 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

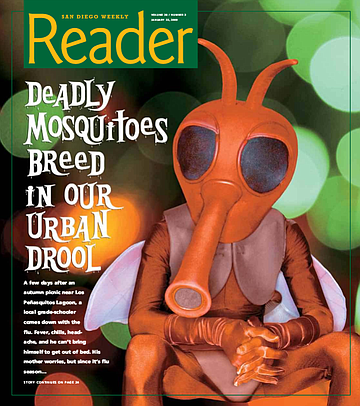
A few days after an autumn picnic near Los Peñasquitos Lagoon, a local grade-schooler comes down with the flu. Fever, chills, headache, and he can’t bring himself to get out of bed. His mother worries, but since it’s flu season…
Three days go by. The boy doesn’t seem to be getting any better. The mother begins to worry more. She wonders whether she should make an appointment at the doctor’s.
The next morning, the little boy is lying in bed with a blank stare. He’s unresponsive, and the mother panics, calling 911. The boy suddenly begins to talk about algebra and dinosaurs and baseball, all in the same garbled sentence. Then he doesn’t recognize his mother.
At the hospital, the doctor knows the symptoms. He’s seeing more cases like this one lately. He runs a blood test. Sure enough.
West Nile virus.
In the past, there were never more than 15 human cases of West Nile virus in a calendar year in San Diego County. So far in 2008, we’re at 23 cases, and climbing. Since the disease is often fatal to birds, dead birds are a sure sign that West Nile is around. Before this year, the highest number of birds that tested positive in a calendar year was 162. This year? Over 500. Four horses in the county are dead from the disease. Of the 40 “sentinel chickens” used for early detection, 13 have converted to West Nile, including all 10 in Los Peñasquitos Lagoon, 2 in Oceanside, and 1 in the Tijuana River Valley. In the past, no more than 1 chicken had converted. Of the 240 batches of mosquitoes that have been tested by the Department of Environmental Health, 37 are positive for West Nile, a higher percentage than ever before. In fact, we’ve never had more than 7 positive batches of mosquitoes in the past.
“West Nile virus is vectored from the bird world to the human world by mosquitoes,” says Chris Conlan, supervising vector ecologist for the Department of Environmental Health. “And this year has been worse by major magnitudes.”
THIS PARK IS CLEAN
A few hundred yards past the entry to Rose Canyon Open Space Park, along a dirt road off Genesee Avenue, Mary Dice spots a swollen area in a creek. “Standing water,” she says, stopping her white Department of Environmental Health truck. “It’s moving at this end and at that end, but there’s stagnation in the middle.”
Dice climbs out of the cab, heads around back, and pulls from her gear what looks like — and, as it turns out, is — a golf club with a ladle soldered onto where the head of the club should be.
“Golf courses have a lot of water features that need to be treated,” Dice says. “So once we get to know the guys, we ask for some of their old clubs. And then we saw off the head and solder a ladle on instead — voila!” She laughs, brandishing the handy tool. “High-tech mosquito-control instrumentation.”
Dice, 57, is a wiry, outdoorsy-looking woman with short, gray hair. A senior technician for the Department of Environmental Health, she’s worked there for over 18 years.
Dice’s department treats public lands — rivers, creeks, ponds, sewage spills — in an attempt to eradicate disease-carrying creatures such as rats and mosquitoes.
“Mosquitoes lay their eggs in standing water,” Dice explains. “It takes about a week, depending on temperature, for the eggs to hatch. The larvae go through four growth stages for the next week or so, before they turn into pupae. Then the adult mosquito emerges from the pupa and goes out looking for a blood meal.”
So the best way to find hundreds of mosquitoes in one place is to seek out their breeding grounds.
“Moving water actually drowns the larvae,” Dice says. “They have a siphon on their back ends, and they have to breach the surface with that siphon and take in oxygen on a regular basis. If the water’s moving a lot, then they’ll have to use more energy than they can take in. That’s not what larvae do. They rest up, and then go after food, and then they rest again. So that’s why mosquitoes lay their eggs in standing water.”
At least 25 species of mosquito live and bite in San Diego County. Only 4 species carry West Nile, but the others need to be watched as well, according to Dice. “At this time,” she says, “we don’t have dengue fever here. But it’s become common in Mexico and Texas, so we’re on the lookout.”
Dice and 14 other vector-control technicians are assigned to different areas in the county for monitoring and treatment. “We’re responsible for all the known sites in our areas,” Dice says, “and we’re responsible for finding additional sites. We try to make sure that the larvae aren’t around long enough to become adults and then fly off and bite people.”
Dice covers “five Thomas Guide pages” in her area, from just east of the Department of Environmental Health office on Hazard Way, near Tierrasanta, all the way to the coast, then north to Del Mar and south to Mission Bay Park. Her jurisdiction encompasses roughly 150 natural mosquito-breeding sites.
But lately, this area has also begun to include hundreds of algae-filled swimming pools that require treatment as well.
“This year’s been just hellacious,” Dice says. “And it’s mostly because of all the foreclosures. I mean, there must have been thousands of green swimming pools that we treated.”
The county health department has even started using its helicopter to spot potential mosquito pools in backyards.
“People are usually pretty surprised when we show up at their front door with a picture of their pool.” Dice chuckles. “But we operate on the principle of helping people. So if you have a green pool, and our helicopter spots it, and I find your house, then I’m not there to give you a lecture or citation or problem. I’m there to help you. If your pool filter’s broken, and you’re looking at thousands of dollars of repairs, and you can’t do it, we’ll be happy to provide you with mosquito-eating fish, and we’ll put them in your pool for you, and we’ll give you a card with a number to call if your fish die off for any reason. Or if you’re getting your pool repaired, then we’ll come fish them out and use them elsewhere.”
A tank full of these little glittery fish is the first thing you see upon entering the front door of the Environmental Health building on Hazard Way. The little surface-breathing Gambusia affinis are found naturally in the county, and Dice has fish traps in the back of her truck to catch them whenever possible. “If I’m at a site that has some, then I’ll set a trap there and head back at the end of the day to take them back to the office. They’re hard workers, and they work cheap,” she jokes. “They don’t have a union.”
Dice dips her golf-club ladle into the edge of the swollen area of Rose Canyon Creek, lets some water eddy in, and then lifts the ladle toward her face, looking for larvae. She dumps the water and checks twice more at different spots along the edge. “I’m not finding any larvae here,” she says. “And that’s a good thing. That’s encouraging.”
