 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

Most stories begin with a person or an event. This one begins with a book.
Last summer I read The Brain That Changes Itself by research psychiatrist and psychologist Norman Doidge, M.D., which discusses developments in neuroscience, especially in the area of neuroplasticity. Now, if I were in a bar and the guy on the next stool leaned over and said to me what I’ve just written here, I’d give a wave to the bouncer. But hang on.
When I was in school, I was given two pieces of information about the brain that, well, stuck in my brain. The first was that the brain was hardwired, meaning that each bit of the brain had a specific function and if that bit were damaged then that particular function was lost forever. The second piece of information was that even though the brain consisted of billions of nerve cells called neurons, I was constantly losing them and I would never get them back.
As a kid, it seemed I was so rich in neurons that the loss caused by a few six-packs during the week or a rough pickup football game without a helmet meant nothing. After all, I was a billionaire.
But as I moved into old age, it seemed I could feel windy places between my ears where megalopolises of neurons used to be situated, dank caverns inhabited by gloomy question marks bent over smoking piles of dead synapses. Some days it seemed as if I only had about 475 neurons left. Some people hear a ringing in their ears? I heard creaking.
Then I read Doidge’s book and learned that all that was a lot of baloney. If one part of the brain is damaged, its function can often be picked up by another part through the creation of new neural pathways. This has resulted in vast improvements and even cures in a number of conditions, from stroke to irrational compulsions, worries, and obsessions. It has also led to new ways of fixing learning problems and sharpening perception and memory. And this is only the beginning of the list.
Those lost neurons? If you don’t watch too much TV and continue to read books, a sizeable number can be replaced.
When I finished the book, I read a few others on the topic and it turned out that one of the top neuroplasticity guys was at University of California, San Diego: Dr. V.S. Ramachandran, who is director of the Center for Brain and Cognition and professor of psychology and neuroscience. His most recent book, The Man with the Phantom Twin, came out in January, and he has published a handful of other books and well over 150 articles and has enough medals, awards, and certificates of merit to fill a large living room. Newsweek has named him one of the hundred most important people to watch in the 21st Century.
One of Ramachandran’s books, Phantoms in the Brain (1998), has a section about phantom-limb syndrome, a condition found in nearly all amputees that makes them experience feeling in the missing limb, as well as feeling that they can move the limbs, as in waving goodbye or kicking a ball. Many people whose bladders have been removed (or genitals or rectums or uteruses or ulcers) can also feel phantom sensations — but that is another story.
Many of those who lost a limb have also experienced intense pain in the phantom limb, pain that might keep them awake night after night and continue for years. Well, Ramachandran invented a device that cured or substantially helped a majority of the amputees he worked with who suffered from this pain. And what struck me most was that the device only cost a few bucks.
Before I describe this gadget, let me describe my friend Glenn, who cracked up his motorcycle in 1991 when he was in his 20s. Swerving to the left to avoid an oncoming car, he hit the curb, and the motorcycle toppled over and mushed his left leg. When he woke up in the hospital, his leg, below the knee, was gone. About 4500 men and women are killed on motorcycles each year, and about 85,000 are injured. A fair number of those are part of the approximately two million amputees in the U.S.
What Glenn soon discovered was that the leg didn’t feel gone. He could move his phantom toes, waggle his phantom ankle. At times it tingled as if it had gone to sleep. Most disturbing, at times it felt as if a knife were being driven into it. The pain would often occur when he got home from work and was trying to relax. Or it would occur at night: a phantom knife blade through the phantom foot to make him jump out of bed.
The tingling sensations and waggling of the phantom toes can occur every day. The pain has become less frequent over time; it happens now perhaps once a month. Still, it has never gone away. Glenn is a tall, handsome guy, over six feet, with jet-black hair and a neatly trimmed beard. Mostly, you wouldn’t notice that he has a fake leg, but if he’s tired he’ll limp a little. “They’re heavy,” he told me, “even the expensive ones. They’re always dragging at you.”
The number of amputees who suffer from phantom pain ranges from 50 to 95 percent, depending on which specialist is asked, but the most agreed upon number is around 75 percent. Usually it develops soon after amputation, but it can also begin after a few months or even years. For some people it might get better after a year or two, for others it never stops. Often the pain comes in bursts several times a day, but some experience it less than once a month. A much smaller percentage have it constantly. With missing limbs, the pain often occurs at the end of the limb, or it feels as if the limb is shorter or twisted into a painful position, or as if something is being jabbed into it, or as if it’s on fire. Stress and anxiety can affect the pain, even changes in the weather.
Aspirin gives no relief, but anticonvulsant drugs and heavy painkillers like morphine have helped some amputees. Others have been helped by a transcutaneous electrical nerve stimulator, or TENS, a battery-driven device about the size of an iPod that delivers electrical impulses to stimulate nerves in the painful area. Somewhat more effective has been a spinal cord stimulator, an electric impulse-generating device implanted near the spinal cord. Hypnosis, acupuncture, biofeedback, vibration therapy, massage, yoga, ice packs, heating pads, and even steroid shots have also been useful. But what seems most significant is that nothing helps very much. The pain is often most severe when the prosthesis is removed, and so patients are encouraged to use the prosthesis as much as possible.
According to Doidge’s book, Ramachandran’s research led him to think that the absence of feedback from the missing limb to the brain leads not only to the phantoms but to phantom pain. “The brain’s motor center might send commands for the hand muscles to contract but, getting no feedback that the hand has moved, it escalates its command” until, for instance, it feels as if the fingernails are digging into the palm. This oversimplifies Ramachandran’s findings, but he felt that the phantoms were a result of the brain’s mistaken body image. If the image were reinforced, he reasoned, the pain might vanish.
Advances in prosthetic technology have been hugely affected by the Iraq War, and by 2004 new prosthetics were coming onto the market that seemed more products of science fiction than medical technology. The Otto Bock C-leg has a battery-powered “onboard” microprocessor that controls knee movement and communicates with a computer through Bluetooth technology. It can switch between two modes of activity with several taps of the toe.
The C-leg, however, is receiving serious competition from the Ossur Bionic Power Knee, which can synchronize movement with the sound leg to “lift the user to standing from a seated position; support the user while ascending inclines; and power them upstairs.” When the user is walking, the knee’s pendulum motion swings it forward, senses the changing terrain, and “actively lifts the heel off the ground,” according to Ossur’s website. By means of “artificial proprioception,” which is a person’s awareness of his or her posture, movement, balance, and location, the knee “anticipates and responds to the appropriate function required for the next prosthetic step.” There are also power heels to give the walker a boost so the prosthesis won’t, in Glenn’s words, “always [be] dragging at you.”
Yet these bionic prosthetics are nothing compared to what is currently in development. In February, the Defense Advanced Research Projects Agency (DARPA) awarded a contract to the Applied Physics Laboratory at Johns Hopkins University to finish work on a mechanical arm “that will look, feel and perform like a normal limb,” according to the online magazine Gizmag. The Johns Hopkins laboratory, leading a team drawn from about 30 organizations, had already developed two prototypes of prosthetic arms. The first is an arm that “can be controlled naturally, provide sensory feedback and allow for eight degrees of freedom.” The best prosthetic arms now on the market provide for only three degrees of movement. The second prototype uses 25 individual joints “that approach the natural speed and range of motions of the human limb…[and] are complemented by a range of emerging neural integration strategies,” meaning they can be wired to the brain through the nervous system. You think your hand into motion and it moves. The arm should be ready for regulatory clearance in under two years.
So far the Iraq War has led to amputations for more than 750 servicemen and women. The high number is due in part to the body armor that protects the trunk. Without it, many of these soldiers would have died. In fact, about 92 percent of those wounded in Iraq survive their wounds, as opposed to 76 percent in Vietnam.
Founded in 1958 in response to the Sputnik surprise, DARPA is responsible for developing new military technology, while its prosthetic program tries to provide the best “medical and rehabilitative technologies for military personnel injured in the line of duty,” according to Gizmag. The requirement that the soldier be injured in the line of duty may explain what was for me an odd discrepancy. Between 2001 and 2007, the Veterans Administration performed more than 17,000 amputations on former military personnel, most of whom suffered from diabetes. Although these amputees provide a steady business for the prosthetics industry, their needs have not led to anything like DARPA’s “Revolutionizing Prosthetics” program, which has provided funds for “the most advanced medical and rehabilitative technologies.” Nor would these VA amputees necessarily benefit from the new developments. Coverage of prosthetic limbs has been limited to $2500 or $5000 a year by many private health plans. Or the plans will pay for only one device per limb over the patient’s lifetime. And the insurance lobby has been trying to reduce this amount. The cost of basic prostheses ranges between $3000 and $15,000, while models resulting from the new technologies can be priced at more than $40,000.
As with any war, sympathy and attention goes to the soldiers injured in combat, and of these Iraq has provided nearly 100,000. The first Iraq War amputees were treated at Walter Reed Army Medical Center outside of Washington. Then, as their number increased, the Department of Defense opened a second amputee care center at Brooke Army Medical Center at Fort Houston in San Antonio, Texas, in early 2005.
A third amputee care center was officially opened in San Diego on October 15 as part of the Comprehensive Combat Casualty Care Center, or C5, of the Naval Medical Center. The 30,000-square-foot facility is not only a showpiece of new technology, with an accurate motion-capture system and an advanced bionic technology room used for gait adjustment, but also includes a 3500-square-foot obstacle course with a 30-foot climbing wall. It cost $4.4 million to build and another $4 million to outfit and staff. A major focus of C5 is to get the amputees moving as soon as possible, taking them on ski trips, having them engage in sports, and even learning to surf. I decided to visit the facility, but before I spoke to the wounded soldiers, I wanted to talk to Dr. Ramachandran at UCSD.
Born in India in the southern province of Tamil Nadu, Ramachandran received his medical degree from Stanley Medical College in Madras, specializing in neurology, and his Ph.D. in psychology from Trinity College at the University of Cambridge. He also studied at Oxford. The British scientist and writer Richard Dawkins has called him “the Marco Polo of neuroscience” because of his explorations into uncharted territories.
Ramachandran’s early work was on human visual perception, using optical illusions to study the brain mechanisms that underlie visual processing. And it was illusions that became key in working with phantom limbs in the mid-’90s. Later, his work with phantom limbs led to using techniques of visual feedback to help stroke victims recover the use of arm and leg functions.
Since then, he has kept his focus on various neurological syndromes to study their underlying mental functions. He and his colleagues have written articles on synesthesia, in which letters might be linked with colors, or sounds with smells. Then came papers on Capgras delusion, in which a person believes that his family members or friends have been replaced by imposters. He has also written about autism, apotemnophilia (in which a patient has a strong desire to amputate one of his or her limbs), and mirror agnosia, where four right-hemisphere stroke patients “were indifferent to objects in their left visual field even though they were not blind,” according to Ramachandran.
