organ donation delays funeral plans and affects the open casket.
On Sunday, February 26, 2006, Mario’s parents gave Lifesharing their consent to donate Mario’s organs. “Everything but his pretty green eyes,” Letty says.
That same day, Michael McCrerey received a call from Scripps Green. “It’s time,” they said. “We have a liver for you.”
∗ ∗ ∗
When Billy Snyder meets new people at barbecues, parties, and bars, he dreads the inevitable “What do you do?” portion of getting-to-know-you chitchat. It’s not that he doesn’t enjoy talking about his work. But when people find out that he’s an organ-procurement specialist, responsible for recovering and transporting organs from the newly deceased to the sick and dying, he usually ends up in a 15–20-minute conversation far removed from party-friendly small talk.
Snyder has been at Lifesharing for nearly a decade, in both organ and tissue recovery. He has also worked as an embalming apprentice and a prep assistant at Greenwood Mortuary, and, at age 19, as a “body snatcher” (picking up bodies from crime scenes and traffic accidents) for the medical examiner’s investigator. Although he’d always planned to become a San Diego police officer like his father, who was on the force for 30 years, Snyder says he “fell in love with the death industry,” during his time with the medical examiner.
“It’s fascinating what happens to the body after death,” he says. “All aspects of it. The decomposition process, the trauma aspect of the body, and then also organ and tissue donation.”
Some of what Snyder says would sound macabre coming from almost any other source. But this clean-shaven 30-year-old surfer dude wears a 3/4-sleeve tattoo of chrysanthemums and lilies on his left arm, has a medical vocabulary to beat the band, and, somehow, his fascination with the science of death sounds no crazier than a fascination with, say, horticulture.
Even now, standing (sleeves rolled down, tattoos covered) in a roomful of organ recipients, where he’s encouraged to speak freely about his work, Billy Snyder is so full of energy and information that, after a while, even his graphic photographs of purplish hearts and shiny livers begin to look less horrifying and more…interesting.
When he says, “Lungs are truly one of my favorite things to come out of the body, no offense to any other recipients here” — then points to a photograph he’s taken of actual lungs and says, “Those are beautiful lungs” — I can’t see beyond the fact that they’re internal organs (and therefore gross). I wish I could.

Snyder’s job as part of Lifesharing’s surgical services team begins in the hours between consent and the organ-procurement operation. Once he’s been called in, he gathers his equipment and supplies (organ-preservation solution, instrumentation, organ-packing supplies, paperwork, etc.) and heads to the hospital where the donor has been kept “alive” on a ventilator. He stops first in the operating room, where he checks in with the charge nurse to get the details about who will be on the surgical team. Then he visits with the Lifesharing nurse to get a rundown on the donor. By this point, a recipient has already been found for each available organ, and transplant teams have been called. Once all the surgeons arrive, Snyder acts as coordinator, gathering them and relaying all pertinent medical information. When he says “pertinent,” he means “Everything. It’s a summation of how this [donor] ended up where he is.”
Tonight, at the volunteer meeting in the Lifesharing conference room, Snyder’s PowerPoint presentation consists of 18 slides, only one of which contains words. The rest are photographs Snyder has taken from the operating room. He’s held nothing back. A close-up shot of a midline incision shows a pair of metal clamps holding the body open, revealing lumps of shiny, purple, and veiny organs.
“Remember, this patient is on a ventilator,” Snyder says. “So you’re actually watching this heart beat inside this person and watching the lungs breathe. You can run your thumb over the liver and guesstimate what the fat content’s going to be after you flush the blood out.”

Another shows a crowd of scrub-mask-and-glove-clad doctors standing over a gaping abdominal cavity. Sometimes, Snyder tells us, there can be as many as 25 people in the operating room: surgeons, scrub technicians, anesthesiologists, nurses, and fellows or med students. All of them work “in symphony,” he says, “to free the organs from their anatomical structure, with the exception of vasculature.”
After the midline incision is made, usually by the heart surgeon, the abdominal cavity is packed with sterilized ice (also called “slush”), and each transplant surgeon cross-clamps, to cut off blood flow, and cannulates (running an IV-like tube into) the organ he or she is responsible for extracting. Through those tubes another cold preservation solution (modified for each organ) flushes each organ of blood and cools it from the inside. The organs are taken out of the body in the same order each time, beginning with the heart, which can last outside the body four or five hours. At most.
“From the time that cold solution starts flushing, the clock starts ticking,” Snyder says.
Inside the operating room, Snyder often plays the role of perfusionist (or preservationist) assisting one of the transplant surgeons with the flushing of an organ. He also sets up the back table where, as each organ is removed, it is measured, and occasionally biopsied, to help doctors understand how it’s going to function when transplanted. Snyder helps with documentation, and if necessary, executes “a little extra flush,” of the organ.