Dice and the other technicians in her department have been pushing themselves to hit as many potential breeding sites as possible, as often as possible. They drive around all day in their white Ford Ranger trucks.
But helicopter drops are also used to get to places that are unreachable from the ground, such as large standing ponds socked in by thick vegetation. Every three weeks during the height of the mosquito-breeding season, from June through September, the Department of Health’s single helicopter will head into the air.
“We use it where we need it,” Dice says of the helicopter, noting that each time it goes up, it costs the county taxpayers about $5000. “But, by golly, if you can squeeze in there and get the job done, then you should squeeze in there and get the job done.”
But many of the mosquitoes in the area come from places much closer to home, even “small sources in our own backyards,” Dice says. “A watering can that you’ve forgotten about, or plant saucers. Without some knowledge about it, you’d have no idea to look there for mosquitoes. A lot of people have no idea that mosquitoes have an aquatic larval stage before they progress to adults.”
Joggers and dog-walkers pass by periodically in the Rose Canyon morning light. After a few more stops along the path, checking with her golf club ladle, Dice determines that the park is clean. “I used to have to hike entire canyons through thick brush,” Dice says. “But now I can mentally trim areas down to their standing water and just pull up at specific spots.”
She climbs back into her truck and drives out to Genesee Avenue, heading toward Pacific Beach. “I have some street gutters holding water in Pacific Beach, near the military housing behind Mission Bay High School. “It’s an area I watch pretty closely, because we’ve had a higher rate of bird mortalities there lately.”
Dice has a host of weapons in her arsenal when mosquitoes are discovered.
In the back of her truck, along with the golf-club ladle and wire-mesh traps for catching mosquito-eating fish, Dice has an old-style B&G tank of Golden Bear Oil, a powerful pesticide that she hates to use. “It’s the only thing that will kill pupae,” she says. “It’s a suffocant. It lays on the surface of the water. It’s a short-lived product, but while it’s there, it kills all the other aquatic insects at a site. It’s very sad because I particularly like dragonflies and damselflies.”
But Dice hardly ever resorts to using the Golden Bear Oil. She has much safer products locked inside a large, black, rubber trunk in the back of her truck. It just so happens that this trunk is covered with multiple images of skulls and crossbones.
“It’s just the law that we mark it that way. But there’s no poison in there. It’s just full of Bti and growth inhibitor.” Bti stands for Bacillus thuringiensis israelensis. It refers to any bacterial product that controls pests.
Dice explains, “Originally, it was a mosquito product that was discovered in Israel in the early ’80s. One year, they went out to control the mosquito larvae, and there were none. And they noticed that the leaves on the corn plants had developed some type of problem, and they were dropping off into the water. And corn plants don’t normally drop their leaves. So they looked closer, and they found a particular bacteria that affects only the gut of mosquito larvae. So now when I put VectoLex or another Bti product out into the water, I feel good about it, because I know it’s only going to affect the mosquito larvae. If a coyote wants to come by five minutes later and have a drink of water, it’s not going to affect him.”
VectoLex is ground-up corncob impregnated with bacteria specific to the gut of mosquito larvae.
Dice remembers testing the first Bti’s 25 years ago, and after she sprinkled some in a pond, a flock of ducks flew down and ate it up just as fast as she could spread it out. “At first I thought, ‘Oh, no!?f I was used to pesticides, and here these ducks were eating this stuff.”
The ducks were pets, and they were subsequently observed for adverse effects. “They were fine,” says Dice. “And after that, I felt relieved to have this product. Not to mention, but 24 hours later we came back, and there wasn’t a single mosquito larva living.”
Thanks to the successful development of Bti’s, the county hasn’t sprayed pesticides in over 16 years, according to Dice.
Another weapon in Dice’s arsenal is a growth-inhibiting hormone called Methoprene. This slow-acting insecticide prevents eggs and larvae from developing into adults, so that the mosquitoes die in arrested stages of immaturity. Methoprene has no effect on adult mosquitoes, however.
“Methoprene works long-term,” says Dice. “And if you’re regulating sensitive areas, or areas that are difficult to get to, you want to use a long-term product.”
GETTING TO KNOW YOUR “BUGS”
PART ONE
Mosquitoes are attracted to carbon dioxide. They also seem to be more attracted to some people than others, but no one knows whether this is because of personal chemistry or diet or cologne or blood health. Without a doubt, mosquitoes possess a higher level of natural awareness than humans can understand.
“A mosquito will land in a dry spot,” says Dice, “and she’ll know that water will return. And she’ll put her eggs there in a dry area, knowing that it will fill with water soon.”
Some mosquitoes are day-biters, but most feed from dusk until dawn. The first thing on a female mosquito’s mind is blood. She needs a blood meal to procreate.
Male mosquitoes lack the saberlike proboscis of the female and are harmless to humans and animals. The males eat only nectar.
“Female mosquitoes fill their stomachs with blood,” Department of Health supervising vector ecologist Chris Conlan explains. “When a mosquito finishes her meal, she’s loaded. It’s a big, red abdomen full of blood. And at that point, she’s going to go off and find a nice, quiet corner to rest. And she’ll spend two or three days converting the protein in that blood meal into eggs. At some point during that time, of course, she’s mated with a male, and that happens pretty quick, and she can store sperm from the male. So she really only has to mate once. And once she’s done all that, then she goes on a hunt to look for a nice place to lay her eggs. The whole process might take about four days, give or take, and then it starts all over again. Theoretically, under the best of all possible circumstances, a mosquito can lay a hundred or so new eggs every four days.”
And each mosquito will continue to eat and ripen eggs and lay them for five or six blood meals or more, depending on temperature, food availability, and, of course, whether or not it can avoid being slapped in mid-meal.
Most mosquitoes only live for a couple of weeks, but Conlan says that some will buck the odds and hibernate through a winter. “The mosquitoes that live longer are a greater risk for disease transmission,” says Conlan, “because they may have picked up an infection somewhere along the line that’s finally incubated long enough that they can transmit it to whatever else they bite.”
GETTING TO KNOW YOUR “BUGS”
PART TWO
Ever since he was in medical school at UCSD 20 years ago, Dr. Dale Lieu has been fascinated by “bugs and the drugs that kill them.” Although, when Dr. Lieu says “bugs,” he doesn’t mean mosquitoes, per se. He means viruses, bacteria, and parasites.
Dr. Lieu is a specialist in infectious diseases for Kaiser Permanente Medical Group.