In “The Emerging Mind,” the first of five Reith Lectures for the BBC in 2003, Ramachandran described the vast scope of the brain as well as the source of its fascination for him. “The brain is made up of one hundred billion nerve cells, or ‘neurons,’ which are the basic structural and function units of the nervous system. Each neuron makes something like a thousand to ten thousand contacts with other neurons, and these points of contact are called synapses, where exchange of information occurs. And based on this information, someone has calculated that the number of possible permutations and combinations of brain activity, in other words the number of brain states, exceeds the number of elementary particles in the known universe.… It never ceases to amaze me that all the richness of our mental life — all our feelings, our emotions, our thoughts, our ambitions, our love life, our religious sentiments, and even what each of us regards as his own intimate private self — is simply the activity of these little specks of jelly in your head, in your brain. There is nothing else.”
Ramachandran described his work to me as we sat in his office, which was as comfortable as a private study or den and decorated with artwork from Asia and Europe, a bust of Freud, a picture of Darwin, odd little antique machines, fossils, bric-a-brac.
He is a tall, dapper man in his late 50s with a mustache and receding curly black hair. He was wearing black shoes, black pants, a black shirt, and a brown-flecked jacket. Handsome and rather aristocratic, he has the slightly ironic and impatient manner of someone who is already thinking about what he needs to do next and what he must do after that. He speaks with nearly no accent other than rolling his R’s and uses quick rushes of phrases between studied transitions to create a striking fast-and-slow pattern that makes his mental gears appear almost visible.
The term “phantom limb” was first used by an English doctor in 1872 in a paper describing how amputees could experience sensations in their missing or phantom limbs. Ramachandran explained that 98 percent of amputees experience phantom sensation and that an innate component of our sense of body image seems to be “hardwired” into our brains, so that even congenitally limbless patients can still feel sensation in the missing limbs. Pain, he argues, first occurs in the brain, and then the sensation or impulse is sent to the damaged or affected area. When I jam my finger in a car door, it’s not the finger that hurts first; rather, the brain evaluates the damage and sends the sensation to the finger. That’s when I cry, “Ouch!” In the case of phantom limbs, the sensation will be mostly a tingling in the missing limb, but three quarters or more can experience excruciating pain. Ramachandran has a great fondness for what he calls “five-minute experiments” that changed the world, such as Galileo’s use of a cardboard tube and two lenses to show that the earth is not the center of the universe, or his experiment of dropping a ten-pound and a one-pound cannonball from the Leaning Tower of Pisa to show that falling bodies fall at the same speed. And there is Michael Faraday’s experiment with a bar magnet, iron filings, and a sheet of paper to demonstrate the presence of a magnetic field, as well as Newton’s work with a simple prism to show that white light is a composite of different colors.
These “five-minute experiments” influenced Ramachandran in trying to solve the problem of phantom pain with a simple, noninvasive treatment using about $20 worth of material. He constructed a “virtual reality box” by setting a long mirror horizontally inside a cardboard box from which the top and front surfaces had been removed. The patient places his good arm (or leg) and the remaining stump in the box separated by the mirror, so that the reflection of the good hand creates the illusion of two hands. The patient then simultaneously tries to move both his hand and the phantom and has the illusion of seeing his phantom hand move, while the actual phantom also feels as if it’s moving. The reflection gives him positive visual feedback that tells the brain that his phantom hand is moving just as it should. In the case of a man whose phantom fist feels clenched, the mirror box creates the illusion that the clenched fist can open. By working with the box, the man learns to unclench his phantom hand. What was discovered in these cases was that the data coming from the different sense modules in the brain can change as the brain updates its model of reality in response to new information. Of course, it was all more complicated than my paraphrase suggests, but my main interest was the effect of these experiments on the patients.
“Two-thirds got great relief in three to six weeks, sometimes sooner,” Ramachandran told me. “In many cases the phantom goes away completely, but if the pain happens to come back, then the box can be used again.”
To give me a better sense of how it worked, he took me downstairs to a room where a tall mirror about two feet wide rose vertically from the floor.
“Stretch out your right hand horizontally across the right side of the mirror,” he told me, “and move a little to the right so you can see your right hand and its reflection, but not your left hand.”
It took some fiddling, but in a few moments I was staring down at my right arm and its reflection, while my left hand was hidden behind the mirror.
“Now wiggle the fingers of your right hand and look at the reflection, while keeping your left hand still.”
As I wiggled my fingers and looked at the reflection, I felt a tingling in my hidden left hand and the sensation that the fingers of my left hand were wiggling as well. The visual feedback from the mirror had tricked my brain into believing that my left hand was moving, and the brain had responded by sending out the appropriate sensations.
But Ramachandran’s interest is in research rather than in the clinical application of his findings, and he knew little about whether his mirror treatment was being used in clinics. Once he is done with a particular facet of research, he hurries on to something else. He had had no contact with medical staff at the Naval hospital, although he said, rather vaguely, “I gather that talks have begun.”
A Google search, however, informed me that the therapeutic use of mirror therapy is increasing. At Walter Reed Hospital the therapy is given to military amputees. This was initiated in 2007 by a Navy neurologist, who was trying to help soldiers suffering from phantom pain. He recalled reading in graduate school a paper by Ramachandran about helping patients with phantom pain with a $20 mirror. But I’ll return to that later.
What struck me most was that more than a dozen years had gone by between Ramachandran’s initial discoveries and their application. That meant that well over a million American amputees had been suffering needlessly from phantom pain.
“The medical community is very conservative and resistant,” Ramachandran told me. “They don’t really care about rehabilitation that much. They leave it up to the therapists. I’m talking about inertia rather than skepticism. They accept it intellectually, but then back in the hospital they get busy with other work and seem to forget about it.”
One possible reason why doctors and clinics have been slow in using the mirror treatment for amputees is its very simplicity. Instead, they find greater credibility in more complicated and costly systems. For instance, scientists at the University of Manchester, U.K., have developed a virtual-reality system that gives amputees the illusion that the missing limb is still there and can function. The scientists referred to Ramachandran’s work with the mirror box, saying they would use it with their virtual-reality technologies to create a more effective treatment for phantom pain.
Ramachandran scoffed at this. “Virtual-reality labs are a waste of money, and they don’t work as well as the simple mirror box, except when working with double amputees. But for many people, the more expensive something is, the more credible it is.”
The next morning I sought out a representative of San Diego’s Amputees in Motion, an amputee support group that Ramachandran had mentioned. The head of the group is Bert Acosta, who lives out near Grossmont College in a two-story Spanish-style house with three huge trees in the front yard.
Acosta is a retired engineer in his 70s who lost a leg in a motorcycle accident 38 years ago. The local Amputees in Motion was started in 1973, and Acosta joined soon afterward. Although the group has a membership list of 500, only about 15 are active. These members visit hospitals to talk to recent amputees about what they might expect and how they might deal with it. The great majority of the amputees are diabetic, with about 1 in 50 being the result of a motorcycle accident. Acosta is a friendly man and a good talker. We sat in his living room.
“After they took off my leg,” he said, “it got infected in the hospital and I got gangrene and the doctor thought I’d die by the end of the day. He said I had one chance out of ten thousand of surviving because I was so weak. I woke up the next day, and they’d amputated my left leg four inches above the knee. But I still felt my toes; it felt like I had a tourniquet on them. Then the pain got worse. My surgeon handed me a bottle with about a dozen pills. ‘Take them when you want,’ he said, ‘but don’t call me again.’ You see, he was afraid I’d become addicted. I’ve met several hundred amputees and not known anyone who didn’t have phantom pain. I saw a man yesterday who had just had his leg amputated, and he complained of charley horses. Some feel like molten lead is being poured on their leg; another will say it feels like a cold ice pick being shoved deep into the bone marrow; a third person will say it feels like the leg is being pulled and the nerves stretched. I can have the molten lead feeling or the stretched feeling. The pain is irregular. It will happen for 10 minutes, stop for 20, come back for 5, then stop and come back again. I don’t have the pain when I’m walking or working, but when I’m home sitting down, then my leg starts tingling. Others, it hurts when they walk and stops hurting when they take off the prosthesis. Fifty people with the same amputation could have 50 different responses. Many don’t do anything about it. For me, after all this time, it’s more of an inconvenience. It feels as if my shoe is too tight. Even if I’m not wearing my prosthesis, it can feel like the shoe is too tight.”
Acosta showed me his small TENS unit, which sends out a series of different electronic waves of different strengths, so each person’s unit has to be individually set.
“The TENS shocks you on degrees of 1 to 100, and then it has different patterns — skips and dual pulses and steady and random modulations and so on. But that’s just mine, because there’re lots of others. I needed it after I stopped taking ibuprofen and used it for maybe five years, then I weaned myself off it. One time the pain hit me for three days straight. Now I can walk it off or distract myself. I got it most when I tried to relax. When I retired in ’85, it started up again. And stress is something that will increase phantom pain, but it depends on the kind of stress. For me, it wasn’t stress from work but family stress. Now, in bed at night, I stretch the leg, raise and lower the leg for 20 minutes just to tire it out.”
I asked Acosta if he had ever tried using Ramachandran’s mirror method, but he suggested that it hadn’t worked for him. He said that when Ramachandran had been conducting his study, he advertised for amputees in the paper and paid them. “We offered to do it for free, but he turned us down. He was seeing amputees with six months or less. Maybe one or two had more time. I read his book and he seemed to be making amputees all the same, but every single one is different. Then one of his students told me that Dr. Ramachandran had told her not to talk to me. I’ve been tainted by that, and so it’s been hard to be objective about him.”
I sent Ramachandran an email asking him about this matter, but he hasn’t responded.
Amputees in Motion is part of the American Coalition of Amputees, an education, advocacy, and support group for the country’s two million amputees. Over 185,000 new amputations are performed in the United States each year, with the highest percentage being performed on patients with Type 2, or adult-onset, diabetes, which takes in more than 90 percent of the 20–30 million diabetics. The number of cases of Type 2 diabetes in the United States is expected to double in the next 25 years, while the Centers for Disease Control and Prevention have anticipated that one out of three Americans born after 2000 will develop diabetes in their lifetime as people grow more sedentary, more overweight, and increasingly committed to a “Western-style” high-fat diet. The vascular destruction caused by diabetes, especially in the lower limbs, can lead to necrosis, gangrene, and amputation. Further amputations, called “revisions,” are often required as the disease progresses. The great majority of these amputees suffer from phantom pain, which is something that Bert Acosta talks about when he visits San Diego amputees in the hospital.
