 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
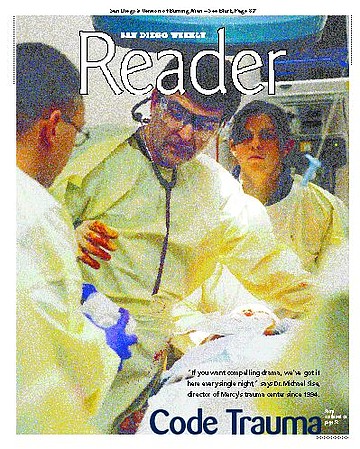
“If you want compelling drama, we’ve got it here every single night,” says Dr. Michael Sise, director of Mercy’s trauma center since 1994.
Sise is a walking encyclopedia of trauma medicine. A New York native, Sise, 50, resembles actor Chazz Palminteri in looks and manner. He stares at you with penetrating intensity, and nothing seems to ruffle him. “I started working here in ’87 part-time and full-time in ’92. Before that I was the chief of vascular surgery at the Naval Hospital. If it’s tough to be in health care, being in one of the highest-performing services of health care makes that toughness especially compelling.” An experienced trauma surgeon, Sise was chief surgeon aboard the USS Guam and USS Iwo Jima during the Persian Gulf War. At Mercy, he works 24-hour shifts with a trauma team that is on call and ready for whatever comes through the door.
Sise explains the distinctions between emergency and trauma medicine. “The emergency department and the trauma center obviously have to work closely together, and the emergency department is an integral part of providing trauma care. But the way it works is, you’re identified as a trauma patient at the scene, either because of the severity of your injury or because of certain criteria. A trauma is not just an injury, but the possibility of an injury or an injury that happens to someone with a pre-existing condition that could make that small injury worse. And ‘injury’ by itself is not enough to qualify as a trauma. A trauma is any major injury or risk of injury that requires immediate diagnostic workup and prompt treatment by qualified professionals.
“For instance, if you’re in an automobile accident where someone is killed, everybody in the car is made a trauma patient because of the likelihood of severe injuries — if one person was killed, there was probably enough force that you were severely injured, even though you may seem stable. If you fall 14 feet or more, if you are involved in a high-speed motor-vehicle accident unrestrained, if you have any number of injuries, the paramedics at the scene will communicate with the base station — and there are a number of base stations around the community based out of hospitals. The base station is where a specially trained doctor and nurse from the emergency department are available to communicate with the paramedics as to whether it’s a medical emergency or a trauma emergency or pediatric or obstetric emergency. They communicate back and forth and they decide, the paramedics and the nurse — the mobile intensive care nurse — whether or not you meet trauma-center criteria.
“So if you’re shot through the chest at the doorstep of Grossmont Hospital, you’ll still go to Sharp, because you’re a trauma patient and we know that at Sharp there is a fully trained surgeon, an operating room, an anesthesiologist, an O.R. nurse — all sorts of people immediately available that aren’t necessarily available at Grossmont on a reliable basis. Now, Grossmont’s a great hospital, but they’re not part of the trauma system, and we’ve proven time and again something we learned in Vietnam, where we flew people to the doctors — that to take the extra 10 to sometimes 20 minutes to fly somebody to the right place is much better for that patient than to take them to the closest facility if they don’t have those resources. So it’s not the geographic location but the resources that make the difference. Then, once you’re a trauma patient, bingo! It sets off the system.”
A string of preventable deaths led to the creation of San Diego’s trauma-care system. “It was organized in 1984. In the 1970s and early ’80s, we did not have a trauma system, so if you were injured, you were taken to the nearest hospital, regardless of its capabilities. There were a couple of very high profile cases where injured patients were taken to hospitals that were the nearest hospitals but weren’t capable of providing trauma care — and they died. It got to a point where in 1982 the county medical society and the Hospital Council, in conjunction with the Department of Emergency Medical Services, commissioned a study in the county by a group called the Amherst Group — a health-care consulting group — and they looked at all the patients who had died in ’82 from trauma and they found that 20 percent of them died a potentially or outright preventable death. So one in five patients who died after trauma could have been saved if they’d had access to an organized trauma system. After that report was received in 1983, we organized a trauma system that came on-line by 1984.