“Like a lot of diseases that mosquitoes carry, West Nile doesn’t hurt the mosquito,” Dr. Lieu says. “And traditionally, it hurts animals a lot more than it hurts people. In a way, you could say that people aren’t the real target; we just kind of get in the way.”
The first time West Nile virus was discovered in the United States was in 1999 near the Bronx Zoo.
“They started having birds die off,” Mary Dice says. “Not their collection, but other birds, crows. And they were kind of confused, and they have an expensive collection of exotic birds to protect, so they got very interested. Because they’d never seen West Nile virus in this country before, the New York health department assumed that some exotic animal from the zoo had imported some disease. That turned out not to be the case. And the zoo collection was never affected. But they helped track it down. They discovered that it was, in fact, West Nile virus.”
Because birds are the carriers of the disease, and they migrate so widely, once a bird becomes a reservoir, then West Nile can go from New York City to Mexico in a week or less.
“West Nile has been sweeping through the country,” Dr. Lieu says, “but the interesting thing is this: Wherever it has peaked, and then the number of cases has started to go down, the virus has never circled back. If you look at New England and New York, where they had a whole bunch of cases seven or eight years ago, in the past couple of years, they hardly had any. And we think both people and the animal community eventually develop immunity.”
But Dr. Lieu is quick to state that we don’t have enough experience with re-exposure to the disease to guarantee that we develop complete immunity. “There’s probably a good chance that people who get it once become less likely to get real sick,” he says. “But we don’t know how protective it is.”
Has San Diego reached its peak?
“There’s no way of telling that,” Dr. Lieu says. “We’re certainly on an upswing, as far as the number of cases. We’ve had 23 cases so far this year, and we had 15 in 2007. But who knows where that’ll stop, or when it will start going down?”
Lieu wears a white lab coat with his stethoscope in his pocket. He expressly does not wear a tie, because it’s “the one article of men’s clothing that we never wash,” and Lieu is nothing if not fastidious. “I think most infectious disease doctors are like that,” he laughs.
Dr. Lieu himself has treated “a few cases” of West Nile virus in the past year. “The most susceptible people are very young, very old, or have compromised immune systems. Only about one in five people who are exposed to the disease actually get sick. And for the majority, they only get a flulike illness: fever, chills, muscle aches, headaches, fatigue. And that starts about three to seven days after the bite. Most people just think they have the flu, and they get better after a week or ten days, and they don’t think much of it. The vast majority are never even checked for West Nile. But about 1 in 100 people who get infected develops encephalitis. And that’s the most dangerous manifestation of West Nile. That’s where the brain tissue itself becomes infected with the virus, and it gets inflamed. And people come in real, real sick.”
What can a doctor do for such a person?
“There’s no specific treatment other than supportive care,” says Dr. Lieu. “If the encephalitis is from herpes or chicken pox, then we’ll use antiviral medication. But if it’s from West Nile, and we know it’s West Nile, then there’s no specific treatment. All we can do is support the person through this period where they’re really sick, protect them from complications, feed them, and hope the inflammation goes away.”
What are the symptoms of having swollen brain tissue?
“Encephalitis can be really scary,” Dr. Lieu says. “People who have it become basically delirious. They’re bonkers. They’re nonsensical in what they’re saying. They’re completely disoriented. It’s clear that they’re mentally impaired. They can’t hold a cogent conversation. Their mind wanders all over the place. They’ll drift between periods of looking like they’re ready to fall asleep and periods of restlessness. They may not recognize family members. There could be a blank stare.”
The encephalitis portion of West Nile will often last for over a week, Dr. Lieu says, and not everyone makes a complete recovery. “You’re talking about brain tissue. And some of that tissue may suffer some permanent damage. When people have serious cases, a lot of them don’t come back completely. They’re thinking they always have some impairment. They may or may not have some neurological deficits, where some parts of their brains don’t work the same way anymore.”
STUDYING THE VECTORS FROM “BUGS” TO “BUGS”
“Mosquitoes are one of the biggest threats that are out there,” vector ecologist Chris Conlan states. “There’s always been some mosquito-borne illness throughout the United States. We used to have some real nasty ones here, like malaria and yellow fever. But because of modernization, and nice living conditions with screens on the windows, and mosquito control, we’ve beaten those diseases back and pretty much pushed them out. The only ones that stayed here tended to stay here at fairly light levels — like equine encephalitis. And they show up every year, but maybe a half a dozen or a dozen people are affected in a bad year.”
Conlan’s tone changes to a slightly higher pitch. “But when West Nile showed up in the United States in 1999, that kind of changed everything. Because now, all of a sudden, we have a new disease in a new land that’s ready to run amok. It’s like having a three-year-old in a candy store. It’s still establishing itself in the environment, and, as a result, we still don’t understand yet just how bad it could end up being. So all of the vector agencies are always kind of in this ‘prepare for the worst and hope for the best’ mode.”
Conlan, a short, squarish man with wavy, graying hair and piercing blue eyes, is a self-professed “bug geek” who started off on his career path by catching butterflies when he was a little kid.
Part of the problem, he says, is that the encephalitis viruses like West Nile are carried around in the bird population. “And we can’t kill all the birds, and not to mention, but birds travel everywhere. So, the best thing we can try to do is to try to control it from the mosquito side. But you can’t get all the mosquitoes either.”
Conlan’s lab in the Environmental Health building on Hazard Way is full of the usual microscopes and test tubes and petri dishes, but it also contains some weird-looking objects.
Conlan heads over to a series of petri dishes laid out on a table. Each labeled dish contains tens, or even hundreds, of tiny mosquito carcasses. “To the naked eye, they all look the same,” Conlan says. “You need a magnifying glass, at least, to tell them apart. But the two that we really worry about here are Culex quinquefasciatus — we call them ‘quinks’ for short — and Culex tarsalis. The quinks are urban breeders, which makes them particularly dangerous. They’re our urban nemesis for West Nile transmission. And the tarsalis is actually called the ‘Western encephalitis mosquito.’ It’s not quite as big of a threat in urban environments, usually, but what we’re finding is, even in urban zones, if someone lets a swimming pool go out of whack, and it turns green, it can breed tarsalis in massive numbers. And the problem with tarsalis is that it will fly a lot farther than the quinks. They might cover a range of two to three miles in some cases.”
As Conlan speaks, one of his colleagues comes into the lab bearing an armful of plastic bags. Inside each bag is a spread-winged dead bird — two crows, a jay, and, in one large bag, a once-majestic red-tailed hawk. On each bag is written where and when the bird carcass was found.