Then, as each organ is readied, it’s packed up using procedures that are, like all parts of the transplantation process, regulated by the United Network for Organ Sharing. Although there are some variations per organ, all are immersed in a “storage solution” (same as or similar to the solution with which they’re flushed), packed with a “triple sterile barrier,” or three closed sterile bags, then stored on ice in a cooler, and labeled. Each organ is then delivered to the transplant program either by courier, by the surgeon, or sometimes by Snyder himself.
“The heart does not leave our hands,” Snyder says. “Because of the small window, it goes [directly] from the patient to the back table, where it gets packaged up quickly, and then rushed off to the awaiting operating room. Same thing with lungs and livers. Pancreas, generally the same thing, too. But with kidneys, we can put them on a machine that will pump them, which increases the amount of time that they can stay out of the body.”
Snyder shows photographs of each organ in the same order that it comes out. After the heart come the lungs, then liver, pancreas, and kidneys. He has healthy and not-so-healthy photos of each. Some people murmur oohs, ahhs, and hmms at the pictures, perhaps wondering what their own look like.
At one point, he shows a photo of a pair of lungs that have been blackened (yes, they are indeed black) by 30 years of pack-a-day smoking. When someone asks, “Those weren’t transplanted, were they?” Snyder says, “Actually, yes, they were.”
He continues, “Sometimes, the only potential for a lung transplant that’ll save someone’s life, or other organ transplants for that matter, is to take risks with some not-so-healthy organs.”
A healthy organ combined with a good match is rare enough to be considered a “miracle,” he reminds us.
A man standing against the back wall pipes in. “As recipients, we can certainly identify with that. If I’m knocking at death’s door and you can buy me two years with those lungs, I’ll take them.”
∗ ∗ ∗
On a warm Friday in June, three weeks after the volunteer education meeting, the large conference room at Lifesharing has been set up for another meeting, this one more intimate, with only six people (the two parents of a donor, the recipient, two Lifesharing staff members, and myself) expected to attend. Two white coffeepots sit at one end of the oblong table, next to a platter of coffeecake squares, a small stack of paper cups, and three boxes of Kleenex.

Katie and Thom Wilson sit at one side of the table, awaiting the arrival of the woman who, eight years ago, received the pancreas and kidney of their 16-year-old son Matthew. Monica Cunningham is already crying when Bell leads her into the conference room. Both Thom and Katie stand. Monica heads straight for Katie, and sobs in her arms for a long moment, before she pushes herself away and apologizes. She cries again in Thom’s arms.
Once everyone is settled into a seat, Monica and the Wilsons swap stories about Monica’s illness and Matthew’s death. They hone in on coincidences (both Monica and Matthew had collections of stuffed animals, both were avid Bible readers) and say things like “It must have been ordained by the ‘man upstairs.’”
This meeting has been eight years and six months in the making, put off originally by the Wilsons, who were not ready to go through with it, and then postponed several times due to the illness of Monica’s mother, who passed away two weeks ago.
Nationally, Ross informed me minutes before this meeting, less than 5 percent of all transplant cases result in a meeting between donor family and recipient. In San Diego, she says, the percentage is “only slightly higher,” and Lifesharing oversees “maybe four [donor/recipient meetings] per year.”
Two months ago, during our first meeting at the Pineda family home, Letty Silva told me she believes the low number of donor/recipient meetings is due in part to the necessary precautions Lifesharing takes to maintain confidentiality. Michael McCrerey agreed. They both cited personal experience as evidence.
At one time, Lifesharing required that, before writing a letter to a donor family, the recipient had to wait at least a full year after the transplant. The purpose of this was to give the family time to grieve and the recipient time to heal. Today, some meetings take place as soon as a month after the transplant surgery, though Lifesharing suggests waiting at least six months.
The organization keeps all contact information confidential. When either a donor family or a recipient want to reach out, they write a letter and send it to the Lifesharing office for review before the organization sends it to its intended recipient. The response letter, too, must be sent through Lifesharing.
“The steps are there for a reason,” Letty says, “but with all those steps, you run the risk of losing letters.”
Michael wrote his letter to Mario’s family in January of 2008. It was only by chance that Letty found the letter in Mario’s apartment eight months later, when she went to retrieve the refrigerator Mario had purchased shortly before his death. The letter was in a Lifesharing envelope and addressed to Mario’s young wife, who had emptied out the apartment and lost contact with his family shortly after his death. Curious, Letty opened it and responded soon after.