“I tell them the sooner they start walking, the easier it is to stand the discomfort,” he said. “The prosthesis doesn’t hurt the wound or scar because the pressure is on the sides. So you can walk on it very quickly. I know a former sheriff who was walking the day after the operation. And the military gets their people walking right away. I make about ten visits a month, and we have about six steady visitors throughout the county. I’ll go all over the place, even down to Tijuana, because I’m the only one that’s bilingual. The hospitals don’t call us for everyone, just mostly the troubled ones, and we’re not really trained for that. They need a psychiatrist. The best time to see the person is before the amputation. Afterward, they’re in pain; they’re depressed. If you talk to them before, you can convince them their life isn’t over. They don’t need to be limited. The Kiwanis has a program to teach amputees how to ski. We have two quadruple amputees, and they get around better than any of us. One woman walks on her stumps; she said she didn’t like the prosthesis. I asked her why, and she said, ‘How do I put them on?’ But your prosthesis needs to be your best friend. The connection is personal and individual, and each person is going to be different. I use a carbon graphite leg that weighs five pounds, so I can sneak into a room with nobody hearing me. Many legs can clunk. I drive a car with a clutch; it never bothers me. My legs bow outward so many times, my prosthesis can seem not to fit. But that’s all psychological. I’ve always felt my foot, and when I put on my prosthesis I have to make sure my phantom foot fits exactly inside the shoe. If I’m off a degree, I have to put it on again, because my brain wants to walk as it always did.”
Acosta’s description seemed to corroborate what Ramachandran had said about one’s body image being mental. We have an image of ourselves that may not be exactly how we look. We appear fatter, thinner, prettier, uglier than we actually are. The body image of most amputees still includes the missing limb or limbs, and it keeps sending out signals to the limb, which of course can’t be answered, and this is the main source of the phantom, as well as the pain. The mirror image works by sending signals back to the brain that convinces the brain the limb is working properly.
Before talking to anyone at the Naval hospital, I spoke to Teresa Harrison, 37, who suffers from phantom pain in her left arm as a result of a surfing accident, by which I mean she has phantom pain in an arm that still exists.
Teresa had gone out surfing by herself in Coronado late in the day on November 17, 2003. Deciding to take one last run, she paddled out to catch a wave. Instead, the wave flipped her. “I found myself spinning underwater. Everything was gray and murky with flashes of light. I knew something was wrong. I told myself, ‘Teresa, just get your feet on the floor and push up.’ Some kids were surfing not far away. I was about 30 yards out. I shouted to them. They were about 12 or 13. One of the boys swam to shore to get help, while the other held me around the neck, almost strangling me. I told the boy not to hold me like that; I said I could swim to shore, but he wouldn’t let me go.”
The boy, whose name she never knew, had saved her life. The fin of the surfboard had cut through her neck, nicking the carotid artery and shaving a bit of her spine. Blood was pouring from the wound. Teresa also had a fractured rib, a collapsed lung, and nerve damage. A lifeguard held her neck together until the ambulance came.
She woke up in the ICU three days later with her family around her, having come out from West Virginia after being called by Teresa’s daughter. She was badly bruised and had 13 staples in her neck, severe pain whenever she tried to lift herself, and complete paralysis in her left arm. She was 33 years old.
Six months later she had regenerative surgery to repair the nerve damage, but it had little effect. The nerves couldn’t be reattached. However, the surgeon believed he could help her if he rerouted a breathing nerve to the arm. Still the arm remained paralyzed. The muscle had atrophied, and the arm was numb and without feeling. Teresa had spent four years in the Navy and was a long-distance runner. Through sheer stubbornness she did hours and hours of physical therapy and exercise. Eventually, her lung came back. A year after her accident she ran a marathon. But the arm remained paralyzed and without feeling.
“For the first year and a half, I felt nothing,” she said. “I would have my daughter touch my hand, my fingers, and I would have no clue what fingers she was touching. But then from my elbow down to my hand, my arm started throbbing as if it was all going to blow. I’ll have a painful sensation that extends past my fingers and hurts a lot. At times the arm will feel full and tight. The whole arm will feel as if it’s going to pop. It gets flooded with it, like a surge. At the same time, the arm is numb. If I pinch it, I feel nothing. The arm is numb and hurts at the same time.”
“So you can’t move your arm at all?” I asked. We were sitting in a coffee shop in Coronado.
“Well, I can do this.” Teresa took her left arm with her right and laid it on the table between us with the palm upward. She took a deep breath and then another. Each time she took a breath the fingers curled. Because the surgeon had attached a breathing nerve to the arm, the fingers moved whenever she took a deep breath, but they didn’t move enough for her to use them. More than five years after her accident, this was the best she could do. And the arm often hurts, feeling as if it’s about to explode even while remaining numb. The pain will wake her up at night. Now she doesn’t know what to do, whether she should keep the arm or have it amputated, which would at least rid her of the nuisance factor of carrying around its dead weight. Unfortunately, her health-insurance carrier won’t let her see a neurologist again, and her regular doctor doesn’t know enough to help her. Teresa is a pretty woman with short brown hair surrounding her face. She is active and still runs marathons. A mother, she also holds a full-time job.
“I feel like my arm has feelings,” she said, “and I don’t want to hurt its feelings by cutting it off. But it also feels like a dead weight. It gets in the way, and I can’t do anything with it. So I think maybe I should get it amputated.”
I explained to her that getting the arm amputated probably wouldn’t make the pain go away. Instead of phantom pain in a real arm, she’d have phantom pain in a phantom arm. I told her about Ramachandran’s book, and rather dubiously, she wrote down the name.
“If there’s a perfect accident, I think I had it,” she told me. “I was very lucky. I could have died.”
Eventually, my meeting with several amputees in the Naval Medical Center was approved, and one afternoon I was led to Sonja Hanson, the blond and statuesque public affairs officer of Navy Medicine West, where C5 was located. She in turn led me through a maze of hallways, while describing the Amputee Care and Rehabilitation Center and its emphasis on restoring the quality of life that the young men and women had had before their injuries. Also affecting the amputees was depression and, in some cases, post-traumatic stress disorder, or PTSD, which leads to flashbacks of battle conditions and disorientation. As I knew from the many Vietnam veterans I have met, PTSD can continue undiminished, and many have suffered from it for the past 40 years.
Added to the difficulties experienced by the amputees was the intense pain that can accompany phantom-limb syndrome. As Sonja told me, the pain made it particularly difficult to deal with the depression. It was bad enough to be missing one or more limbs and to suffer the effects of other injuries, but the intense phantom pain made everything worse.
I asked her about Dr. Ramachandran and the mirror treatment, but she knew nothing about it. Indeed, even the term “phantom-limb syndrome” was new to her. Again, I was astonished that more than a dozen years after his experiments, his simple procedure was almost unknown. Even though it didn’t help all the participants, it had helped a high percentage, and given its simplicity and economic advantage, it seems almost tragic that it hasn’t become a fundamental part of the program.
What Sonja especially praised was the Wounded Warrior Project, a private nonprofit organization begun by a few veterans and service members shortly after the start of the current Iraq War. The project focused at first on wounded service members who found themselves in military trauma centers without clothes or personal possessions, supplying the wounded with backpacks containing clothes, playing cards, toiletries, a calling card, a CD player, and other items intended to ease their return. Since then, the project has developed into a nationwide organization specializing in peer mentoring, a variety of support programs to assist with the return to civilian life, and sports programs that include activities like football, marathon-running, hunting, mountain-climbing, skiing, swimming, and much more. Everything is designed to give wounded service members a sense of community and return them to a life that most feared they would never have again.
Eventually, Sonja took me into a conference room where several present and former servicemen were seated at a long table. The first person I spoke with was Captain Lonnie Moore, 32, who had lost his right leg above the knee in a bomb blast in Iraq in April 2004. Now he was the western area director of the Wounded Warrior Project and had worked with C5 amputees since the beginning of 2007.
“We work as peer mentors,” he said. “Our job is to be there as someone who listens and answers questions, like ‘How do I learn to drive?’ Absolutely, I tell them there’s a life after their injury. I say it may seem overwhelming now, but you’ll have your life again and walk again and have the same heart and mind and soul that you had before.”
What makes these peer mentors so effective is that they too have suffered injuries. “I was shot by a rocket-propelled grenade that went through my Bradley turret,” said Moore. “Besides the leg, I had a concussion, minor things like that.”
Standing behind Moore was Army Major Brian Belnap, the 35-year-old medical director of the amputee center, who occasionally added his comments to what Moore had said. Neither he nor Moore knew the term “phantom-limb syndrome,” as a description of the condition, although Belnap knew of Ramachandran and had heard of the mirror treatment. “Almost everybody has phantom pain,” he told me.
“When I first see somebody,” said Moore, “they’ll say, ‘I still feel I have my leg or arm or whatever — what does it mean?’ It’s one of the first or second questions they ask. Early on I had a phantom sensation — feeling in my missing foot and calf. Then after a month or two it felt like someone had wrapped a wire around each of my toes and yanked them back and forth. I couldn’t sleep for two weeks. I saw the doctor and received a steroid injection, which helped a little; massage also helped. I tried the mirror treatment, but it wasn’t effective for me. I rarely have the pain now, but I expect it will keep coming back all my life.
“For some people it feels like a stabbed toe, others feel as if their feet have been hit with a hammer, others feel an electric shock. It can consume a lot of their thoughts and be a big drawback in rehab. The military saw the pain as a huge issue right from the start. Each day they’d ask how my pain was.”
So one of Lonnie Moore’s jobs as a peer mentor is to talk to amputees about phantom pain, about the various treatments, and how the pain can diminish with time or even disappear. An increasing sense of urgency accompanies such work. Not mentioned in our discussion was the record number of suicides and attempted suicides among active-duty soldiers. The Department of Defense reports that as of March 1, 2008, 145 active Iraq military have committed suicide since the start of the war. And there are other suicides where the death has been reported as accidental or from friendly fire. But Defense has been reluctant to release these figures, because of what it says about the emotional damage caused by the war. For instance, according to a 2004 report by United Press International, between eight and ten percent of the approximately 12,000 soldiers evacuated from Iraq and Afghanistan to the Landstuhl Regional Medical Center in Germany have been sent to the hospital for psychiatric or behavioral health issues, according to the hospital’s commander, Col. Rhonda Cornum.
In 2007, CBS News submitted a Freedom of Information Act request to the Defense Department asking for the number of active-duty service members who committed suicide between 1995 and 2007. The answer was 2200. This figure would seem to throw doubt on the subsequently stated figure of 145.