“The way the trauma system works is, the county is the agency that designates whether or not a hospital is a trauma center and can receive trauma patients. There’s a code of law called Title 22, which is part of the California Health and Safety Code that tells you what you have to have. And the American College of Surgeons has published this document that we have to live by. The reason I’m telling you this is that it’s almost schizophrenic. If you are admitted to this hospital or any of the trauma centers, you are tracked and everything that happens to you is timed, recorded, and audited in a way where it’s audited nowhere else in health care — throughout the United States or even the world. Not only are we required to do this by the county, but also by the American College of Surgeons to meet the national standard of what it is to be a trauma center.
“Anyway, in 1984, six trauma centers came on-line: Mercy, ucsd, at the time Grossmont, Scripps La Jolla, and Sharp Memorial, and Children’s for pediatric trauma. Within a year, Grossmont dropped out and Palomar came on-line. Since 1985, those six trauma hospitals have stayed in the system, which is remarkable. At the same time, in L.A. County, in a 40-hospital trauma system, only 13 hospitals are left. This has left a tremendous burden on the other hospitals, particularly the public hospitals.”
Sise shows me a map of the county. “The way it works in this county and what makes it so sustainable is that we have absolutely rock-hard, drawn catchment areas. For instance, if you’re coming up 805 northbound and get injured, you come to Mercy. Southbound, you go to ucsd, unless that trauma center is on bypass; then you’re routed to another trauma center. So it’s kind of the ultimate ‘managed competition.’ We all work together. We don’t compete for each other’s patients — we back each other up and support each other. Many of us have trauma surgeons who take calls at different trauma hospitals, so we ‘cross-pollinate,’ so we all know each other, and every month we meet and review the course of every patient that’s admitted to the trauma system. So I have to report not only how fast you got your x-rays, how fast you got to the operating room, but whether or not you had a complication.
“The trauma centers belong to competing health-care systems, yet we’re all very collaborative and we work together, so there’s a real difference now. The year after our trauma system came on-line, we repeated the study of the Amherst Group, and the preventable death rate fell to 1 percent, where it has stayed since.
“One of our faults as a trauma system is that we haven’t done a whole lot to promote awareness in the community so that we don’t get taken for granted, because in San Diego County we don’t have a public hospital system. We have a safety net that’s made up of private- and public-sector hospitals. Fortunately, we’ve been able to be very efficient in the way we run our trauma centers and have them more or less break even, which has kept us sustainable as opposed to L.A., where private hospitals are bailing out. Either it’s not part of their mission — they don’t feel the need to do it — or they don’t have the will to do it. It takes a fair amount of work. You have to provide for the call panels, the nurses, the surgeons, always having an operating room available, a cat scanner, and all the other stuff. It’s like running a marathon — you don’t just decide you’re going to do it one day. It’s day after day after day. You have to be prepared.”
It is also expensive. “It’s hard to tell you exactly how much, because those same nurses who are caring for the trauma patient are the same nurses who care for the ruptured abdominal aortic aneurysm or the heart attack or also have duties in the operating room. I can’t put a dollar value on it, but I would estimate it’s a couple of million bucks [a year].”
Surprisingly, Sise focuses his role of trauma medicine to prevention. “If you draw a line across the county — maybe at 8, maybe at 52 — south of that line we have a lot of folks for whom there is no voice. Many of those folks come from extremely challenging environments. A high incidence of trauma patients are victims of substance abuse or domestic violence. Our challenge comes from taking people who live high-risk lives — participate in high-risk behaviors and get hurt — trying to get them through their acute illness and trying to get them to some environment with resources to help them somehow get out of the trouble they were in in the first place which got them hurt.
“The fact that we’ve got the preventable death rate down to less than 1 percent means that it’s gotten about as good as it can get in many ways. It’s a matter of maintaining. Our biggest obstacle is the overall pressure on health care to do more with less. The nursing shortage is a tremendous obstacle. Not only are fewer men and women going into nursing, but many of our nurses are getting older, retiring, and moving on.