In November 2008, Rita and Michael met Letty, Lupe, Gloria, Nena, four of Mario’s six siblings, and two of their husbands. The newly acquainted families, who would forge a lasting friendship, shared stories and, like Monica and Thom and Katie Wilson, toyed with questions of coincidence and fate. The story that continues to thrill Rita, Michael, and Mario’s sisters is about how, prior to receiving Mario’s liver, Michael had no taste for Mexican food.
“When we left the hospital after his transplant,” Rita explained, “we jumped on the 52, and I asked, ‘What do you want to eat?’ He says, ‘I want Mexican food.’ I thought he was humoring me, since that’s one of my favorite food groups. This was before we knew anything about where the liver came from. The next week, we’re driving down the freeway, and I say, ‘What do you want to eat?’ and he says, ‘Mexican.’ I thought I’d died and gone to heaven.”
Michael nodded. These days, he eats Mexican food at least three times a week.
You can sign up for organ donation online at register.donatelifecalifornia.org/register/.


Michael McCrerey wanted to die at home. In the four years since he’d been diagnosed with liver disease, he’d been hospitalized at least a dozen times (six in the past 12 months), his abdominal cavity had been flooded with toxic fluid, and he’d shrunk from a beefy six-foot-four, 225-pound hunk of a man to a sack of bones weighing 135 pounds.
Michael’s wife Rita documented the whole ordeal. In the living room of his donor Mario Pinedo’s childhood home in National City, she heaves a large white binder into her lap, opens it, and flips to a picture of her husband at Scripps Green Hospital. Though Michael was 62 at the time, the combination of his sunken cheeks, the wheelchair, and the hospital gown ages him a good 25 years. When Rita passes the picture around the room, three of Mario’s sisters marvel at the difference between the Michael in the picture and the Michael sitting now in a chair against the far wall, beefy and healthy again, a somewhat bored look on his face.

“We got married in 1973,” Rita says. “Fool that I am. I should’ve read the fine print.”
The women laugh. The corner of Michael’s mouth twitches, but he doesn’t smile.
In 1977, after 11 years as a California Highway Patrol officer, Michael was forced to retire at 33 due to an on-the-job injury — a herniated disc. He had always wanted to be a policeman, and the retirement “pulled the carpet from under him,” Rita says. So he took to golf and scotch.
“We always liked our cocktails,” Rita says with a smirk. “Back in those years, they were doing lots of happy hours, and you could practically go have dinner with the hors d’oeuvres and that kind of thing. So he wound up having liver disease because he fell into the habit of drinking a lot.”
The average human liver weighs 2 1/2–3 1/2 pounds. The largest solid organ in the body, it performs essential functions, including detoxification of the blood and the metabolization of fats and proteins. In October 2002, Michael received his first diagnosis of cirrhosis, a disease in which scar tissue replaces healthy liver tissue, resulting in the liver’s inability to function. Cirrhosis is not reversible, and Michael’s doctor told him it was likely he would one day need a transplant. While Rita initiated the process of obtaining referrals and taking other necessary steps to get him on the transplant list, Michael went from sick to sicker, eventually developing ascites.
“[Ascites] is when your liver’s not processing the bile or liquid that it’s supposed to be processing to get your bloodstream cleaned up, so it oozes out and becomes liquid in the cavities,” Michael explains from across the room. “It balloons your stomach right out to where it looks like you swallowed a beach ball. I mean, huge and tight.”
Several times, the fluid caused Michael’s lungs to collapse.
“See. This is what his stomach looked like,” Rita says. She flips to a picture of Michael, ancient-looking and skinny, save for the giant stomach. “We went in, and they take a nice, big, long needle, poke it in your gut, and drain out the fluid.”
The first time the doctors drained Michael’s fluid, they told him he’d probably be in again in a month, and then again the month after that. But it would be another 14 months before he had to be drained again. Later, however, as his illness progressed, he went to Kaiser’s Otay Mesa gastroenterology department every Tuesday, and each time, the doctors drained 20–22 pounds of liquid from his body. That’s the equivalent of three to four two-liter bottles of soda. Every week.
“They’d suck it all out of there,” Rita says, “and when he’d come out, of course, [his stomach] would be all flat.”

Michael sits stoically, nodding every now and again. Rita’s women friends raise their eyebrows and shake their heads in sympathy. Rita doesn’t have the patience for boo-hooing, though. Once, when faced with a condescending Kaiser administrator who said something to the tune of “I know you love your husband, but there’s nothing I can do,” Rita replied, “Don’t give me that ‘woe is me, poor little wife’ stuff. This is business.” And then she proceeded to school him about a thing called “denial of medical care,” for which she would not hesitate to sue if he didn’t find a way to help her husband.