Further research by CBS News revealed that in 2005, in 45 states at least 6256 of those who had served in the armed forces committed suicide. In 2007, 121 active-duty soldiers took their lives and about 2000 injured themselves in suicide attempts, according to the U.S. Army Medical Command Suicide Prevention Action Plan. More than half of these incidents occurred after the soldiers had returned to the United States. The suicide rate among nonveterans is 8.3 per 100,000 persons; among veterans it’s between 22.9 and 31.9 per 100,000.
Clearly, there are many reasons for these suicides, but a great number have occurred among those suffering from PTSD or previous wounds or both. As a result, the Wounded Warrior Project not only tries to bring comfort and assistance to the Iraq wounded, it also tries to save lives.
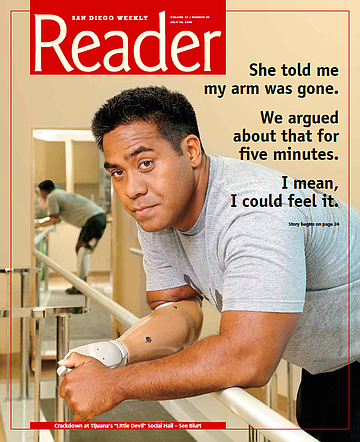
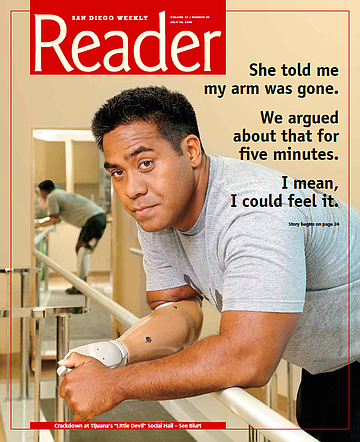
Another soldier I spoke to was Sgt. Wallace — or Wally — Fanene, a 25-year-old Samoan from Temecula. He was wounded on September 8, 2007, and lost his right arm and right leg. He had been in Iraq for 14 months and was a month away from coming home.
“We were on a dismounted patrol in Kirkuk,” he told me, “and I was on point. I saw someone running, and I shouted to everyone to take a knee. I knelt down on a landmine; I sat on it. I knew my leg was gone right when I was hit, but I didn’t feel any pain, and I didn’t know about my arm.”
Fanene was flown immediately to the Landstuhl Regional Medical Facility. “When I came to in the hospital, I still didn’t know my arm was gone. What was left was heavily bandaged, and all I could see was the bandage. I had a tremendous itching in my right hand, and I asked my wife to scratch it. She told me my arm was gone. We argued about that for five minutes. I mean, I could feel it.”
Fanene was sent on to Walter Reed Hospital and then arrived at the Naval Medical Center on September 22. “The pain must have begun once I got here. I was heavily on meds, and as I tried backing off them, the pain started to come hard. It kept me up all night. I’d get it after I got back from rehab — then it was really hard. It felt like needles in every part of my leg and nails in my toes — I mean actual nails, not a metaphor, and it felt like a knife in my leg. It was the most excruciating pain in my life. The wound itself was never as bad. And I never had these feelings in my arm. Two weeks later I started the mirror treatment. I was skeptical at first, but then I said, what the heck. So we tried it and it worked right away. The pain just stopped. Four hours later the pain came back again, and again the mirror helped right away.”
The time between the attacks grew longer. “The pain still comes back, but it’s nowhere as bad as it was. It comes back several times a day. But if it starts to bother me, I use the mirror. I also took Klonopin [a muscle relaxant and anticonvulsant that addresses depression and panic attacks] for about two weeks, but then I stopped. Now it’s been about ten weeks since I was injured, and I’m moving around all right. I’m just now coming to realize what I can and cannot do. And what I’ll be able to do. But my life has changed, there’s no doubt about that. Even so, you have a surprising will to drive on, knowing that the only thing that holds you back is yourself. You move from threshold to threshold. I just got into the pool last week. It was nice to be in the water again. And I’ll surf again. I’ll do what I can until I have to stop.”
Fanene intends to stay in the Army if possible. He’s been married for about two and a half years and has a one-year-old daughter. He’s a big, strong guy, tall, with mocha skin, and muscular as a weightlifter. Yet now and then he looked vulnerable, and there was uncertainty in his eyes. Although he tried to stay optimistic, the future was more than he could imagine. Still, he had seen many amputees in the center as bad off or worse than he was running or going up the climbing wall. He could see what was possible, and there were always people like Lonnie Moore nearby to offer encouragement.
As for the mirror treatment, Major Belnap said it had just started being used at Walter Reed when he left there for San Diego in mid-2007. “My job is as a rehab specialist, so I spend a lot of time dealing with pain, all sorts of pain. So we’re always brainstorming to see what might be done. No two cases are alike. And we’re always looking for therapies without side effects; so any method that doesn’t involve meds or surgery, I’m for it. I work closely with a team of doctors and therapists, both active duty and civil. We need multiple disciplines including mental health. We have to look at the whole picture, like the whole family-support system. It’s a very stressful time. In some cases there’s been a divorce, but in other cases the wives stand by their sides and help a lot. The phantom pain can be very disabling, but it can diminish over time. At Walter Reed we tried acupuncture and meds like Gabapentin, which has been useful in alleviating neuropathic pain. Some it helps, some it doesn’t. You try to use evidence-based meds, so you ask what literature there is out there, and it’s always mixed. The TENS unit often works right after the limb has been taken off, but not for long.”
Nearly 40 amputees are in the center, with three-quarters from the Iraq War, one from Afghanistan, and a number of victims of motorcycle accidents.
“Two weeks after the sutures come out, we fit them with a prosthesis,” said Major Belnap. “Then we speed up the rehab. The sports component has been a big help. You can teach them to ski in less than a day. It gives them confidence that they can do something, and their motivation seems to lessen their phantom pain. It’s inspiring for me to see them; it’s an emotional experience. We have a very robust peer-visitation program with 17 visitors whose job is to listen and answer questions. Many people say they turned the corner after they had their first peer visit. I’ve worked with the phantom pain from the beginning. It takes time, and no magic bullet will take it away. The last-ditch effort would be spinal cord surgery. I really hope to talk to Dr. Ramachandran at some point, but nothing has been set up. We should invite him to come.”
The last person I talked to, under Sonja’s care, was Peter Harsch, 36, a civil prosthetist, blond, fast-talking, and with Hollywood good looks and charm. He showed me the equipment they used in preparing a prosthesis, most of it computerized. A cast is taken and the residual limb scanned and modified on a computer. Then the image is sent over to a carving machine, which produces a copy of the limb. Then heated Duraplex is put around the socket of the copy to make a mold ensuring that the eventual prosthesis will be a perfect fit.
As we moved from room to room, we passed amputees, both men and women, working on treadmills or being fitted. Everyone in contact with the amputees seemed tremendously upbeat, as if the missing limb were just a minor inconvenience, but it wasn’t as superficial as that may seem, because the staff obviously cared deeply about their patients and were doing what they could to make their lives better.
Harsch was particularly enthusiastic about the new technology developed in the past few years. “You’re getting a very smart monkey in the knee,” he told me. “You have four sensors recognizing the ground terrain, evaluating data at 1500 times per second, and motor systems powering the knee, foot, and ankle.” He also spoke about the i-Limb Hand, developed by U.K.-based Touch Bionics, which has five individually powered digits and looks and acts like a real human hand. The hand, according to the company’s website, touchbionics.com, “utilizes the electrical signals generated by the muscles in the remaining portion of the patient’s limb” to hold a coffee cup, slip a key in a lock, offer a business card, and a wide variety of other movements impossible in the past.
“We can reduce the phantom pain with the use of a good prosthesis,” Harsch said. “It really helps to desensitize those nerves. What’s important is which doctors are paying attention to the nerves. So orthopedic surgery is far more effective than vascular surgery. Vascular surgery might try to save the limb, but orthopedic surgery tries to prepare for the prosthesis. But with these guys in here, what they want to do, we try to do. We create a positive vibe. Some people will ask if this sort of work isn’t depressing, but I find it an incredible experience.”
I gathered most of the material for this article at the very end of 2007. Unknown to me at the time was an article on mirror therapy in the November 22 issue of the New England Journal of Medicine, written by a team of doctors and researchers at Walter Reed Army Medical Center. The team used 22 lower-limb amputees separated into three groups. All suffered from phantom pain. Indeed, the article said that phantom pain occurred in more than 90 percent of limb amputees. In a daily 15-minute therapy session, one group without mirrors closed their eyes and imagined moving the amputated limb. A second group used the mirror, but the mirror was covered so they couldn’t see it. In the third group, the patients could see “the reflected image of their intact foot in the mirror.”
After four weeks, two patients in the mental-visualization group reported less pain and four reported more pain. In the covered-mirror group, one patient reported less pain and three said they had more pain. In the mirror group, every single patient reported substantial improvement. Then nine patients from the first two groups were given four weeks of mirror therapy. At the end of that time, eight of those nine also experienced a substantial decrease in pain. Those in the first mirror-therapy group received another four weeks of treatment, and all continued to improve. Because of these results, Navy Cmdr. Jack Tsao, a neurologist at Walter Reed, who was one of the authors of the article, now offers mirror therapy routinely. It is extremely cheap and requires no special training. Indeed, he gives the few instructions to anyone interested by phone or email. He doesn’t know how it works except that the mirror seems to trick the brain into thinking that the missing limb still exists.
One wonders what would have happened if Tsao hadn’t recalled reading an article by Ramachandran while he was still in graduate school. And one wonders how mirror therapy might have helped the two million amputees in this country, many of whom still suffer from bouts of phantom pain. Use of mirror therapy has shown that the sooner it is administered, the more effective it is, although gains have been made no matter how old the amputation. And, again, I am amazed by how long it has taken for this treatment to be put into practice. A lot of pain has been endured unnecessarily.
Then there is my friend Glenn. After writing the above, I went to Home Depot and bought an inexpensive mirror measuring 30 x 36 inches. A little later I brought Glenn over to my house. Following a certain amount of talk, I got him to put on a pair of shorts, remove his prosthesis, and sit on the floor with the mirror separating his two legs and with the damaged leg hidden. “Now wiggle your toes,” I said. “On both feet.”
Glenn looked at me as if I’d said something foolish, but then he wiggled his toes. The toes in the mirror also wiggled. It didn’t look like a reflection; it looked like two separate feet wiggling their toes.