“These are from our bird pickup program,” Conlan says. “What we do to monitor the disease is, while most birds will get the disease and get a little ill, they’ll get over it and go on to live their happy birdie lives, but some species do not. They end up in a plastic bag, and off they go to the vet for testing. So we focus our testing on birds that are likely to die from it — crows, jays, and birds of prey, like hawks and owls. And you have to get them fresh, right after they die, otherwise you can’t test them because the virus degrades too fast.”
If the Environmental Health veterinarian determines that a bird died from West Nile, then Conlan’s team puts a dot on a map and monitors that area to see if a hot spot is developing. “The birds are the best early detection method that we have. We have other methods that we use. We test the mosquitoes themselves, and we also have what we call ‘sentinel chickens,’ which are basically four groups of ten chickens each, strategically located around the county — one in Oceanside, one in the Tijuana River Valley, one in eastern Santee, and one in Peñasquitos Lagoon — and we do a blood test on those chickens every two weeks to see if they’ve developed antibodies to the virus. Because chickens don’t die when they get it. They mount a quick response and get over it in a heartbeat.”
But how does a mosquito bite a bird? How does it get that little proboscis through all those thick feathers?
“It doesn’t,” Conlan says, about to deliver a truly macabre piece of information. “The best place to get a bird is right in the eye. A bird cannot protect its eyes. So, even when their eyes are closed, the mosquito can bite right through the bird’s eyelid.”
One of the tests Conlan’s lab is using involves the bird’s eye fluid because there’s a higher concentration of the virus in the eye than there is anywhere else in the bird.
At another table in the lab, Conlan points to some unusual-looking devices. Mosquito traps.
The traps are made of inexpensive household products available at any hardware store, such as bus tubs, handheld fans, battery packs, and mesh nets. Nothing high-tech about them, but they are effective. The traps are hung from tree branches overnight, and mosquitoes are collected from the catch bags in the morning.
One kind of trap uses dry ice and a high carbon dioxide concentration that draws mosquitoes toward a fan that blows them into a bag. “That one’s for hungry mosquitoes,” Conlan says. “They associate carbon dioxide with the breathing of some creature that’s full of blood.” A second kind of trap — called a gravid trap — attracts pregnant females by using a mixture of foul-smelling water and organic debris that also eventually blows the attracted insects into a bag for later study.
“The mosquitoes are used for testing,” Conlan says, “and we’ll also count the mosquitoes and sort them by species, which helps us understand if there might be a problem going on in one area or another.”
Some nights, in some areas, the traps will come back nearly empty, and sometimes, a single trap will contain “several thousand” mosquitoes.
“We had a case up in Oceanside this summer,” Conlan relates, “where one of our traps was filling up with the bad kind of mosquitoes — Felix tarsalis — but the normal sources that we were monitoring weren’t showing anything. So we ended up finally going door to door, and we finally found a house that had a bad pool behind it, and it was just breeding them like crazy and messing it up for the whole neighborhood.”
To combat this increasingly common scenario, Conlan says, “We’ve got to teach people. Don’t breed mosquitoes, or you’re kind of asking for it.”
THIS NEIGHBORHOOD IS…NOT CLEAN!
“This looks likely as heck!” Mary Dice exclaims. And then says, “Oh, my gosh.”
She’s turned left off Garnet Avenue in Pacific Beach and parked her truck alongside a veritable stream of gutter water. She calls this stuff “urban drool,” and it’s running down Olney Avenue and turning onto Oliver Avenue. Every ten feet or so along this tract of dark water, large brown puddles bulge out from the curb.
“It fills up the low spots on a lot of our streets,” Dice says, “and you’d be surprised how much of this ‘drool’ is attractive to mosquitoes.”
Dice grabs her trusty golf-club ladle, heads to the edge of the long water trail, and dips into the drool.
“Now!” her voice rises. “There. There’s some mosquito larvae.”
Inside the scoop, among the dirt and tiny bits of glistening debris, three half-inch-long things are wiggling. They look almost like little transparent caterpillars. “See that?” Dice says. “When they move, they travel.”
Indeed, the slightest shaking of the ladle causes the larvae to wiggle. And when they wiggle, they skitter through the water.
“These look like Culex tarsalis,” Dice says. “And they are purveyors of West Nile virus.”
At first, glancing at this little pond of urban drool on Oliver Avenue, it’s difficult to see the larvae among the algae and dirt. But once you do see them, it’s difficult not to. They’re everywhere, wiggling and wriggling by the dozens.
“They have to surface to breathe,” Dice says, pointing out how the larvae will wiggle up, breathe, and settle down, then wiggle up, and settle down again. It’s a creepy little dance. “Kind of gives you the willies, doesn’t it?” she laughs.
Dice scoops her ladle a few more times along the length of the gutter, trying to get a sense of the larvae population, gauging how much Bti to use.
On her third scoopful, she finds something different.
“Those are pupae,” she says, pointing. At the top of the water in the ladle, two tiny balls are floating. “The larvae curl up into little circles like that,” she says. “Their bodies change, and harden. This is the last phase before the adult mosquito emerges.”
The pupae float, breathing at the surface, until disturbed. Then they move much as the larvae do, wiggling and wriggling. Only, after a pupa wiggles, it balls back up and floats to the top.
“The pupae don’t eat,” Dice says, “which is why the bacterial formulations don’t work on them.”
To kill the pupae, Dice would have to use the environmentally destructive Golden Bear Oil. “I don’t want the oil in this gutter,” she says, then adds, “People walk their dogs here.”
She decides to focus on the larvae, which are far more populous in the puddle anyway.
She heads back to the locked rubber chest with skull and crossbones on it, and she takes out a handful of clear, water-soluble packets. Inside each one are a bunch of golden pellets that look a little like couscous. This is the VectoLex Bti.
“It doesn’t take a lot of this to treat an area,” says Dice, as she drops the first packet of VectoLex into the water. Within moments, the packet dissolves, and the pellets spread, some floating and some sinking to the bottom.
Up the puddle 20 feet or so, Dice drops another packet in. Then 20 feet farther, and another packet goes into the water.
“This will hold up for about two weeks,” Dice says, as she drops a fourth packet, “so even if there are eggs in here that haven’t hatched yet, if they pop out in the next week or so, it’ll still work.”
A young woman in flip-flops ambles by Dice and shows barely a passing interest. She has no way of knowing that Dice may well be saving her life.
But Dice dismisses the notion with a wave of her hand.
She says, “I’m just doing my job.”