Rita’s binder, her facts, and her big silent man are all part of what she calls her “dog and pony show.”
“I’m the dog, he’s the pony,” she says.
Eventually, Michael’s loss of liver function also meant that toxins such as ammonia, which are normally made harmless by the liver, began to build up in his body. This resulted in hepatic encephalopathy, a disorder of the brain that often causes confusion and altered levels of consciousness.
“It’s like your brain waves would say, ‘I’m going to have a cup of tea,’ and then you would do something totally different,” Rita says. “He would use the TV remote and think it was the lamp or the phone.”
Along with the confusion, the encephalopathy also scrambled Michael’s personality.
“One of the special little fun side effects was that he became a secret shopper,” Rita says. “A shopaholic.”
At the time, Rita worked an express mail route for the United States Postal Service. Because she had a flexible manager who allowed her to eat lunch at home, she was able to check on Michael every day. One day, one of her neighbors stopped her and asked if she realized that packages arrived via FedEx, UPS, or DHL at her house almost daily, sometimes two or three boxes at a time. Rita was shocked. She’d never seen any of the packages.
“I was home one day, and I heard the delivery truck, so I hid and kind of watched from by the door,” Rita says. “[Michael] got the item, the delivery guy left, and he closed the door, picked up the box, and went scurrying down the hall to hide it like a damn chipmunk. He hid it in the closet. I didn’t realize that, for a year, he’d been buying things from catalogs and on the internet. Anything that said you’d get something for free, anything like free shipping, it was a trigger for him.”
By the time Rita found out about it, Michael had spent $80,000 on towels, socks, underwear, toaster ovens, comforter sets, shirts and pants, one or two of every color. Over time, Rita did see and question some of Michael’s purchases, but when she asked about them he snapped at her, saying he could buy what he wanted as long as he was paying for it. He used credit cards, and the more he spent, the more credit he was offered by the credit card companies. Michael retrieved the mail before Rita came home. He also hid much of what he bought in his closet, which Rita never looked in, and in the closet of the guest room, and under beds.
“We have ten comforter sets. There are two of us!” Rita says. “We have so many towels and sets of sheets, I had to give hundreds away. And anything with an eagle. He decided he loved eagles.”
“I’d always liked them,” Michael says. “But before then, I’d never had to have them.”
Rita nods. “Yeah. He spent $80,000 on stupid stuff.”
In early 2006, after four years of gathering information and documenting evidence, Rita’s tenacity secured Michael a spot on the transplant list and a contract at Scripps Green. On February 10, he went in for a transjugular intrahepatic portosystemic shunt (TIPS) procedure, in which a bypass relieves the pressure of the fluid going through the liver. Although normally an outpatient procedure, blood infections landed Michael in intensive care for two weeks. During those two weeks, he was a backup for two livers (he was second in line for a transplant — twice), but the infections made him ineligible.
“He was on lots of monitors, and he was always making those alarms go off,” Rita says. “When he was in intensive care, it was like he was a dead guy.”
By that point, Rita and Michael were exhausted and ready to accept Michael’s death as imminent. Against the advice of doctors, as well as her own wishes for Michael to die in the hospital so he could be an organ donor, Rita brought him home and set up a hospital bed in the living room.
“I didn’t want to die in the hospital,” Michael says. “I just wanted to pet my cat, watch the big-screen TV, and die [at home].”
∗ ∗ ∗
A pizza, fruit, and cake buffet has been set up in the fourth-floor conference room at the Lifesharing office on Camino del Rio South. People file into the room, put their bags down on their chosen chairs, and fill their plates. When I sit at the large oval table (it won’t be big enough for the 20-some-odd people who show up for tonight’s meeting) between two women, the one on my left asks, “What do you have?” I don’t understand the question until she explains that she’s had her new liver six and a half years. I inform her I have all my original organs and that I’m here researching an article.
The woman on my right introduces herself as Mary. While she takes the pineapple off her pizza (“Not kosher,” she says) she explains that her new liver came from a 14-year-old boy named Jonathan. She got two thirds of the liver, and the other third went to a baby. That was 21 months ago.
“Jonathan is my angel,” she says.
At 7:00 p.m., Sharon Ross, director of public relations and community outreach at Lifesharing, asks for a round of self-introductions. Five liver, three heart, four lung, and five kidney recipients state their names and the length of time they’ve had their new organs. Their time from transplant ranges from 3 1/2 weeks to 24 years. Rita sits at one end of the table, next to Letty, one of Mario’s sisters, whom I’d met along with two other sisters at their childhood home back in April. Letty represents one of five donor families in attendance tonight.
Rita and Letty also represent Lifesharing’s current volunteers. They’ll share their experiences with those who have come to learn about volunteering their time with the organization.