After a moment, Glenn said, “It’s weird. I mean, my other foot is moving its toes. The missing toes. I can feel my toes moving.” All the skepticism was gone from his voice. For a minute or so he happily wiggled the three sets of toes — the real, the reflected, and the phantom. “Think of that,” he said. “How strange.” He moved the foot from side to side, raised it a little. It was as if his missing foot had been restored, and he leaned over to his left to see if the stump was still there. “How does this happen?”
I told him how the brain has a body image and his body image included two feet. The mirror had tricked the brain.
“That’s weird,” he repeated. “That’s really interesting.”
I let him keep the mirror. Of course, he hadn’t been feeling any pain at that particular moment, but now at least, when the pain comes back, he’ll be ready.


Most stories begin with a person or an event. This one begins with a book.
Last summer I read The Brain That Changes Itself by research psychiatrist and psychologist Norman Doidge, M.D., which discusses developments in neuroscience, especially in the area of neuroplasticity. Now, if I were in a bar and the guy on the next stool leaned over and said to me what I’ve just written here, I’d give a wave to the bouncer. But hang on.
When I was in school, I was given two pieces of information about the brain that, well, stuck in my brain. The first was that the brain was hardwired, meaning that each bit of the brain had a specific function and if that bit were damaged then that particular function was lost forever. The second piece of information was that even though the brain consisted of billions of nerve cells called neurons, I was constantly losing them and I would never get them back.
As a kid, it seemed I was so rich in neurons that the loss caused by a few six-packs during the week or a rough pickup football game without a helmet meant nothing. After all, I was a billionaire.
But as I moved into old age, it seemed I could feel windy places between my ears where megalopolises of neurons used to be situated, dank caverns inhabited by gloomy question marks bent over smoking piles of dead synapses. Some days it seemed as if I only had about 475 neurons left. Some people hear a ringing in their ears? I heard creaking.
Then I read Doidge’s book and learned that all that was a lot of baloney. If one part of the brain is damaged, its function can often be picked up by another part through the creation of new neural pathways. This has resulted in vast improvements and even cures in a number of conditions, from stroke to irrational compulsions, worries, and obsessions. It has also led to new ways of fixing learning problems and sharpening perception and memory. And this is only the beginning of the list.
Those lost neurons? If you don’t watch too much TV and continue to read books, a sizeable number can be replaced.
When I finished the book, I read a few others on the topic and it turned out that one of the top neuroplasticity guys was at University of California, San Diego: Dr. V.S. Ramachandran, who is director of the Center for Brain and Cognition and professor of psychology and neuroscience. His most recent book, The Man with the Phantom Twin, came out in January, and he has published a handful of other books and well over 150 articles and has enough medals, awards, and certificates of merit to fill a large living room. Newsweek has named him one of the hundred most important people to watch in the 21st Century.
One of Ramachandran’s books, Phantoms in the Brain (1998), has a section about phantom-limb syndrome, a condition found in nearly all amputees that makes them experience feeling in the missing limb, as well as feeling that they can move the limbs, as in waving goodbye or kicking a ball. Many people whose bladders have been removed (or genitals or rectums or uteruses or ulcers) can also feel phantom sensations — but that is another story.
Many of those who lost a limb have also experienced intense pain in the phantom limb, pain that might keep them awake night after night and continue for years. Well, Ramachandran invented a device that cured or substantially helped a majority of the amputees he worked with who suffered from this pain. And what struck me most was that the device only cost a few bucks.
Before I describe this gadget, let me describe my friend Glenn, who cracked up his motorcycle in 1991 when he was in his 20s. Swerving to the left to avoid an oncoming car, he hit the curb, and the motorcycle toppled over and mushed his left leg. When he woke up in the hospital, his leg, below the knee, was gone. About 4500 men and women are killed on motorcycles each year, and about 85,000 are injured. A fair number of those are part of the approximately two million amputees in the U.S.
What Glenn soon discovered was that the leg didn’t feel gone. He could move his phantom toes, waggle his phantom ankle. At times it tingled as if it had gone to sleep. Most disturbing, at times it felt as if a knife were being driven into it. The pain would often occur when he got home from work and was trying to relax. Or it would occur at night: a phantom knife blade through the phantom foot to make him jump out of bed.
The tingling sensations and waggling of the phantom toes can occur every day. The pain has become less frequent over time; it happens now perhaps once a month. Still, it has never gone away. Glenn is a tall, handsome guy, over six feet, with jet-black hair and a neatly trimmed beard. Mostly, you wouldn’t notice that he has a fake leg, but if he’s tired he’ll limp a little. “They’re heavy,” he told me, “even the expensive ones. They’re always dragging at you.”
The number of amputees who suffer from phantom pain ranges from 50 to 95 percent, depending on which specialist is asked, but the most agreed upon number is around 75 percent. Usually it develops soon after amputation, but it can also begin after a few months or even years. For some people it might get better after a year or two, for others it never stops. Often the pain comes in bursts several times a day, but some experience it less than once a month. A much smaller percentage have it constantly. With missing limbs, the pain often occurs at the end of the limb, or it feels as if the limb is shorter or twisted into a painful position, or as if something is being jabbed into it, or as if it’s on fire. Stress and anxiety can affect the pain, even changes in the weather.
Aspirin gives no relief, but anticonvulsant drugs and heavy painkillers like morphine have helped some amputees. Others have been helped by a transcutaneous electrical nerve stimulator, or TENS, a battery-driven device about the size of an iPod that delivers electrical impulses to stimulate nerves in the painful area. Somewhat more effective has been a spinal cord stimulator, an electric impulse-generating device implanted near the spinal cord. Hypnosis, acupuncture, biofeedback, vibration therapy, massage, yoga, ice packs, heating pads, and even steroid shots have also been useful. But what seems most significant is that nothing helps very much. The pain is often most severe when the prosthesis is removed, and so patients are encouraged to use the prosthesis as much as possible.
According to Doidge’s book, Ramachandran’s research led him to think that the absence of feedback from the missing limb to the brain leads not only to the phantoms but to phantom pain. “The brain’s motor center might send commands for the hand muscles to contract but, getting no feedback that the hand has moved, it escalates its command” until, for instance, it feels as if the fingernails are digging into the palm. This oversimplifies Ramachandran’s findings, but he felt that the phantoms were a result of the brain’s mistaken body image. If the image were reinforced, he reasoned, the pain might vanish.
Advances in prosthetic technology have been hugely affected by the Iraq War, and by 2004 new prosthetics were coming onto the market that seemed more products of science fiction than medical technology. The Otto Bock C-leg has a battery-powered “onboard” microprocessor that controls knee movement and communicates with a computer through Bluetooth technology. It can switch between two modes of activity with several taps of the toe.
The C-leg, however, is receiving serious competition from the Ossur Bionic Power Knee, which can synchronize movement with the sound leg to “lift the user to standing from a seated position; support the user while ascending inclines; and power them upstairs.” When the user is walking, the knee’s pendulum motion swings it forward, senses the changing terrain, and “actively lifts the heel off the ground,” according to Ossur’s website. By means of “artificial proprioception,” which is a person’s awareness of his or her posture, movement, balance, and location, the knee “anticipates and responds to the appropriate function required for the next prosthetic step.” There are also power heels to give the walker a boost so the prosthesis won’t, in Glenn’s words, “always [be] dragging at you.”
Yet these bionic prosthetics are nothing compared to what is currently in development. In February, the Defense Advanced Research Projects Agency (DARPA) awarded a contract to the Applied Physics Laboratory at Johns Hopkins University to finish work on a mechanical arm “that will look, feel and perform like a normal limb,” according to the online magazine Gizmag. The Johns Hopkins laboratory, leading a team drawn from about 30 organizations, had already developed two prototypes of prosthetic arms. The first is an arm that “can be controlled naturally, provide sensory feedback and allow for eight degrees of freedom.” The best prosthetic arms now on the market provide for only three degrees of movement. The second prototype uses 25 individual joints “that approach the natural speed and range of motions of the human limb…[and] are complemented by a range of emerging neural integration strategies,” meaning they can be wired to the brain through the nervous system. You think your hand into motion and it moves. The arm should be ready for regulatory clearance in under two years.
So far the Iraq War has led to amputations for more than 750 servicemen and women. The high number is due in part to the body armor that protects the trunk. Without it, many of these soldiers would have died. In fact, about 92 percent of those wounded in Iraq survive their wounds, as opposed to 76 percent in Vietnam.
Founded in 1958 in response to the Sputnik surprise, DARPA is responsible for developing new military technology, while its prosthetic program tries to provide the best “medical and rehabilitative technologies for military personnel injured in the line of duty,” according to Gizmag. The requirement that the soldier be injured in the line of duty may explain what was for me an odd discrepancy. Between 2001 and 2007, the Veterans Administration performed more than 17,000 amputations on former military personnel, most of whom suffered from diabetes. Although these amputees provide a steady business for the prosthetics industry, their needs have not led to anything like DARPA’s “Revolutionizing Prosthetics” program, which has provided funds for “the most advanced medical and rehabilitative technologies.” Nor would these VA amputees necessarily benefit from the new developments. Coverage of prosthetic limbs has been limited to $2500 or $5000 a year by many private health plans. Or the plans will pay for only one device per limb over the patient’s lifetime. And the insurance lobby has been trying to reduce this amount. The cost of basic prostheses ranges between $3000 and $15,000, while models resulting from the new technologies can be priced at more than $40,000.
As with any war, sympathy and attention goes to the soldiers injured in combat, and of these Iraq has provided nearly 100,000. The first Iraq War amputees were treated at Walter Reed Army Medical Center outside of Washington. Then, as their number increased, the Department of Defense opened a second amputee care center at Brooke Army Medical Center at Fort Houston in San Antonio, Texas, in early 2005.
A third amputee care center was officially opened in San Diego on October 15 as part of the Comprehensive Combat Casualty Care Center, or C5, of the Naval Medical Center. The 30,000-square-foot facility is not only a showpiece of new technology, with an accurate motion-capture system and an advanced bionic technology room used for gait adjustment, but also includes a 3500-square-foot obstacle course with a 30-foot climbing wall. It cost $4.4 million to build and another $4 million to outfit and staff. A major focus of C5 is to get the amputees moving as soon as possible, taking them on ski trips, having them engage in sports, and even learning to surf. I decided to visit the facility, but before I spoke to the wounded soldiers, I wanted to talk to Dr. Ramachandran at UCSD.
Born in India in the southern province of Tamil Nadu, Ramachandran received his medical degree from Stanley Medical College in Madras, specializing in neurology, and his Ph.D. in psychology from Trinity College at the University of Cambridge. He also studied at Oxford. The British scientist and writer Richard Dawkins has called him “the Marco Polo of neuroscience” because of his explorations into uncharted territories.