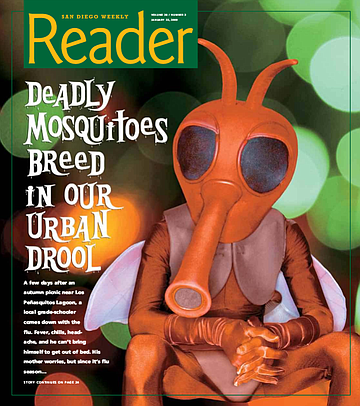
A few days after an autumn picnic near Los Peñasquitos Lagoon, a local grade-schooler comes down with the flu. Fever, chills, headache, and he can’t bring himself to get out of bed. His mother worries, but since it’s flu season…
Three days go by. The boy doesn’t seem to be getting any better. The mother begins to worry more. She wonders whether she should make an appointment at the doctor’s.
The next morning, the little boy is lying in bed with a blank stare. He’s unresponsive, and the mother panics, calling 911. The boy suddenly begins to talk about algebra and dinosaurs and baseball, all in the same garbled sentence. Then he doesn’t recognize his mother.
At the hospital, the doctor knows the symptoms. He’s seeing more cases like this one lately. He runs a blood test. Sure enough.
West Nile virus.
In the past, there were never more than 15 human cases of West Nile virus in a calendar year in San Diego County. So far in 2008, we’re at 23 cases, and climbing. Since the disease is often fatal to birds, dead birds are a sure sign that West Nile is around. Before this year, the highest number of birds that tested positive in a calendar year was 162. This year? Over 500. Four horses in the county are dead from the disease. Of the 40 “sentinel chickens” used for early detection, 13 have converted to West Nile, including all 10 in Los Peñasquitos Lagoon, 2 in Oceanside, and 1 in the Tijuana River Valley. In the past, no more than 1 chicken had converted. Of the 240 batches of mosquitoes that have been tested by the Department of Environmental Health, 37 are positive for West Nile, a higher percentage than ever before. In fact, we’ve never had more than 7 positive batches of mosquitoes in the past.
“West Nile virus is vectored from the bird world to the human world by mosquitoes,” says Chris Conlan, supervising vector ecologist for the Department of Environmental Health. “And this year has been worse by major magnitudes.”
THIS PARK IS CLEAN
A few hundred yards past the entry to Rose Canyon Open Space Park, along a dirt road off Genesee Avenue, Mary Dice spots a swollen area in a creek. “Standing water,” she says, stopping her white Department of Environmental Health truck. “It’s moving at this end and at that end, but there’s stagnation in the middle.”
Dice climbs out of the cab, heads around back, and pulls from her gear what looks like — and, as it turns out, is — a golf club with a ladle soldered onto where the head of the club should be.
“Golf courses have a lot of water features that need to be treated,” Dice says. “So once we get to know the guys, we ask for some of their old clubs. And then we saw off the head and solder a ladle on instead — voila!” She laughs, brandishing the handy tool. “High-tech mosquito-control instrumentation.”
Dice, 57, is a wiry, outdoorsy-looking woman with short, gray hair. A senior technician for the Department of Environmental Health, she’s worked there for over 18 years.
Dice’s department treats public lands — rivers, creeks, ponds, sewage spills — in an attempt to eradicate disease-carrying creatures such as rats and mosquitoes.
“Mosquitoes lay their eggs in standing water,” Dice explains. “It takes about a week, depending on temperature, for the eggs to hatch. The larvae go through four growth stages for the next week or so, before they turn into pupae. Then the adult mosquito emerges from the pupa and goes out looking for a blood meal.”
So the best way to find hundreds of mosquitoes in one place is to seek out their breeding grounds.
“Moving water actually drowns the larvae,” Dice says. “They have a siphon on their back ends, and they have to breach the surface with that siphon and take in oxygen on a regular basis. If the water’s moving a lot, then they’ll have to use more energy than they can take in. That’s not what larvae do. They rest up, and then go after food, and then they rest again. So that’s why mosquitoes lay their eggs in standing water.”
At least 25 species of mosquito live and bite in San Diego County. Only 4 species carry West Nile, but the others need to be watched as well, according to Dice. “At this time,” she says, “we don’t have dengue fever here. But it’s become common in Mexico and Texas, so we’re on the lookout.”
Dice and 14 other vector-control technicians are assigned to different areas in the county for monitoring and treatment. “We’re responsible for all the known sites in our areas,” Dice says, “and we’re responsible for finding additional sites. We try to make sure that the larvae aren’t around long enough to become adults and then fly off and bite people.”
Dice covers “five Thomas Guide pages” in her area, from just east of the Department of Environmental Health office on Hazard Way, near Tierrasanta, all the way to the coast, then north to Del Mar and south to Mission Bay Park. Her jurisdiction encompasses roughly 150 natural mosquito-breeding sites.
But lately, this area has also begun to include hundreds of algae-filled swimming pools that require treatment as well.
“This year’s been just hellacious,” Dice says. “And it’s mostly because of all the foreclosures. I mean, there must have been thousands of green swimming pools that we treated.”
The county health department has even started using its helicopter to spot potential mosquito pools in backyards.
“People are usually pretty surprised when we show up at their front door with a picture of their pool.” Dice chuckles. “But we operate on the principle of helping people. So if you have a green pool, and our helicopter spots it, and I find your house, then I’m not there to give you a lecture or citation or problem. I’m there to help you. If your pool filter’s broken, and you’re looking at thousands of dollars of repairs, and you can’t do it, we’ll be happy to provide you with mosquito-eating fish, and we’ll put them in your pool for you, and we’ll give you a card with a number to call if your fish die off for any reason. Or if you’re getting your pool repaired, then we’ll come fish them out and use them elsewhere.”
A tank full of these little glittery fish is the first thing you see upon entering the front door of the Environmental Health building on Hazard Way. The little surface-breathing Gambusia affinis are found naturally in the county, and Dice has fish traps in the back of her truck to catch them whenever possible. “If I’m at a site that has some, then I’ll set a trap there and head back at the end of the day to take them back to the office. They’re hard workers, and they work cheap,” she jokes. “They don’t have a union.”
Dice dips her golf-club ladle into the edge of the swollen area of Rose Canyon Creek, lets some water eddy in, and then lifts the ladle toward her face, looking for larvae. She dumps the water and checks twice more at different spots along the edge. “I’m not finding any larvae here,” she says. “And that’s a good thing. That’s encouraging.”