Lifesharing is the sole organ-procurement organization for San Diego and Imperial counties, a population of nearly 3.5 million people. This means that every organ transplanted in this area is recovered by Lifesharing.
A total of 58 such organizations exist across the country, 4 in California. All are federally designated, and each is a member of the United Network for Organ Sharing (UNOS), which allocates distribution of organs across the country.
Though it is a commonly held belief that there is one waiting list per organ, and that each organ is flown to wherever the patient at the top of the list happens to be, the list shifts and changes each time an organ is made available. When organs are identified, the procurement organization enters information about the organs into the UNOS computer system and runs the match program. The list of criteria that puts a patient at the top of the list include the matching of organ characteristics (size, blood type, tissue type), medical urgency, time on the waiting list, and distance from donor.
The shortage of available organs, which causes people to use terms such as “miracle” and “hero” in the world of organ donation and transplantation, is due to the fact that it is the particular circumstances of death that make a person eligible to be a donor. Only brain death and cardiac death qualify. In the days before the advancement of legal definitions for brain death, all organ recovery used to be from cardiac death, though that’s now less common. As many as eight organs can be recovered after brain death; after cardiac death, often only the kidneys and liver are recoverable. Of the more than 2 million deaths in the United States each year, less than 1 percent are brain deaths.
Once a hospital patient has been identified as a potential donor, the hospital staff contacts Lifesharing. They send out a “first responder” to evaluate the medical and social history of the patient and follow along as doctors perform tests to confirm brain death.
Billy Snyder, a Lifesharing organ procurement specialist, relates brain death to pregnancy.
“Either you’re pregnant or you’re not. Either you’re brain dead or you’re not,” he says. “There’s no wiggle-worming gray area. When someone’s brain dead, they have complete cessation of their entire brain system and all those functions that go along with it: respiratory drive, pupillary response, cornea response, any pain response, any receptor in the body.”
After brain death has been declared, Lifesharing first tries to place all organs locally. Today, over 1600 people in San Diego are waiting for organ transplants. Because the length of time an organ can live outside the body differs, the allocation varies. For example, hearts and lungs tend to stay local because they have only four or five hours of viability. Kidneys, on the other hand, can last as long as 48 hours with the use of a perfusion pump, which stimulates optimal body function for the kidney and increases the success of its transplant. If someone on the list is a perfect match, that kidney will bypass local transplant centers because it has the best chance of functioning in the body of a person with “zero mismatch.” In other cases, if Lifesharing can’t find a suitable match for organs in San Diego, they expand the search to Los Angeles, Northern California, Arizona, Nevada, and so on.
∗ ∗ ∗
Outside the doors of the conference room, past the reception desk, a narrow hallway leads to the Lifesharing staff offices. The walls of this hallway are hung with five “donor quilts,” each bearing 20 squares dedicated to the dead, whose organs and tissue live on in the bodies of strangers like those around the conference room table.
Crystal, We miss you is embroidered in white thread on a red square.
Sarah Elaine Schonhoff is stitched in green above a picture of a smiling, thin-haired baby, along with the dates 1-21-2004 and 2-10-2006.
The right half of the backside of a pair of jeans (including belt loops to just below the pocket) fills the square next to little Sarah’s. Poker chips and pictures of dice, running shoes, and a tool belt create a collage of significant mementos, along with the words “husband” and “father” spelled out in tiny Travel Scrabble letters.
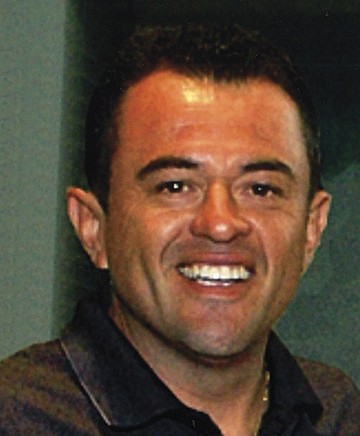
Mario Gerardo Pinedo does not yet have a quilt square. The 39-year-old owner of a National City auto-detailing shop died of a massive brain aneurism in 2006, and his sister, Letty, who sits next to Rita at the Lifesharing volunteer meeting, says the square is something she and her four sisters have been meaning to get around to. During a recent conversation, they did come to a couple of decisions. They want a Chargers background, and something about the Padres, for sure — maybe a picture — and also, perhaps, a couple of lines about Pinedo.
In July 2005, a few days before his 39th birthday, Mario went to the Chula Vista DMV to renew his driver’s license.