Ramachandran’s early work was on human visual perception, using optical illusions to study the brain mechanisms that underlie visual processing. And it was illusions that became key in working with phantom limbs in the mid-’90s. Later, his work with phantom limbs led to using techniques of visual feedback to help stroke victims recover the use of arm and leg functions.
Since then, he has kept his focus on various neurological syndromes to study their underlying mental functions. He and his colleagues have written articles on synesthesia, in which letters might be linked with colors, or sounds with smells. Then came papers on Capgras delusion, in which a person believes that his family members or friends have been replaced by imposters. He has also written about autism, apotemnophilia (in which a patient has a strong desire to amputate one of his or her limbs), and mirror agnosia, where four right-hemisphere stroke patients “were indifferent to objects in their left visual field even though they were not blind,” according to Ramachandran.
In “The Emerging Mind,” the first of five Reith Lectures for the BBC in 2003, Ramachandran described the vast scope of the brain as well as the source of its fascination for him. “The brain is made up of one hundred billion nerve cells, or ‘neurons,’ which are the basic structural and function units of the nervous system. Each neuron makes something like a thousand to ten thousand contacts with other neurons, and these points of contact are called synapses, where exchange of information occurs. And based on this information, someone has calculated that the number of possible permutations and combinations of brain activity, in other words the number of brain states, exceeds the number of elementary particles in the known universe.… It never ceases to amaze me that all the richness of our mental life — all our feelings, our emotions, our thoughts, our ambitions, our love life, our religious sentiments, and even what each of us regards as his own intimate private self — is simply the activity of these little specks of jelly in your head, in your brain. There is nothing else.”
Ramachandran described his work to me as we sat in his office, which was as comfortable as a private study or den and decorated with artwork from Asia and Europe, a bust of Freud, a picture of Darwin, odd little antique machines, fossils, bric-a-brac.
He is a tall, dapper man in his late 50s with a mustache and receding curly black hair. He was wearing black shoes, black pants, a black shirt, and a brown-flecked jacket. Handsome and rather aristocratic, he has the slightly ironic and impatient manner of someone who is already thinking about what he needs to do next and what he must do after that. He speaks with nearly no accent other than rolling his R’s and uses quick rushes of phrases between studied transitions to create a striking fast-and-slow pattern that makes his mental gears appear almost visible.
The term “phantom limb” was first used by an English doctor in 1872 in a paper describing how amputees could experience sensations in their missing or phantom limbs. Ramachandran explained that 98 percent of amputees experience phantom sensation and that an innate component of our sense of body image seems to be “hardwired” into our brains, so that even congenitally limbless patients can still feel sensation in the missing limbs. Pain, he argues, first occurs in the brain, and then the sensation or impulse is sent to the damaged or affected area. When I jam my finger in a car door, it’s not the finger that hurts first; rather, the brain evaluates the damage and sends the sensation to the finger. That’s when I cry, “Ouch!” In the case of phantom limbs, the sensation will be mostly a tingling in the missing limb, but three quarters or more can experience excruciating pain. Ramachandran has a great fondness for what he calls “five-minute experiments” that changed the world, such as Galileo’s use of a cardboard tube and two lenses to show that the earth is not the center of the universe, or his experiment of dropping a ten-pound and a one-pound cannonball from the Leaning Tower of Pisa to show that falling bodies fall at the same speed. And there is Michael Faraday’s experiment with a bar magnet, iron filings, and a sheet of paper to demonstrate the presence of a magnetic field, as well as Newton’s work with a simple prism to show that white light is a composite of different colors.
These “five-minute experiments” influenced Ramachandran in trying to solve the problem of phantom pain with a simple, noninvasive treatment using about $20 worth of material. He constructed a “virtual reality box” by setting a long mirror horizontally inside a cardboard box from which the top and front surfaces had been removed. The patient places his good arm (or leg) and the remaining stump in the box separated by the mirror, so that the reflection of the good hand creates the illusion of two hands. The patient then simultaneously tries to move both his hand and the phantom and has the illusion of seeing his phantom hand move, while the actual phantom also feels as if it’s moving. The reflection gives him positive visual feedback that tells the brain that his phantom hand is moving just as it should. In the case of a man whose phantom fist feels clenched, the mirror box creates the illusion that the clenched fist can open. By working with the box, the man learns to unclench his phantom hand. What was discovered in these cases was that the data coming from the different sense modules in the brain can change as the brain updates its model of reality in response to new information. Of course, it was all more complicated than my paraphrase suggests, but my main interest was the effect of these experiments on the patients.
“Two-thirds got great relief in three to six weeks, sometimes sooner,” Ramachandran told me. “In many cases the phantom goes away completely, but if the pain happens to come back, then the box can be used again.”
To give me a better sense of how it worked, he took me downstairs to a room where a tall mirror about two feet wide rose vertically from the floor.
“Stretch out your right hand horizontally across the right side of the mirror,” he told me, “and move a little to the right so you can see your right hand and its reflection, but not your left hand.”
It took some fiddling, but in a few moments I was staring down at my right arm and its reflection, while my left hand was hidden behind the mirror.
“Now wiggle the fingers of your right hand and look at the reflection, while keeping your left hand still.”
As I wiggled my fingers and looked at the reflection, I felt a tingling in my hidden left hand and the sensation that the fingers of my left hand were wiggling as well. The visual feedback from the mirror had tricked my brain into believing that my left hand was moving, and the brain had responded by sending out the appropriate sensations.
But Ramachandran’s interest is in research rather than in the clinical application of his findings, and he knew little about whether his mirror treatment was being used in clinics. Once he is done with a particular facet of research, he hurries on to something else. He had had no contact with medical staff at the Naval hospital, although he said, rather vaguely, “I gather that talks have begun.”
A Google search, however, informed me that the therapeutic use of mirror therapy is increasing. At Walter Reed Hospital the therapy is given to military amputees. This was initiated in 2007 by a Navy neurologist, who was trying to help soldiers suffering from phantom pain. He recalled reading in graduate school a paper by Ramachandran about helping patients with phantom pain with a $20 mirror. But I’ll return to that later.
What struck me most was that more than a dozen years had gone by between Ramachandran’s initial discoveries and their application. That meant that well over a million American amputees had been suffering needlessly from phantom pain.
“The medical community is very conservative and resistant,” Ramachandran told me. “They don’t really care about rehabilitation that much. They leave it up to the therapists. I’m talking about inertia rather than skepticism. They accept it intellectually, but then back in the hospital they get busy with other work and seem to forget about it.”
One possible reason why doctors and clinics have been slow in using the mirror treatment for amputees is its very simplicity. Instead, they find greater credibility in more complicated and costly systems. For instance, scientists at the University of Manchester, U.K., have developed a virtual-reality system that gives amputees the illusion that the missing limb is still there and can function. The scientists referred to Ramachandran’s work with the mirror box, saying they would use it with their virtual-reality technologies to create a more effective treatment for phantom pain.
Ramachandran scoffed at this. “Virtual-reality labs are a waste of money, and they don’t work as well as the simple mirror box, except when working with double amputees. But for many people, the more expensive something is, the more credible it is.”
The next morning I sought out a representative of San Diego’s Amputees in Motion, an amputee support group that Ramachandran had mentioned. The head of the group is Bert Acosta, who lives out near Grossmont College in a two-story Spanish-style house with three huge trees in the front yard.
Acosta is a retired engineer in his 70s who lost a leg in a motorcycle accident 38 years ago. The local Amputees in Motion was started in 1973, and Acosta joined soon afterward. Although the group has a membership list of 500, only about 15 are active. These members visit hospitals to talk to recent amputees about what they might expect and how they might deal with it. The great majority of the amputees are diabetic, with about 1 in 50 being the result of a motorcycle accident. Acosta is a friendly man and a good talker. We sat in his living room.
“After they took off my leg,” he said, “it got infected in the hospital and I got gangrene and the doctor thought I’d die by the end of the day. He said I had one chance out of ten thousand of surviving because I was so weak. I woke up the next day, and they’d amputated my left leg four inches above the knee. But I still felt my toes; it felt like I had a tourniquet on them. Then the pain got worse. My surgeon handed me a bottle with about a dozen pills. ‘Take them when you want,’ he said, ‘but don’t call me again.’ You see, he was afraid I’d become addicted. I’ve met several hundred amputees and not known anyone who didn’t have phantom pain. I saw a man yesterday who had just had his leg amputated, and he complained of charley horses. Some feel like molten lead is being poured on their leg; another will say it feels like a cold ice pick being shoved deep into the bone marrow; a third person will say it feels like the leg is being pulled and the nerves stretched. I can have the molten lead feeling or the stretched feeling. The pain is irregular. It will happen for 10 minutes, stop for 20, come back for 5, then stop and come back again. I don’t have the pain when I’m walking or working, but when I’m home sitting down, then my leg starts tingling. Others, it hurts when they walk and stops hurting when they take off the prosthesis. Fifty people with the same amputation could have 50 different responses. Many don’t do anything about it. For me, after all this time, it’s more of an inconvenience. It feels as if my shoe is too tight. Even if I’m not wearing my prosthesis, it can feel like the shoe is too tight.”
Acosta showed me his small TENS unit, which sends out a series of different electronic waves of different strengths, so each person’s unit has to be individually set.
“The TENS shocks you on degrees of 1 to 100, and then it has different patterns — skips and dual pulses and steady and random modulations and so on. But that’s just mine, because there’re lots of others. I needed it after I stopped taking ibuprofen and used it for maybe five years, then I weaned myself off it. One time the pain hit me for three days straight. Now I can walk it off or distract myself. I got it most when I tried to relax. When I retired in ’85, it started up again. And stress is something that will increase phantom pain, but it depends on the kind of stress. For me, it wasn’t stress from work but family stress. Now, in bed at night, I stretch the leg, raise and lower the leg for 20 minutes just to tire it out.”
I asked Acosta if he had ever tried using Ramachandran’s mirror method, but he suggested that it hadn’t worked for him. He said that when Ramachandran had been conducting his study, he advertised for amputees in the paper and paid them. “We offered to do it for free, but he turned us down. He was seeing amputees with six months or less. Maybe one or two had more time. I read his book and he seemed to be making amputees all the same, but every single one is different. Then one of his students told me that Dr. Ramachandran had told her not to talk to me. I’ve been tainted by that, and so it’s been hard to be objective about him.”
I sent Ramachandran an email asking him about this matter, but he hasn’t responded.