“It’s not just the everyday grind of measuring up, but also in doing a good job for the people we treat. There’s some tough, tough stories. I met a woman on Friday night — some person came to her home, shot her husband dead, and shot her through the liver, and she’s got three young kids. She’s going to recover, but she’s going home a widow with three young kids. Or take someone who’s desperately crazy and keeps trying to commit suicide, you can’t just ‘treat ’em and street ’em.’ You’ve got to somehow reach into the community. And beyond that, how do you reach into the community to stop injuries from happening? If we’re down to less than 1 percent preventable death rate, that means we’re not going to get a lot better. Unless we come up with some sort of a Star Trek system of placing you in suspended animation, you’re either going to live or die based on the severity of that injury. The ‘heavy lifting’ of trauma care is getting out into the community and preventing injury or returning the injured patient to a better environment than the one they left. That’s hard.”
The role of a trauma surgeon is highly specialized yet flexible. “A trauma surgeon is not an emergency medicine position. A trauma surgeon is a fully trained surgeon with the expertise and background and commitment and the ongoing education and all the things that we have to do in terms of ongoing participation that makes you a trauma surgeon. A general surgeon may do trauma, but not every general surgeon is a trauma surgeon.
“The trauma team is composed of the team leader who is a trauma surgeon, a nurse who is a trauma-care specialist — a lot of the people in the emergency department respond and become part of the trauma team: nurses, O.R. nurses, x-ray technicians, respiratory therapists, cat scan/radiology folks who support us. We’re actually the training program for the Navy residents, so we are the trauma training center for the Navy.
“We also have what we call the trauma ‘special teams’ — the folks we bring in — the neurosurgeons, orthopedic surgeons, anesthesiologists, plastic surgeons. The specialized surgeons who come in and help us. Doctors tend to work alone. Surgeons, especially, usually operate alone [without other surgeons present]. One of the real pleasures of being on the trauma team is that you’re together with a team. It makes you better individually and vastly improves the care for the patients.”
There are specific times when the number of traumas increase. “You gotta like working at night. Trauma is a nocturnal disease and every night’s a gut check. Halloween is traditionally bad. It’s incredible how many adults and young kids go out and drink and drive. If you look at the week, most trauma occurs between four in the afternoon and four in the morning. Friday and Saturday nights are the two busiest nights. Our busiest night here was on a Thursday night — we saw 17 patients in one day — and that’s a lot of patients. It turns out that clear, cool nights, particularly clear, cool weekend nights, especially if they are paydays or full moons — full moons seem to do it! People laugh, but it’s true! People get more active. On paydays people are partyin’, particularly if you have a combined military and civilian payday” — Sise pauses and grins — “on a Friday night, clear and cool, it can be particularly treacherous. On weekends, we talk about the ‘Domestic Violence Hour.’ That’s between two and four in the morning, after the bars close. If someone has a drinking problem, they go home and will frequently get in a fight with their spouse. Somebody will get beat up, shot, or stabbed.”
One of Sise’s trauma patients still haunts his memory. “A young guy was depressed because his girlfriend dumped him. He was a good kid from a good family, but he got a little drunk, got ahold of a shotgun, and tried to kill himself.” Sise points upward through his chin. “Instead of killing himself, he blew his face off. It’s sad. If he hadn’t had access to a firearm, the next morning he would have been dumped, depressed, and hung over instead of facing lifelong reconstructive surgery. He lost one eye and most of his upper and lower jaw.”
Our interview is cut short as Sise’s voice pager announces “Code Trauma.” “We’ve got a code trauma — come on!” We walk down several corridors until we face doors open to a parking lot filled with ambulances. The paramedics wheel in a Hispanic man in a neck brace wearing only shorts. There is blood all over his left arm. He is fully conscious. The team quietly converges on him as the paramedics calmly provide relevant information. They ask Sise if he needs an interpreter, and he declines before addressing the patient in Spanish. He is moved onto an operating table as they examine, test, and monitor him. An x-ray machine is wheeled into the room. All of this takes place in less than two minutes. While diligently applied to their tasks, no one on the team seems panicked or nervous.
I find out later that the man was working on a roof that collapsed under him. He fell 12 feet onto a solid concrete walkway, where he landed on his back. His left arm is apparently fractured from hitting a metal rail while falling. He was brought to Mercy from the College Area.
Ten minutes later, Sise emerges from the trauma room, apparently satisfied that the man is stable.