“They asked him if he wanted to be an organ donor, and he said yes,” Letty said on the evening we sat together with Rita, Michael, and two of Mario’s other sisters in the Pinedo siblings’ childhood home. “He comes home all excited because he was going to be a donor. My parents were telling him, ‘Are you crazy? You’re 38 years old. What are you thinking?’ And he was, like, ‘When I die, what are they going to do with it? Everything’s going to turn into a worm. I’m going to be eaten up. No. I’m going to give it to somebody. You never know, Mami. You never know whose life you can save.’”
Seven months later while at a Friday-night barbecue, Mario suffered a massive brain aneurism and was admitted to Scripps Chula Vista Hospital around 10:00 p.m. Two days later, he died.
“We all ran to the hospital, though my parents weren’t here. They were in Mexico,” Letty says. “Pretty much right away, [the doctors] told us he was brain dead. At that point, it wasn’t even what are we going to do, it was how are we going to tell our mom, and who’s going to make that call?”

It was at this point that Belen Bell, family-services specialist at Lifesharing, introduced herself to the Pinedo family. The now 57-year-old Bell, fond of brightly colored sweater sets, establishes and maintains eye contact when she explains her job to me one afternoon in another, smaller conference room. It’s been a week since the volunteer meeting.
Although Bell has several responsibilities, one of them is to obtain consent from family members for the procurement of organs. She had been at the hospital following Mario’s case but did not approach the family right away.
“We follow from a distance,” she says. “We check their labs, and we check their neurostats, to see if they’ve worsened or gotten better. We don’t go near the families until the right moment. Never do we want a family to feel that we’re hovering.”
Once a family has been informed by physicians that their loved one is brain dead, they need time to grieve, Bell says.
“What we normally listen for is ‘What is our next step? Should we be looking for a funeral home? What should we do now?’” she explains.
In the case of Mario Pinedo, this happened around 5:30 on Saturday morning, when his sisters began to discuss how they were going to tell their parents that Mario was gone. The first thing Bell did after introducing herself to Mario’s family was to ask after his mother. When his sisters informed her that their mother was in Mexico and didn’t yet know what had happened, Bell told them to call her and tell her that he was ill, not that he was dead, so she wouldn’t go into shock before the long trip home. Bell then helped the sisters decide who would drive to Tijuana to pick their parents up from the airport and drive them back into San Diego.
“She was our savior,” Letty said of Bell during our meeting at the Pinedo home. “We didn’t even look at the doctors. Belen knew all the medical lingo. If we had a medical question, we’d ask her, and in layman’s terms she would tell us what it was. She also spoke Spanish, and maybe that’s one reason why we identified with her.”
Bell’s Spanish was, in fact, the impetus for establishing the family-services department at Lifesharing. Back in 1994, when she was a translator at the Palomar Trauma Center, her current boss came to Palomar as a Lifesharing nurse to ask a family for consent. She needed Bell’s assistance to navigate the Spanish-English language barrier. Bell, daughter of a German mother and a Mexican father, was born in Venezuela, raised in Spain, and had been translating at Palomar for several years.
“At that time, our Hispanic consent rate was atrocious,” Bell says. “Very, very few Hispanic families would ever consent.”
In 2004, before Bell joined the team, the Hispanic consent rate in San Diego was 42 percent; by 2010, it had risen to 71 percent.
Even after Bell explained to Mario’s family that he had the pink dot (on top of the plastic) on his license, his parents took some convincing. Letty believes this was due in part to cultural and religious beliefs that the body must remain intact for burial.
Mario’s sister Lupe says, “I think they thought they’d give him back to us in pieces.”
To be fair, this was two and a half years before Pope Benedict XVI encouraged organ donation, when he stated publicly: “The act of love which is expressed with the gift of one’s vital organs remains a genuine testimony of charity that is able to look beyond death so that life always wins.”
It is also a common myth (one that Lifesharing staff must debunk frequently) that organ donation delays funeral plans and affects the open casket.
On Sunday, February 26, 2006, Mario’s parents gave Lifesharing their consent to donate Mario’s organs. “Everything but his pretty green eyes,” Letty says.
That same day, Michael McCrerey received a call from Scripps Green. “It’s time,” they said. “We have a liver for you.”
∗ ∗ ∗
When Billy Snyder meets new people at barbecues, parties, and bars, he dreads the inevitable “What do you do?” portion of getting-to-know-you chitchat. It’s not that he doesn’t enjoy talking about his work. But when people find out that he’s an organ-procurement specialist, responsible for recovering and transporting organs from the newly deceased to the sick and dying, he usually ends up in a 15–20-minute conversation far removed from party-friendly small talk.