Amputees in Motion is part of the American Coalition of Amputees, an education, advocacy, and support group for the country’s two million amputees. Over 185,000 new amputations are performed in the United States each year, with the highest percentage being performed on patients with Type 2, or adult-onset, diabetes, which takes in more than 90 percent of the 20–30 million diabetics. The number of cases of Type 2 diabetes in the United States is expected to double in the next 25 years, while the Centers for Disease Control and Prevention have anticipated that one out of three Americans born after 2000 will develop diabetes in their lifetime as people grow more sedentary, more overweight, and increasingly committed to a “Western-style” high-fat diet. The vascular destruction caused by diabetes, especially in the lower limbs, can lead to necrosis, gangrene, and amputation. Further amputations, called “revisions,” are often required as the disease progresses. The great majority of these amputees suffer from phantom pain, which is something that Bert Acosta talks about when he visits San Diego amputees in the hospital.
“I tell them the sooner they start walking, the easier it is to stand the discomfort,” he said. “The prosthesis doesn’t hurt the wound or scar because the pressure is on the sides. So you can walk on it very quickly. I know a former sheriff who was walking the day after the operation. And the military gets their people walking right away. I make about ten visits a month, and we have about six steady visitors throughout the county. I’ll go all over the place, even down to Tijuana, because I’m the only one that’s bilingual. The hospitals don’t call us for everyone, just mostly the troubled ones, and we’re not really trained for that. They need a psychiatrist. The best time to see the person is before the amputation. Afterward, they’re in pain; they’re depressed. If you talk to them before, you can convince them their life isn’t over. They don’t need to be limited. The Kiwanis has a program to teach amputees how to ski. We have two quadruple amputees, and they get around better than any of us. One woman walks on her stumps; she said she didn’t like the prosthesis. I asked her why, and she said, ‘How do I put them on?’ But your prosthesis needs to be your best friend. The connection is personal and individual, and each person is going to be different. I use a carbon graphite leg that weighs five pounds, so I can sneak into a room with nobody hearing me. Many legs can clunk. I drive a car with a clutch; it never bothers me. My legs bow outward so many times, my prosthesis can seem not to fit. But that’s all psychological. I’ve always felt my foot, and when I put on my prosthesis I have to make sure my phantom foot fits exactly inside the shoe. If I’m off a degree, I have to put it on again, because my brain wants to walk as it always did.”
Acosta’s description seemed to corroborate what Ramachandran had said about one’s body image being mental. We have an image of ourselves that may not be exactly how we look. We appear fatter, thinner, prettier, uglier than we actually are. The body image of most amputees still includes the missing limb or limbs, and it keeps sending out signals to the limb, which of course can’t be answered, and this is the main source of the phantom, as well as the pain. The mirror image works by sending signals back to the brain that convinces the brain the limb is working properly.
Before talking to anyone at the Naval hospital, I spoke to Teresa Harrison, 37, who suffers from phantom pain in her left arm as a result of a surfing accident, by which I mean she has phantom pain in an arm that still exists.
Teresa had gone out surfing by herself in Coronado late in the day on November 17, 2003. Deciding to take one last run, she paddled out to catch a wave. Instead, the wave flipped her. “I found myself spinning underwater. Everything was gray and murky with flashes of light. I knew something was wrong. I told myself, ‘Teresa, just get your feet on the floor and push up.’ Some kids were surfing not far away. I was about 30 yards out. I shouted to them. They were about 12 or 13. One of the boys swam to shore to get help, while the other held me around the neck, almost strangling me. I told the boy not to hold me like that; I said I could swim to shore, but he wouldn’t let me go.”
The boy, whose name she never knew, had saved her life. The fin of the surfboard had cut through her neck, nicking the carotid artery and shaving a bit of her spine. Blood was pouring from the wound. Teresa also had a fractured rib, a collapsed lung, and nerve damage. A lifeguard held her neck together until the ambulance came.
She woke up in the ICU three days later with her family around her, having come out from West Virginia after being called by Teresa’s daughter. She was badly bruised and had 13 staples in her neck, severe pain whenever she tried to lift herself, and complete paralysis in her left arm. She was 33 years old.
Six months later she had regenerative surgery to repair the nerve damage, but it had little effect. The nerves couldn’t be reattached. However, the surgeon believed he could help her if he rerouted a breathing nerve to the arm. Still the arm remained paralyzed. The muscle had atrophied, and the arm was numb and without feeling. Teresa had spent four years in the Navy and was a long-distance runner. Through sheer stubbornness she did hours and hours of physical therapy and exercise. Eventually, her lung came back. A year after her accident she ran a marathon. But the arm remained paralyzed and without feeling.
“For the first year and a half, I felt nothing,” she said. “I would have my daughter touch my hand, my fingers, and I would have no clue what fingers she was touching. But then from my elbow down to my hand, my arm started throbbing as if it was all going to blow. I’ll have a painful sensation that extends past my fingers and hurts a lot. At times the arm will feel full and tight. The whole arm will feel as if it’s going to pop. It gets flooded with it, like a surge. At the same time, the arm is numb. If I pinch it, I feel nothing. The arm is numb and hurts at the same time.”
“So you can’t move your arm at all?” I asked. We were sitting in a coffee shop in Coronado.
“Well, I can do this.” Teresa took her left arm with her right and laid it on the table between us with the palm upward. She took a deep breath and then another. Each time she took a breath the fingers curled. Because the surgeon had attached a breathing nerve to the arm, the fingers moved whenever she took a deep breath, but they didn’t move enough for her to use them. More than five years after her accident, this was the best she could do. And the arm often hurts, feeling as if it’s about to explode even while remaining numb. The pain will wake her up at night. Now she doesn’t know what to do, whether she should keep the arm or have it amputated, which would at least rid her of the nuisance factor of carrying around its dead weight. Unfortunately, her health-insurance carrier won’t let her see a neurologist again, and her regular doctor doesn’t know enough to help her. Teresa is a pretty woman with short brown hair surrounding her face. She is active and still runs marathons. A mother, she also holds a full-time job.
“I feel like my arm has feelings,” she said, “and I don’t want to hurt its feelings by cutting it off. But it also feels like a dead weight. It gets in the way, and I can’t do anything with it. So I think maybe I should get it amputated.”
I explained to her that getting the arm amputated probably wouldn’t make the pain go away. Instead of phantom pain in a real arm, she’d have phantom pain in a phantom arm. I told her about Ramachandran’s book, and rather dubiously, she wrote down the name.
“If there’s a perfect accident, I think I had it,” she told me. “I was very lucky. I could have died.”
Eventually, my meeting with several amputees in the Naval Medical Center was approved, and one afternoon I was led to Sonja Hanson, the blond and statuesque public affairs officer of Navy Medicine West, where C5 was located. She in turn led me through a maze of hallways, while describing the Amputee Care and Rehabilitation Center and its emphasis on restoring the quality of life that the young men and women had had before their injuries. Also affecting the amputees was depression and, in some cases, post-traumatic stress disorder, or PTSD, which leads to flashbacks of battle conditions and disorientation. As I knew from the many Vietnam veterans I have met, PTSD can continue undiminished, and many have suffered from it for the past 40 years.
Added to the difficulties experienced by the amputees was the intense pain that can accompany phantom-limb syndrome. As Sonja told me, the pain made it particularly difficult to deal with the depression. It was bad enough to be missing one or more limbs and to suffer the effects of other injuries, but the intense phantom pain made everything worse.
I asked her about Dr. Ramachandran and the mirror treatment, but she knew nothing about it. Indeed, even the term “phantom-limb syndrome” was new to her. Again, I was astonished that more than a dozen years after his experiments, his simple procedure was almost unknown. Even though it didn’t help all the participants, it had helped a high percentage, and given its simplicity and economic advantage, it seems almost tragic that it hasn’t become a fundamental part of the program.
What Sonja especially praised was the Wounded Warrior Project, a private nonprofit organization begun by a few veterans and service members shortly after the start of the current Iraq War. The project focused at first on wounded service members who found themselves in military trauma centers without clothes or personal possessions, supplying the wounded with backpacks containing clothes, playing cards, toiletries, a calling card, a CD player, and other items intended to ease their return. Since then, the project has developed into a nationwide organization specializing in peer mentoring, a variety of support programs to assist with the return to civilian life, and sports programs that include activities like football, marathon-running, hunting, mountain-climbing, skiing, swimming, and much more. Everything is designed to give wounded service members a sense of community and return them to a life that most feared they would never have again.
Eventually, Sonja took me into a conference room where several present and former servicemen were seated at a long table. The first person I spoke with was Captain Lonnie Moore, 32, who had lost his right leg above the knee in a bomb blast in Iraq in April 2004. Now he was the western area director of the Wounded Warrior Project and had worked with C5 amputees since the beginning of 2007.
“We work as peer mentors,” he said. “Our job is to be there as someone who listens and answers questions, like ‘How do I learn to drive?’ Absolutely, I tell them there’s a life after their injury. I say it may seem overwhelming now, but you’ll have your life again and walk again and have the same heart and mind and soul that you had before.”
What makes these peer mentors so effective is that they too have suffered injuries. “I was shot by a rocket-propelled grenade that went through my Bradley turret,” said Moore. “Besides the leg, I had a concussion, minor things like that.”
Standing behind Moore was Army Major Brian Belnap, the 35-year-old medical director of the amputee center, who occasionally added his comments to what Moore had said. Neither he nor Moore knew the term “phantom-limb syndrome,” as a description of the condition, although Belnap knew of Ramachandran and had heard of the mirror treatment. “Almost everybody has phantom pain,” he told me.
“When I first see somebody,” said Moore, “they’ll say, ‘I still feel I have my leg or arm or whatever — what does it mean?’ It’s one of the first or second questions they ask. Early on I had a phantom sensation — feeling in my missing foot and calf. Then after a month or two it felt like someone had wrapped a wire around each of my toes and yanked them back and forth. I couldn’t sleep for two weeks. I saw the doctor and received a steroid injection, which helped a little; massage also helped. I tried the mirror treatment, but it wasn’t effective for me. I rarely have the pain now, but I expect it will keep coming back all my life.
“For some people it feels like a stabbed toe, others feel as if their feet have been hit with a hammer, others feel an electric shock. It can consume a lot of their thoughts and be a big drawback in rehab. The military saw the pain as a huge issue right from the start. Each day they’d ask how my pain was.”
So one of Lonnie Moore’s jobs as a peer mentor is to talk to amputees about phantom pain, about the various treatments, and how the pain can diminish with time or even disappear. An increasing sense of urgency accompanies such work. Not mentioned in our discussion was the record number of suicides and attempted suicides among active-duty soldiers. The Department of Defense reports that as of March 1, 2008, 145 active Iraq military have committed suicide since the start of the war. And there are other suicides where the death has been reported as accidental or from friendly fire. But Defense has been reluctant to release these figures, because of what it says about the emotional damage caused by the war. For instance, according to a 2004 report by United Press International, between eight and ten percent of the approximately 12,000 soldiers evacuated from Iraq and Afghanistan to the Landstuhl Regional Medical Center in Germany have been sent to the hospital for psychiatric or behavioral health issues, according to the hospital’s commander, Col. Rhonda Cornum.