Dice and the other technicians in her department have been pushing themselves to hit as many potential breeding sites as possible, as often as possible. They drive around all day in their white Ford Ranger trucks.
But helicopter drops are also used to get to places that are unreachable from the ground, such as large standing ponds socked in by thick vegetation. Every three weeks during the height of the mosquito-breeding season, from June through September, the Department of Health’s single helicopter will head into the air.
“We use it where we need it,” Dice says of the helicopter, noting that each time it goes up, it costs the county taxpayers about $5000. “But, by golly, if you can squeeze in there and get the job done, then you should squeeze in there and get the job done.”
But many of the mosquitoes in the area come from places much closer to home, even “small sources in our own backyards,” Dice says. “A watering can that you’ve forgotten about, or plant saucers. Without some knowledge about it, you’d have no idea to look there for mosquitoes. A lot of people have no idea that mosquitoes have an aquatic larval stage before they progress to adults.”
Joggers and dog-walkers pass by periodically in the Rose Canyon morning light. After a few more stops along the path, checking with her golf club ladle, Dice determines that the park is clean. “I used to have to hike entire canyons through thick brush,” Dice says. “But now I can mentally trim areas down to their standing water and just pull up at specific spots.”
She climbs back into her truck and drives out to Genesee Avenue, heading toward Pacific Beach. “I have some street gutters holding water in Pacific Beach, near the military housing behind Mission Bay High School. “It’s an area I watch pretty closely, because we’ve had a higher rate of bird mortalities there lately.”
Dice has a host of weapons in her arsenal when mosquitoes are discovered.
In the back of her truck, along with the golf-club ladle and wire-mesh traps for catching mosquito-eating fish, Dice has an old-style B&G tank of Golden Bear Oil, a powerful pesticide that she hates to use. “It’s the only thing that will kill pupae,” she says. “It’s a suffocant. It lays on the surface of the water. It’s a short-lived product, but while it’s there, it kills all the other aquatic insects at a site. It’s very sad because I particularly like dragonflies and damselflies.”
But Dice hardly ever resorts to using the Golden Bear Oil. She has much safer products locked inside a large, black, rubber trunk in the back of her truck. It just so happens that this trunk is covered with multiple images of skulls and crossbones.
“It’s just the law that we mark it that way. But there’s no poison in there. It’s just full of Bti and growth inhibitor.” Bti stands for Bacillus thuringiensis israelensis. It refers to any bacterial product that controls pests.
Dice explains, “Originally, it was a mosquito product that was discovered in Israel in the early ’80s. One year, they went out to control the mosquito larvae, and there were none. And they noticed that the leaves on the corn plants had developed some type of problem, and they were dropping off into the water. And corn plants don’t normally drop their leaves. So they looked closer, and they found a particular bacteria that affects only the gut of mosquito larvae. So now when I put VectoLex or another Bti product out into the water, I feel good about it, because I know it’s only going to affect the mosquito larvae. If a coyote wants to come by five minutes later and have a drink of water, it’s not going to affect him.”
VectoLex is ground-up corncob impregnated with bacteria specific to the gut of mosquito larvae.
Dice remembers testing the first Bti’s 25 years ago, and after she sprinkled some in a pond, a flock of ducks flew down and ate it up just as fast as she could spread it out. “At first I thought, ‘Oh, no!?f I was used to pesticides, and here these ducks were eating this stuff.”
The ducks were pets, and they were subsequently observed for adverse effects. “They were fine,” says Dice. “And after that, I felt relieved to have this product. Not to mention, but 24 hours later we came back, and there wasn’t a single mosquito larva living.”
Thanks to the successful development of Bti’s, the county hasn’t sprayed pesticides in over 16 years, according to Dice.
Another weapon in Dice’s arsenal is a growth-inhibiting hormone called Methoprene. This slow-acting insecticide prevents eggs and larvae from developing into adults, so that the mosquitoes die in arrested stages of immaturity. Methoprene has no effect on adult mosquitoes, however.
“Methoprene works long-term,” says Dice. “And if you’re regulating sensitive areas, or areas that are difficult to get to, you want to use a long-term product.”
GETTING TO KNOW YOUR “BUGS”
PART ONE
Mosquitoes are attracted to carbon dioxide. They also seem to be more attracted to some people than others, but no one knows whether this is because of personal chemistry or diet or cologne or blood health. Without a doubt, mosquitoes possess a higher level of natural awareness than humans can understand.
“A mosquito will land in a dry spot,” says Dice, “and she’ll know that water will return. And she’ll put her eggs there in a dry area, knowing that it will fill with water soon.”
Some mosquitoes are day-biters, but most feed from dusk until dawn. The first thing on a female mosquito’s mind is blood. She needs a blood meal to procreate.
Male mosquitoes lack the saberlike proboscis of the female and are harmless to humans and animals. The males eat only nectar.
“Female mosquitoes fill their stomachs with blood,” Department of Health supervising vector ecologist Chris Conlan explains. “When a mosquito finishes her meal, she’s loaded. It’s a big, red abdomen full of blood. And at that point, she’s going to go off and find a nice, quiet corner to rest. And she’ll spend two or three days converting the protein in that blood meal into eggs. At some point during that time, of course, she’s mated with a male, and that happens pretty quick, and she can store sperm from the male. So she really only has to mate once. And once she’s done all that, then she goes on a hunt to look for a nice place to lay her eggs. The whole process might take about four days, give or take, and then it starts all over again. Theoretically, under the best of all possible circumstances, a mosquito can lay a hundred or so new eggs every four days.”
And each mosquito will continue to eat and ripen eggs and lay them for five or six blood meals or more, depending on temperature, food availability, and, of course, whether or not it can avoid being slapped in mid-meal.
Most mosquitoes only live for a couple of weeks, but Conlan says that some will buck the odds and hibernate through a winter. “The mosquitoes that live longer are a greater risk for disease transmission,” says Conlan, “because they may have picked up an infection somewhere along the line that’s finally incubated long enough that they can transmit it to whatever else they bite.”
GETTING TO KNOW YOUR “BUGS”
PART TWO
Ever since he was in medical school at UCSD 20 years ago, Dr. Dale Lieu has been fascinated by “bugs and the drugs that kill them.” Although, when Dr. Lieu says “bugs,” he doesn’t mean mosquitoes, per se. He means viruses, bacteria, and parasites.
Dr. Lieu is a specialist in infectious diseases for Kaiser Permanente Medical Group.