He urges readers to consider his parting words: “Look at it this way: A third of us get cancer at some time in our lives. Half of us get severe heart disease, and half of us die from heart disease or stroke. But none of us are predestined to die from trauma. It’s totally, 100 percent preventable. If you have a strong family history of diabetes, you’re probably going to get diabetes. You can’t prevent it. You can manipulate it and minimize its impact. But there’s no reason why you, your wife, or your kids have to get shot, stabbed, or wounded.”

“If you want compelling drama, we’ve got it here every single night,” says Dr. Michael Sise, director of Mercy’s trauma center since 1994.
Sise is a walking encyclopedia of trauma medicine. A New York native, Sise, 50, resembles actor Chazz Palminteri in looks and manner. He stares at you with penetrating intensity, and nothing seems to ruffle him. “I started working here in ’87 part-time and full-time in ’92. Before that I was the chief of vascular surgery at the Naval Hospital. If it’s tough to be in health care, being in one of the highest-performing services of health care makes that toughness especially compelling.” An experienced trauma surgeon, Sise was chief surgeon aboard the USS Guam and USS Iwo Jima during the Persian Gulf War. At Mercy, he works 24-hour shifts with a trauma team that is on call and ready for whatever comes through the door.
Sise explains the distinctions between emergency and trauma medicine. “The emergency department and the trauma center obviously have to work closely together, and the emergency department is an integral part of providing trauma care. But the way it works is, you’re identified as a trauma patient at the scene, either because of the severity of your injury or because of certain criteria. A trauma is not just an injury, but the possibility of an injury or an injury that happens to someone with a pre-existing condition that could make that small injury worse. And ‘injury’ by itself is not enough to qualify as a trauma. A trauma is any major injury or risk of injury that requires immediate diagnostic workup and prompt treatment by qualified professionals.
“For instance, if you’re in an automobile accident where someone is killed, everybody in the car is made a trauma patient because of the likelihood of severe injuries — if one person was killed, there was probably enough force that you were severely injured, even though you may seem stable. If you fall 14 feet or more, if you are involved in a high-speed motor-vehicle accident unrestrained, if you have any number of injuries, the paramedics at the scene will communicate with the base station — and there are a number of base stations around the community based out of hospitals. The base station is where a specially trained doctor and nurse from the emergency department are available to communicate with the paramedics as to whether it’s a medical emergency or a trauma emergency or pediatric or obstetric emergency. They communicate back and forth and they decide, the paramedics and the nurse — the mobile intensive care nurse — whether or not you meet trauma-center criteria.
“So if you’re shot through the chest at the doorstep of Grossmont Hospital, you’ll still go to Sharp, because you’re a trauma patient and we know that at Sharp there is a fully trained surgeon, an operating room, an anesthesiologist, an O.R. nurse — all sorts of people immediately available that aren’t necessarily available at Grossmont on a reliable basis. Now, Grossmont’s a great hospital, but they’re not part of the trauma system, and we’ve proven time and again something we learned in Vietnam, where we flew people to the doctors — that to take the extra 10 to sometimes 20 minutes to fly somebody to the right place is much better for that patient than to take them to the closest facility if they don’t have those resources. So it’s not the geographic location but the resources that make the difference. Then, once you’re a trauma patient, bingo! It sets off the system.”
A string of preventable deaths led to the creation of San Diego’s trauma-care system. “It was organized in 1984. In the 1970s and early ’80s, we did not have a trauma system, so if you were injured, you were taken to the nearest hospital, regardless of its capabilities. There were a couple of very high profile cases where injured patients were taken to hospitals that were the nearest hospitals but weren’t capable of providing trauma care — and they died. It got to a point where in 1982 the county medical society and the Hospital Council, in conjunction with the Department of Emergency Medical Services, commissioned a study in the county by a group called the Amherst Group — a health-care consulting group — and they looked at all the patients who had died in ’82 from trauma and they found that 20 percent of them died a potentially or outright preventable death. So one in five patients who died after trauma could have been saved if they’d had access to an organized trauma system. After that report was received in 1983, we organized a trauma system that came on-line by 1984.
“The way the trauma system works is, the county is the agency that designates whether or not a hospital is a trauma center and can receive trauma patients. There’s a code of law called Title 22, which is part of the California Health and Safety Code that tells you what you have to have. And the American College of Surgeons has published this document that we have to live by. The reason I’m telling you this is that it’s almost schizophrenic. If you are admitted to this hospital or any of the trauma centers, you are tracked and everything that happens to you is timed, recorded, and audited in a way where it’s audited nowhere else in health care — throughout the United States or even the world. Not only are we required to do this by the county, but also by the American College of Surgeons to meet the national standard of what it is to be a trauma center.