In 2007, CBS News submitted a Freedom of Information Act request to the Defense Department asking for the number of active-duty service members who committed suicide between 1995 and 2007. The answer was 2200. This figure would seem to throw doubt on the subsequently stated figure of 145.
Further research by CBS News revealed that in 2005, in 45 states at least 6256 of those who had served in the armed forces committed suicide. In 2007, 121 active-duty soldiers took their lives and about 2000 injured themselves in suicide attempts, according to the U.S. Army Medical Command Suicide Prevention Action Plan. More than half of these incidents occurred after the soldiers had returned to the United States. The suicide rate among nonveterans is 8.3 per 100,000 persons; among veterans it’s between 22.9 and 31.9 per 100,000.
Clearly, there are many reasons for these suicides, but a great number have occurred among those suffering from PTSD or previous wounds or both. As a result, the Wounded Warrior Project not only tries to bring comfort and assistance to the Iraq wounded, it also tries to save lives.
Another soldier I spoke to was Sgt. Wallace — or Wally — Fanene, a 25-year-old Samoan from Temecula. He was wounded on September 8, 2007, and lost his right arm and right leg. He had been in Iraq for 14 months and was a month away from coming home.
“We were on a dismounted patrol in Kirkuk,” he told me, “and I was on point. I saw someone running, and I shouted to everyone to take a knee. I knelt down on a landmine; I sat on it. I knew my leg was gone right when I was hit, but I didn’t feel any pain, and I didn’t know about my arm.”
Fanene was flown immediately to the Landstuhl Regional Medical Facility. “When I came to in the hospital, I still didn’t know my arm was gone. What was left was heavily bandaged, and all I could see was the bandage. I had a tremendous itching in my right hand, and I asked my wife to scratch it. She told me my arm was gone. We argued about that for five minutes. I mean, I could feel it.”
Fanene was sent on to Walter Reed Hospital and then arrived at the Naval Medical Center on September 22. “The pain must have begun once I got here. I was heavily on meds, and as I tried backing off them, the pain started to come hard. It kept me up all night. I’d get it after I got back from rehab — then it was really hard. It felt like needles in every part of my leg and nails in my toes — I mean actual nails, not a metaphor, and it felt like a knife in my leg. It was the most excruciating pain in my life. The wound itself was never as bad. And I never had these feelings in my arm. Two weeks later I started the mirror treatment. I was skeptical at first, but then I said, what the heck. So we tried it and it worked right away. The pain just stopped. Four hours later the pain came back again, and again the mirror helped right away.”
The time between the attacks grew longer. “The pain still comes back, but it’s nowhere as bad as it was. It comes back several times a day. But if it starts to bother me, I use the mirror. I also took Klonopin [a muscle relaxant and anticonvulsant that addresses depression and panic attacks] for about two weeks, but then I stopped. Now it’s been about ten weeks since I was injured, and I’m moving around all right. I’m just now coming to realize what I can and cannot do. And what I’ll be able to do. But my life has changed, there’s no doubt about that. Even so, you have a surprising will to drive on, knowing that the only thing that holds you back is yourself. You move from threshold to threshold. I just got into the pool last week. It was nice to be in the water again. And I’ll surf again. I’ll do what I can until I have to stop.”
Fanene intends to stay in the Army if possible. He’s been married for about two and a half years and has a one-year-old daughter. He’s a big, strong guy, tall, with mocha skin, and muscular as a weightlifter. Yet now and then he looked vulnerable, and there was uncertainty in his eyes. Although he tried to stay optimistic, the future was more than he could imagine. Still, he had seen many amputees in the center as bad off or worse than he was running or going up the climbing wall. He could see what was possible, and there were always people like Lonnie Moore nearby to offer encouragement.
As for the mirror treatment, Major Belnap said it had just started being used at Walter Reed when he left there for San Diego in mid-2007. “My job is as a rehab specialist, so I spend a lot of time dealing with pain, all sorts of pain. So we’re always brainstorming to see what might be done. No two cases are alike. And we’re always looking for therapies without side effects; so any method that doesn’t involve meds or surgery, I’m for it. I work closely with a team of doctors and therapists, both active duty and civil. We need multiple disciplines including mental health. We have to look at the whole picture, like the whole family-support system. It’s a very stressful time. In some cases there’s been a divorce, but in other cases the wives stand by their sides and help a lot. The phantom pain can be very disabling, but it can diminish over time. At Walter Reed we tried acupuncture and meds like Gabapentin, which has been useful in alleviating neuropathic pain. Some it helps, some it doesn’t. You try to use evidence-based meds, so you ask what literature there is out there, and it’s always mixed. The TENS unit often works right after the limb has been taken off, but not for long.”
Nearly 40 amputees are in the center, with three-quarters from the Iraq War, one from Afghanistan, and a number of victims of motorcycle accidents.
“Two weeks after the sutures come out, we fit them with a prosthesis,” said Major Belnap. “Then we speed up the rehab. The sports component has been a big help. You can teach them to ski in less than a day. It gives them confidence that they can do something, and their motivation seems to lessen their phantom pain. It’s inspiring for me to see them; it’s an emotional experience. We have a very robust peer-visitation program with 17 visitors whose job is to listen and answer questions. Many people say they turned the corner after they had their first peer visit. I’ve worked with the phantom pain from the beginning. It takes time, and no magic bullet will take it away. The last-ditch effort would be spinal cord surgery. I really hope to talk to Dr. Ramachandran at some point, but nothing has been set up. We should invite him to come.”
The last person I talked to, under Sonja’s care, was Peter Harsch, 36, a civil prosthetist, blond, fast-talking, and with Hollywood good looks and charm. He showed me the equipment they used in preparing a prosthesis, most of it computerized. A cast is taken and the residual limb scanned and modified on a computer. Then the image is sent over to a carving machine, which produces a copy of the limb. Then heated Duraplex is put around the socket of the copy to make a mold ensuring that the eventual prosthesis will be a perfect fit.
As we moved from room to room, we passed amputees, both men and women, working on treadmills or being fitted. Everyone in contact with the amputees seemed tremendously upbeat, as if the missing limb were just a minor inconvenience, but it wasn’t as superficial as that may seem, because the staff obviously cared deeply about their patients and were doing what they could to make their lives better.
Harsch was particularly enthusiastic about the new technology developed in the past few years. “You’re getting a very smart monkey in the knee,” he told me. “You have four sensors recognizing the ground terrain, evaluating data at 1500 times per second, and motor systems powering the knee, foot, and ankle.” He also spoke about the i-Limb Hand, developed by U.K.-based Touch Bionics, which has five individually powered digits and looks and acts like a real human hand. The hand, according to the company’s website, touchbionics.com, “utilizes the electrical signals generated by the muscles in the remaining portion of the patient’s limb” to hold a coffee cup, slip a key in a lock, offer a business card, and a wide variety of other movements impossible in the past.
“We can reduce the phantom pain with the use of a good prosthesis,” Harsch said. “It really helps to desensitize those nerves. What’s important is which doctors are paying attention to the nerves. So orthopedic surgery is far more effective than vascular surgery. Vascular surgery might try to save the limb, but orthopedic surgery tries to prepare for the prosthesis. But with these guys in here, what they want to do, we try to do. We create a positive vibe. Some people will ask if this sort of work isn’t depressing, but I find it an incredible experience.”
I gathered most of the material for this article at the very end of 2007. Unknown to me at the time was an article on mirror therapy in the November 22 issue of the New England Journal of Medicine, written by a team of doctors and researchers at Walter Reed Army Medical Center. The team used 22 lower-limb amputees separated into three groups. All suffered from phantom pain. Indeed, the article said that phantom pain occurred in more than 90 percent of limb amputees. In a daily 15-minute therapy session, one group without mirrors closed their eyes and imagined moving the amputated limb. A second group used the mirror, but the mirror was covered so they couldn’t see it. In the third group, the patients could see “the reflected image of their intact foot in the mirror.”
After four weeks, two patients in the mental-visualization group reported less pain and four reported more pain. In the covered-mirror group, one patient reported less pain and three said they had more pain. In the mirror group, every single patient reported substantial improvement. Then nine patients from the first two groups were given four weeks of mirror therapy. At the end of that time, eight of those nine also experienced a substantial decrease in pain. Those in the first mirror-therapy group received another four weeks of treatment, and all continued to improve. Because of these results, Navy Cmdr. Jack Tsao, a neurologist at Walter Reed, who was one of the authors of the article, now offers mirror therapy routinely. It is extremely cheap and requires no special training. Indeed, he gives the few instructions to anyone interested by phone or email. He doesn’t know how it works except that the mirror seems to trick the brain into thinking that the missing limb still exists.
One wonders what would have happened if Tsao hadn’t recalled reading an article by Ramachandran while he was still in graduate school. And one wonders how mirror therapy might have helped the two million amputees in this country, many of whom still suffer from bouts of phantom pain. Use of mirror therapy has shown that the sooner it is administered, the more effective it is, although gains have been made no matter how old the amputation. And, again, I am amazed by how long it has taken for this treatment to be put into practice. A lot of pain has been endured unnecessarily.
Then there is my friend Glenn. After writing the above, I went to Home Depot and bought an inexpensive mirror measuring 30 x 36 inches. A little later I brought Glenn over to my house. Following a certain amount of talk, I got him to put on a pair of shorts, remove his prosthesis, and sit on the floor with the mirror separating his two legs and with the damaged leg hidden. “Now wiggle your toes,” I said. “On both feet.”
Glenn looked at me as if I’d said something foolish, but then he wiggled his toes. The toes in the mirror also wiggled. It didn’t look like a reflection; it looked like two separate feet wiggling their toes.
After a moment, Glenn said, “It’s weird. I mean, my other foot is moving its toes. The missing toes. I can feel my toes moving.” All the skepticism was gone from his voice. For a minute or so he happily wiggled the three sets of toes — the real, the reflected, and the phantom. “Think of that,” he said. “How strange.” He moved the foot from side to side, raised it a little. It was as if his missing foot had been restored, and he leaned over to his left to see if the stump was still there. “How does this happen?”
I told him how the brain has a body image and his body image included two feet. The mirror had tricked the brain.
“That’s weird,” he repeated. “That’s really interesting.”
I let him keep the mirror. Of course, he hadn’t been feeling any pain at that particular moment, but now at least, when the pain comes back, he’ll be ready.
Comments