Snyder has been at Lifesharing for nearly a decade, in both organ and tissue recovery. He has also worked as an embalming apprentice and a prep assistant at Greenwood Mortuary, and, at age 19, as a “body snatcher” (picking up bodies from crime scenes and traffic accidents) for the medical examiner’s investigator. Although he’d always planned to become a San Diego police officer like his father, who was on the force for 30 years, Snyder says he “fell in love with the death industry,” during his time with the medical examiner.
“It’s fascinating what happens to the body after death,” he says. “All aspects of it. The decomposition process, the trauma aspect of the body, and then also organ and tissue donation.”
Some of what Snyder says would sound macabre coming from almost any other source. But this clean-shaven 30-year-old surfer dude wears a 3/4-sleeve tattoo of chrysanthemums and lilies on his left arm, has a medical vocabulary to beat the band, and, somehow, his fascination with the science of death sounds no crazier than a fascination with, say, horticulture.
Even now, standing (sleeves rolled down, tattoos covered) in a roomful of organ recipients, where he’s encouraged to speak freely about his work, Billy Snyder is so full of energy and information that, after a while, even his graphic photographs of purplish hearts and shiny livers begin to look less horrifying and more…interesting.
When he says, “Lungs are truly one of my favorite things to come out of the body, no offense to any other recipients here” — then points to a photograph he’s taken of actual lungs and says, “Those are beautiful lungs” — I can’t see beyond the fact that they’re internal organs (and therefore gross). I wish I could.

Snyder’s job as part of Lifesharing’s surgical services team begins in the hours between consent and the organ-procurement operation. Once he’s been called in, he gathers his equipment and supplies (organ-preservation solution, instrumentation, organ-packing supplies, paperwork, etc.) and heads to the hospital where the donor has been kept “alive” on a ventilator. He stops first in the operating room, where he checks in with the charge nurse to get the details about who will be on the surgical team. Then he visits with the Lifesharing nurse to get a rundown on the donor. By this point, a recipient has already been found for each available organ, and transplant teams have been called. Once all the surgeons arrive, Snyder acts as coordinator, gathering them and relaying all pertinent medical information. When he says “pertinent,” he means “Everything. It’s a summation of how this [donor] ended up where he is.”
Tonight, at the volunteer meeting in the Lifesharing conference room, Snyder’s PowerPoint presentation consists of 18 slides, only one of which contains words. The rest are photographs Snyder has taken from the operating room. He’s held nothing back. A close-up shot of a midline incision shows a pair of metal clamps holding the body open, revealing lumps of shiny, purple, and veiny organs.
“Remember, this patient is on a ventilator,” Snyder says. “So you’re actually watching this heart beat inside this person and watching the lungs breathe. You can run your thumb over the liver and guesstimate what the fat content’s going to be after you flush the blood out.”

Another shows a crowd of scrub-mask-and-glove-clad doctors standing over a gaping abdominal cavity. Sometimes, Snyder tells us, there can be as many as 25 people in the operating room: surgeons, scrub technicians, anesthesiologists, nurses, and fellows or med students. All of them work “in symphony,” he says, “to free the organs from their anatomical structure, with the exception of vasculature.”
After the midline incision is made, usually by the heart surgeon, the abdominal cavity is packed with sterilized ice (also called “slush”), and each transplant surgeon cross-clamps, to cut off blood flow, and cannulates (running an IV-like tube into) the organ he or she is responsible for extracting. Through those tubes another cold preservation solution (modified for each organ) flushes each organ of blood and cools it from the inside. The organs are taken out of the body in the same order each time, beginning with the heart, which can last outside the body four or five hours. At most.
“From the time that cold solution starts flushing, the clock starts ticking,” Snyder says.
Inside the operating room, Snyder often plays the role of perfusionist (or preservationist) assisting one of the transplant surgeons with the flushing of an organ. He also sets up the back table where, as each organ is removed, it is measured, and occasionally biopsied, to help doctors understand how it’s going to function when transplanted. Snyder helps with documentation, and if necessary, executes “a little extra flush,” of the organ.
Then, as each organ is readied, it’s packed up using procedures that are, like all parts of the transplantation process, regulated by the United Network for Organ Sharing. Although there are some variations per organ, all are immersed in a “storage solution” (same as or similar to the solution with which they’re flushed), packed with a “triple sterile barrier,” or three closed sterile bags, then stored on ice in a cooler, and labeled. Each organ is then delivered to the transplant program either by courier, by the surgeon, or sometimes by Snyder himself.
“The heart does not leave our hands,” Snyder says. “Because of the small window, it goes [directly] from the patient to the back table, where it gets packaged up quickly, and then rushed off to the awaiting operating room. Same thing with lungs and livers. Pancreas, generally the same thing, too. But with kidneys, we can put them on a machine that will pump them, which increases the amount of time that they can stay out of the body.”