“Anyway, in 1984, six trauma centers came on-line: Mercy, ucsd, at the time Grossmont, Scripps La Jolla, and Sharp Memorial, and Children’s for pediatric trauma. Within a year, Grossmont dropped out and Palomar came on-line. Since 1985, those six trauma hospitals have stayed in the system, which is remarkable. At the same time, in L.A. County, in a 40-hospital trauma system, only 13 hospitals are left. This has left a tremendous burden on the other hospitals, particularly the public hospitals.”
Sise shows me a map of the county. “The way it works in this county and what makes it so sustainable is that we have absolutely rock-hard, drawn catchment areas. For instance, if you’re coming up 805 northbound and get injured, you come to Mercy. Southbound, you go to ucsd, unless that trauma center is on bypass; then you’re routed to another trauma center. So it’s kind of the ultimate ‘managed competition.’ We all work together. We don’t compete for each other’s patients — we back each other up and support each other. Many of us have trauma surgeons who take calls at different trauma hospitals, so we ‘cross-pollinate,’ so we all know each other, and every month we meet and review the course of every patient that’s admitted to the trauma system. So I have to report not only how fast you got your x-rays, how fast you got to the operating room, but whether or not you had a complication.
“The trauma centers belong to competing health-care systems, yet we’re all very collaborative and we work together, so there’s a real difference now. The year after our trauma system came on-line, we repeated the study of the Amherst Group, and the preventable death rate fell to 1 percent, where it has stayed since.
“One of our faults as a trauma system is that we haven’t done a whole lot to promote awareness in the community so that we don’t get taken for granted, because in San Diego County we don’t have a public hospital system. We have a safety net that’s made up of private- and public-sector hospitals. Fortunately, we’ve been able to be very efficient in the way we run our trauma centers and have them more or less break even, which has kept us sustainable as opposed to L.A., where private hospitals are bailing out. Either it’s not part of their mission — they don’t feel the need to do it — or they don’t have the will to do it. It takes a fair amount of work. You have to provide for the call panels, the nurses, the surgeons, always having an operating room available, a cat scanner, and all the other stuff. It’s like running a marathon — you don’t just decide you’re going to do it one day. It’s day after day after day. You have to be prepared.”
It is also expensive. “It’s hard to tell you exactly how much, because those same nurses who are caring for the trauma patient are the same nurses who care for the ruptured abdominal aortic aneurysm or the heart attack or also have duties in the operating room. I can’t put a dollar value on it, but I would estimate it’s a couple of million bucks [a year].”
Surprisingly, Sise focuses his role of trauma medicine to prevention. “If you draw a line across the county — maybe at 8, maybe at 52 — south of that line we have a lot of folks for whom there is no voice. Many of those folks come from extremely challenging environments. A high incidence of trauma patients are victims of substance abuse or domestic violence. Our challenge comes from taking people who live high-risk lives — participate in high-risk behaviors and get hurt — trying to get them through their acute illness and trying to get them to some environment with resources to help them somehow get out of the trouble they were in in the first place which got them hurt.
“The fact that we’ve got the preventable death rate down to less than 1 percent means that it’s gotten about as good as it can get in many ways. It’s a matter of maintaining. Our biggest obstacle is the overall pressure on health care to do more with less. The nursing shortage is a tremendous obstacle. Not only are fewer men and women going into nursing, but many of our nurses are getting older, retiring, and moving on.
“It’s not just the everyday grind of measuring up, but also in doing a good job for the people we treat. There’s some tough, tough stories. I met a woman on Friday night — some person came to her home, shot her husband dead, and shot her through the liver, and she’s got three young kids. She’s going to recover, but she’s going home a widow with three young kids. Or take someone who’s desperately crazy and keeps trying to commit suicide, you can’t just ‘treat ’em and street ’em.’ You’ve got to somehow reach into the community. And beyond that, how do you reach into the community to stop injuries from happening? If we’re down to less than 1 percent preventable death rate, that means we’re not going to get a lot better. Unless we come up with some sort of a Star Trek system of placing you in suspended animation, you’re either going to live or die based on the severity of that injury. The ‘heavy lifting’ of trauma care is getting out into the community and preventing injury or returning the injured patient to a better environment than the one they left. That’s hard.”