“Like a lot of diseases that mosquitoes carry, West Nile doesn’t hurt the mosquito,” Dr. Lieu says. “And traditionally, it hurts animals a lot more than it hurts people. In a way, you could say that people aren’t the real target; we just kind of get in the way.”
The first time West Nile virus was discovered in the United States was in 1999 near the Bronx Zoo.
“They started having birds die off,” Mary Dice says. “Not their collection, but other birds, crows. And they were kind of confused, and they have an expensive collection of exotic birds to protect, so they got very interested. Because they’d never seen West Nile virus in this country before, the New York health department assumed that some exotic animal from the zoo had imported some disease. That turned out not to be the case. And the zoo collection was never affected. But they helped track it down. They discovered that it was, in fact, West Nile virus.”
Because birds are the carriers of the disease, and they migrate so widely, once a bird becomes a reservoir, then West Nile can go from New York City to Mexico in a week or less.
“West Nile has been sweeping through the country,” Dr. Lieu says, “but the interesting thing is this: Wherever it has peaked, and then the number of cases has started to go down, the virus has never circled back. If you look at New England and New York, where they had a whole bunch of cases seven or eight years ago, in the past couple of years, they hardly had any. And we think both people and the animal community eventually develop immunity.”
But Dr. Lieu is quick to state that we don’t have enough experience with re-exposure to the disease to guarantee that we develop complete immunity. “There’s probably a good chance that people who get it once become less likely to get real sick,” he says. “But we don’t know how protective it is.”
Has San Diego reached its peak?
“There’s no way of telling that,” Dr. Lieu says. “We’re certainly on an upswing, as far as the number of cases. We’ve had 23 cases so far this year, and we had 15 in 2007. But who knows where that’ll stop, or when it will start going down?”
Lieu wears a white lab coat with his stethoscope in his pocket. He expressly does not wear a tie, because it’s “the one article of men’s clothing that we never wash,” and Lieu is nothing if not fastidious. “I think most infectious disease doctors are like that,” he laughs.
Dr. Lieu himself has treated “a few cases” of West Nile virus in the past year. “The most susceptible people are very young, very old, or have compromised immune systems. Only about one in five people who are exposed to the disease actually get sick. And for the majority, they only get a flulike illness: fever, chills, muscle aches, headaches, fatigue. And that starts about three to seven days after the bite. Most people just think they have the flu, and they get better after a week or ten days, and they don’t think much of it. The vast majority are never even checked for West Nile. But about 1 in 100 people who get infected develops encephalitis. And that’s the most dangerous manifestation of West Nile. That’s where the brain tissue itself becomes infected with the virus, and it gets inflamed. And people come in real, real sick.”
What can a doctor do for such a person?
“There’s no specific treatment other than supportive care,” says Dr. Lieu. “If the encephalitis is from herpes or chicken pox, then we’ll use antiviral medication. But if it’s from West Nile, and we know it’s West Nile, then there’s no specific treatment. All we can do is support the person through this period where they’re really sick, protect them from complications, feed them, and hope the inflammation goes away.”
What are the symptoms of having swollen brain tissue?
“Encephalitis can be really scary,” Dr. Lieu says. “People who have it become basically delirious. They’re bonkers. They’re nonsensical in what they’re saying. They’re completely disoriented. It’s clear that they’re mentally impaired. They can’t hold a cogent conversation. Their mind wanders all over the place. They’ll drift between periods of looking like they’re ready to fall asleep and periods of restlessness. They may not recognize family members. There could be a blank stare.”
The encephalitis portion of West Nile will often last for over a week, Dr. Lieu says, and not everyone makes a complete recovery. “You’re talking about brain tissue. And some of that tissue may suffer some permanent damage. When people have serious cases, a lot of them don’t come back completely. They’re thinking they always have some impairment. They may or may not have some neurological deficits, where some parts of their brains don’t work the same way anymore.”
STUDYING THE VECTORS FROM “BUGS” TO “BUGS”
“Mosquitoes are one of the biggest threats that are out there,” vector ecologist Chris Conlan states. “There’s always been some mosquito-borne illness throughout the United States. We used to have some real nasty ones here, like malaria and yellow fever. But because of modernization, and nice living conditions with screens on the windows, and mosquito control, we’ve beaten those diseases back and pretty much pushed them out. The only ones that stayed here tended to stay here at fairly light levels — like equine encephalitis. And they show up every year, but maybe a half a dozen or a dozen people are affected in a bad year.”
Conlan’s tone changes to a slightly higher pitch. “But when West Nile showed up in the United States in 1999, that kind of changed everything. Because now, all of a sudden, we have a new disease in a new land that’s ready to run amok. It’s like having a three-year-old in a candy store. It’s still establishing itself in the environment, and, as a result, we still don’t understand yet just how bad it could end up being. So all of the vector agencies are always kind of in this ‘prepare for the worst and hope for the best’ mode.”
Conlan, a short, squarish man with wavy, graying hair and piercing blue eyes, is a self-professed “bug geek” who started off on his career path by catching butterflies when he was a little kid.
Part of the problem, he says, is that the encephalitis viruses like West Nile are carried around in the bird population. “And we can’t kill all the birds, and not to mention, but birds travel everywhere. So, the best thing we can try to do is to try to control it from the mosquito side. But you can’t get all the mosquitoes either.”
Conlan’s lab in the Environmental Health building on Hazard Way is full of the usual microscopes and test tubes and petri dishes, but it also contains some weird-looking objects.
Conlan heads over to a series of petri dishes laid out on a table. Each labeled dish contains tens, or even hundreds, of tiny mosquito carcasses. “To the naked eye, they all look the same,” Conlan says. “You need a magnifying glass, at least, to tell them apart. But the two that we really worry about here are Culex quinquefasciatus — we call them ‘quinks’ for short — and Culex tarsalis. The quinks are urban breeders, which makes them particularly dangerous. They’re our urban nemesis for West Nile transmission. And the tarsalis is actually called the ‘Western encephalitis mosquito.’ It’s not quite as big of a threat in urban environments, usually, but what we’re finding is, even in urban zones, if someone lets a swimming pool go out of whack, and it turns green, it can breed tarsalis in massive numbers. And the problem with tarsalis is that it will fly a lot farther than the quinks. They might cover a range of two to three miles in some cases.”
As Conlan speaks, one of his colleagues comes into the lab bearing an armful of plastic bags. Inside each bag is a spread-winged dead bird — two crows, a jay, and, in one large bag, a once-majestic red-tailed hawk. On each bag is written where and when the bird carcass was found.