Snyder shows photographs of each organ in the same order that it comes out. After the heart come the lungs, then liver, pancreas, and kidneys. He has healthy and not-so-healthy photos of each. Some people murmur oohs, ahhs, and hmms at the pictures, perhaps wondering what their own look like.
At one point, he shows a photo of a pair of lungs that have been blackened (yes, they are indeed black) by 30 years of pack-a-day smoking. When someone asks, “Those weren’t transplanted, were they?” Snyder says, “Actually, yes, they were.”
He continues, “Sometimes, the only potential for a lung transplant that’ll save someone’s life, or other organ transplants for that matter, is to take risks with some not-so-healthy organs.”
A healthy organ combined with a good match is rare enough to be considered a “miracle,” he reminds us.
A man standing against the back wall pipes in. “As recipients, we can certainly identify with that. If I’m knocking at death’s door and you can buy me two years with those lungs, I’ll take them.”
∗ ∗ ∗
On a warm Friday in June, three weeks after the volunteer education meeting, the large conference room at Lifesharing has been set up for another meeting, this one more intimate, with only six people (the two parents of a donor, the recipient, two Lifesharing staff members, and myself) expected to attend. Two white coffeepots sit at one end of the oblong table, next to a platter of coffeecake squares, a small stack of paper cups, and three boxes of Kleenex.

Katie and Thom Wilson sit at one side of the table, awaiting the arrival of the woman who, eight years ago, received the pancreas and kidney of their 16-year-old son Matthew. Monica Cunningham is already crying when Bell leads her into the conference room. Both Thom and Katie stand. Monica heads straight for Katie, and sobs in her arms for a long moment, before she pushes herself away and apologizes. She cries again in Thom’s arms.
Once everyone is settled into a seat, Monica and the Wilsons swap stories about Monica’s illness and Matthew’s death. They hone in on coincidences (both Monica and Matthew had collections of stuffed animals, both were avid Bible readers) and say things like “It must have been ordained by the ‘man upstairs.’”
This meeting has been eight years and six months in the making, put off originally by the Wilsons, who were not ready to go through with it, and then postponed several times due to the illness of Monica’s mother, who passed away two weeks ago.
Nationally, Ross informed me minutes before this meeting, less than 5 percent of all transplant cases result in a meeting between donor family and recipient. In San Diego, she says, the percentage is “only slightly higher,” and Lifesharing oversees “maybe four [donor/recipient meetings] per year.”
Two months ago, during our first meeting at the Pineda family home, Letty Silva told me she believes the low number of donor/recipient meetings is due in part to the necessary precautions Lifesharing takes to maintain confidentiality. Michael McCrerey agreed. They both cited personal experience as evidence.
At one time, Lifesharing required that, before writing a letter to a donor family, the recipient had to wait at least a full year after the transplant. The purpose of this was to give the family time to grieve and the recipient time to heal. Today, some meetings take place as soon as a month after the transplant surgery, though Lifesharing suggests waiting at least six months.
The organization keeps all contact information confidential. When either a donor family or a recipient want to reach out, they write a letter and send it to the Lifesharing office for review before the organization sends it to its intended recipient. The response letter, too, must be sent through Lifesharing.
“The steps are there for a reason,” Letty says, “but with all those steps, you run the risk of losing letters.”
Michael wrote his letter to Mario’s family in January of 2008. It was only by chance that Letty found the letter in Mario’s apartment eight months later, when she went to retrieve the refrigerator Mario had purchased shortly before his death. The letter was in a Lifesharing envelope and addressed to Mario’s young wife, who had emptied out the apartment and lost contact with his family shortly after his death. Curious, Letty opened it and responded soon after.

In November 2008, Rita and Michael met Letty, Lupe, Gloria, Nena, four of Mario’s six siblings, and two of their husbands. The newly acquainted families, who would forge a lasting friendship, shared stories and, like Monica and Thom and Katie Wilson, toyed with questions of coincidence and fate. The story that continues to thrill Rita, Michael, and Mario’s sisters is about how, prior to receiving Mario’s liver, Michael had no taste for Mexican food.
“When we left the hospital after his transplant,” Rita explained, “we jumped on the 52, and I asked, ‘What do you want to eat?’ He says, ‘I want Mexican food.’ I thought he was humoring me, since that’s one of my favorite food groups. This was before we knew anything about where the liver came from. The next week, we’re driving down the freeway, and I say, ‘What do you want to eat?’ and he says, ‘Mexican.’ I thought I’d died and gone to heaven.”
Michael nodded. These days, he eats Mexican food at least three times a week.
You can sign up for organ donation online at register.donatelifecalifornia.org/register/.