The role of a trauma surgeon is highly specialized yet flexible. “A trauma surgeon is not an emergency medicine position. A trauma surgeon is a fully trained surgeon with the expertise and background and commitment and the ongoing education and all the things that we have to do in terms of ongoing participation that makes you a trauma surgeon. A general surgeon may do trauma, but not every general surgeon is a trauma surgeon.
“The trauma team is composed of the team leader who is a trauma surgeon, a nurse who is a trauma-care specialist — a lot of the people in the emergency department respond and become part of the trauma team: nurses, O.R. nurses, x-ray technicians, respiratory therapists, cat scan/radiology folks who support us. We’re actually the training program for the Navy residents, so we are the trauma training center for the Navy.
“We also have what we call the trauma ‘special teams’ — the folks we bring in — the neurosurgeons, orthopedic surgeons, anesthesiologists, plastic surgeons. The specialized surgeons who come in and help us. Doctors tend to work alone. Surgeons, especially, usually operate alone [without other surgeons present]. One of the real pleasures of being on the trauma team is that you’re together with a team. It makes you better individually and vastly improves the care for the patients.”
There are specific times when the number of traumas increase. “You gotta like working at night. Trauma is a nocturnal disease and every night’s a gut check. Halloween is traditionally bad. It’s incredible how many adults and young kids go out and drink and drive. If you look at the week, most trauma occurs between four in the afternoon and four in the morning. Friday and Saturday nights are the two busiest nights. Our busiest night here was on a Thursday night — we saw 17 patients in one day — and that’s a lot of patients. It turns out that clear, cool nights, particularly clear, cool weekend nights, especially if they are paydays or full moons — full moons seem to do it! People laugh, but it’s true! People get more active. On paydays people are partyin’, particularly if you have a combined military and civilian payday” — Sise pauses and grins — “on a Friday night, clear and cool, it can be particularly treacherous. On weekends, we talk about the ‘Domestic Violence Hour.’ That’s between two and four in the morning, after the bars close. If someone has a drinking problem, they go home and will frequently get in a fight with their spouse. Somebody will get beat up, shot, or stabbed.”
One of Sise’s trauma patients still haunts his memory. “A young guy was depressed because his girlfriend dumped him. He was a good kid from a good family, but he got a little drunk, got ahold of a shotgun, and tried to kill himself.” Sise points upward through his chin. “Instead of killing himself, he blew his face off. It’s sad. If he hadn’t had access to a firearm, the next morning he would have been dumped, depressed, and hung over instead of facing lifelong reconstructive surgery. He lost one eye and most of his upper and lower jaw.”
Our interview is cut short as Sise’s voice pager announces “Code Trauma.” “We’ve got a code trauma — come on!” We walk down several corridors until we face doors open to a parking lot filled with ambulances. The paramedics wheel in a Hispanic man in a neck brace wearing only shorts. There is blood all over his left arm. He is fully conscious. The team quietly converges on him as the paramedics calmly provide relevant information. They ask Sise if he needs an interpreter, and he declines before addressing the patient in Spanish. He is moved onto an operating table as they examine, test, and monitor him. An x-ray machine is wheeled into the room. All of this takes place in less than two minutes. While diligently applied to their tasks, no one on the team seems panicked or nervous.
I find out later that the man was working on a roof that collapsed under him. He fell 12 feet onto a solid concrete walkway, where he landed on his back. His left arm is apparently fractured from hitting a metal rail while falling. He was brought to Mercy from the College Area.
Ten minutes later, Sise emerges from the trauma room, apparently satisfied that the man is stable.
He urges readers to consider his parting words: “Look at it this way: A third of us get cancer at some time in our lives. Half of us get severe heart disease, and half of us die from heart disease or stroke. But none of us are predestined to die from trauma. It’s totally, 100 percent preventable. If you have a strong family history of diabetes, you’re probably going to get diabetes. You can’t prevent it. You can manipulate it and minimize its impact. But there’s no reason why you, your wife, or your kids have to get shot, stabbed, or wounded.”
Comments