“These are from our bird pickup program,” Conlan says. “What we do to monitor the disease is, while most birds will get the disease and get a little ill, they’ll get over it and go on to live their happy birdie lives, but some species do not. They end up in a plastic bag, and off they go to the vet for testing. So we focus our testing on birds that are likely to die from it — crows, jays, and birds of prey, like hawks and owls. And you have to get them fresh, right after they die, otherwise you can’t test them because the virus degrades too fast.”
If the Environmental Health veterinarian determines that a bird died from West Nile, then Conlan’s team puts a dot on a map and monitors that area to see if a hot spot is developing. “The birds are the best early detection method that we have. We have other methods that we use. We test the mosquitoes themselves, and we also have what we call ‘sentinel chickens,’ which are basically four groups of ten chickens each, strategically located around the county — one in Oceanside, one in the Tijuana River Valley, one in eastern Santee, and one in Peñasquitos Lagoon — and we do a blood test on those chickens every two weeks to see if they’ve developed antibodies to the virus. Because chickens don’t die when they get it. They mount a quick response and get over it in a heartbeat.”
But how does a mosquito bite a bird? How does it get that little proboscis through all those thick feathers?
“It doesn’t,” Conlan says, about to deliver a truly macabre piece of information. “The best place to get a bird is right in the eye. A bird cannot protect its eyes. So, even when their eyes are closed, the mosquito can bite right through the bird’s eyelid.”
One of the tests Conlan’s lab is using involves the bird’s eye fluid because there’s a higher concentration of the virus in the eye than there is anywhere else in the bird.
At another table in the lab, Conlan points to some unusual-looking devices. Mosquito traps.
The traps are made of inexpensive household products available at any hardware store, such as bus tubs, handheld fans, battery packs, and mesh nets. Nothing high-tech about them, but they are effective. The traps are hung from tree branches overnight, and mosquitoes are collected from the catch bags in the morning.
One kind of trap uses dry ice and a high carbon dioxide concentration that draws mosquitoes toward a fan that blows them into a bag. “That one’s for hungry mosquitoes,” Conlan says. “They associate carbon dioxide with the breathing of some creature that’s full of blood.” A second kind of trap — called a gravid trap — attracts pregnant females by using a mixture of foul-smelling water and organic debris that also eventually blows the attracted insects into a bag for later study.
“The mosquitoes are used for testing,” Conlan says, “and we’ll also count the mosquitoes and sort them by species, which helps us understand if there might be a problem going on in one area or another.”
Some nights, in some areas, the traps will come back nearly empty, and sometimes, a single trap will contain “several thousand” mosquitoes.
“We had a case up in Oceanside this summer,” Conlan relates, “where one of our traps was filling up with the bad kind of mosquitoes — Felix tarsalis — but the normal sources that we were monitoring weren’t showing anything. So we ended up finally going door to door, and we finally found a house that had a bad pool behind it, and it was just breeding them like crazy and messing it up for the whole neighborhood.”
To combat this increasingly common scenario, Conlan says, “We’ve got to teach people. Don’t breed mosquitoes, or you’re kind of asking for it.”
THIS NEIGHBORHOOD IS…NOT CLEAN!
“This looks likely as heck!” Mary Dice exclaims. And then says, “Oh, my gosh.”
She’s turned left off Garnet Avenue in Pacific Beach and parked her truck alongside a veritable stream of gutter water. She calls this stuff “urban drool,” and it’s running down Olney Avenue and turning onto Oliver Avenue. Every ten feet or so along this tract of dark water, large brown puddles bulge out from the curb.
“It fills up the low spots on a lot of our streets,” Dice says, “and you’d be surprised how much of this ‘drool’ is attractive to mosquitoes.”
Dice grabs her trusty golf-club ladle, heads to the edge of the long water trail, and dips into the drool.
“Now!” her voice rises. “There. There’s some mosquito larvae.”
Inside the scoop, among the dirt and tiny bits of glistening debris, three half-inch-long things are wiggling. They look almost like little transparent caterpillars. “See that?” Dice says. “When they move, they travel.”
Indeed, the slightest shaking of the ladle causes the larvae to wiggle. And when they wiggle, they skitter through the water.
“These look like Culex tarsalis,” Dice says. “And they are purveyors of West Nile virus.”
At first, glancing at this little pond of urban drool on Oliver Avenue, it’s difficult to see the larvae among the algae and dirt. But once you do see them, it’s difficult not to. They’re everywhere, wiggling and wriggling by the dozens.
“They have to surface to breathe,” Dice says, pointing out how the larvae will wiggle up, breathe, and settle down, then wiggle up, and settle down again. It’s a creepy little dance. “Kind of gives you the willies, doesn’t it?” she laughs.
Dice scoops her ladle a few more times along the length of the gutter, trying to get a sense of the larvae population, gauging how much Bti to use.
On her third scoopful, she finds something different.
“Those are pupae,” she says, pointing. At the top of the water in the ladle, two tiny balls are floating. “The larvae curl up into little circles like that,” she says. “Their bodies change, and harden. This is the last phase before the adult mosquito emerges.”
The pupae float, breathing at the surface, until disturbed. Then they move much as the larvae do, wiggling and wriggling. Only, after a pupa wiggles, it balls back up and floats to the top.
“The pupae don’t eat,” Dice says, “which is why the bacterial formulations don’t work on them.”
To kill the pupae, Dice would have to use the environmentally destructive Golden Bear Oil. “I don’t want the oil in this gutter,” she says, then adds, “People walk their dogs here.”
She decides to focus on the larvae, which are far more populous in the puddle anyway.
She heads back to the locked rubber chest with skull and crossbones on it, and she takes out a handful of clear, water-soluble packets. Inside each one are a bunch of golden pellets that look a little like couscous. This is the VectoLex Bti.
“It doesn’t take a lot of this to treat an area,” says Dice, as she drops the first packet of VectoLex into the water. Within moments, the packet dissolves, and the pellets spread, some floating and some sinking to the bottom.
Up the puddle 20 feet or so, Dice drops another packet in. Then 20 feet farther, and another packet goes into the water.
“This will hold up for about two weeks,” Dice says, as she drops a fourth packet, “so even if there are eggs in here that haven’t hatched yet, if they pop out in the next week or so, it’ll still work.”
A young woman in flip-flops ambles by Dice and shows barely a passing interest. She has no way of knowing that Dice may well be saving her life.
But Dice dismisses the notion with a wave of her hand.
She says, “I’m just doing my job.”
Comments