 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

Like many newly married couples, Cristen and Jeffry Hays wanted to get pregnant soon after their wedding in 1992 but felt it best to wait.
They used birth control until Jeffry finished three years of chiropractic school, passed his preceptorship, and established a practice in San Diego. Then, in their mid-30s, with “it’s now or never” nagging them, they dropped their protective shields and went at it, a pleasure as often as it was a duty.
For a year, nothing happened. Something was wrong, and the Bakersfield natives suspected the problem was inside Cristen. An insulin-dependent diabetic since 12, Cristen wears an insulin pump, monitors her intake by pricking her finger and testing her blood-sugar level ten times a day, and lives at times emotionally weakened by the high maintenance her illness requires. Tests suggested that either the diabetes or scar tissue from the disease was blocking her fallopian tubes. She was ovulating regularly, but the incoming sperm couldn’t find an egg. They considered laparoscopy, a “roto-rooter,” Cristen calls it, to open up the tubes. But the operation guaranteed nothing, except another invasive procedure.
Diabetics do have healthy babies every day, Cristen tells me on a warm evening in January when she and her husband are lounging at the dining room table in drawstring shorts and cotton T-shirts at their Scripps Ranch home. Cristen is 37, athletic and fit, able to work, but weary of her daily regimen. Jeffry, a year older and a former personal trainer, possesses (literally) a hands-on grasp of anatomy as well as empathy for his wife’s condition. “Yes, [pregnancy] is doable,” he says. “But Cristen had had complications with her eyes, some stages of kidney dysfunction. Throw a pregnancy in there, throw some hormones in there, throw all that together and try to manage your blood sugar. If the blood sugars get out of control, it can wreak havoc. Some higher power was saying that this was not meant to be.” So they gave up on getting pregnant and turned to the higher power of science.

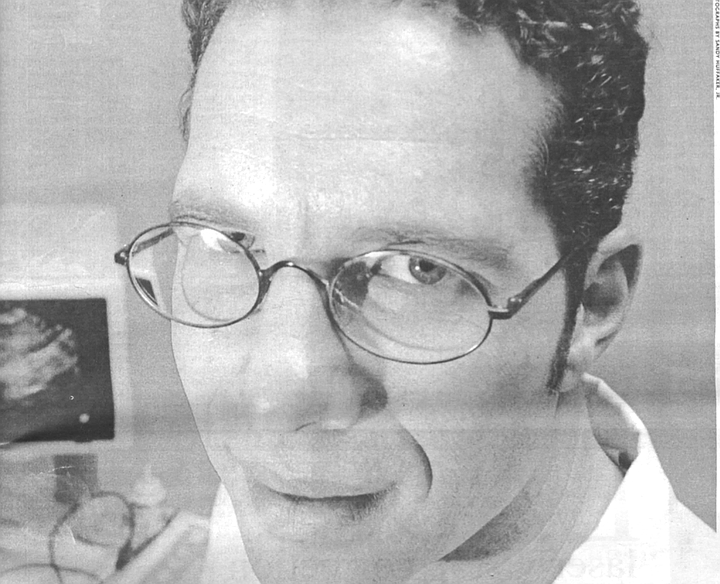
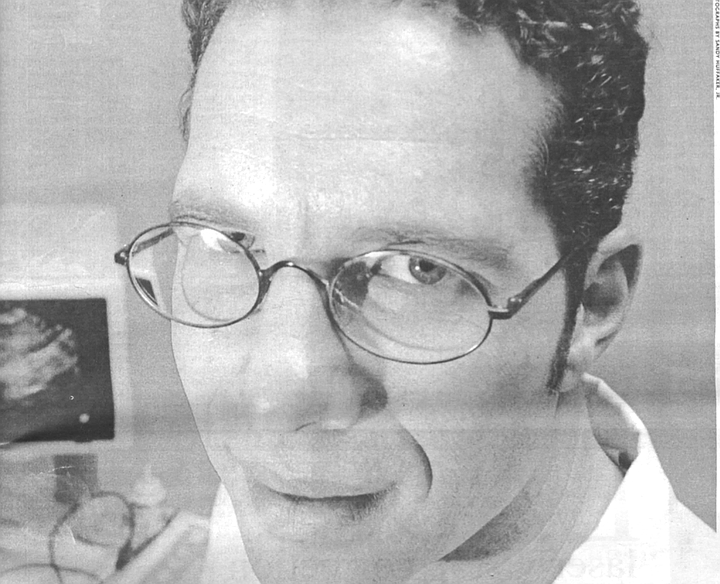
In vitro fertilization, it’s called. The now-22-year-old technique whereby conception can occur outside the body is routinely performed at seven San Diego fertility clinics. Cristen and Jeffry met Dr. David Smotrich at his Smotrich Center for Reproductive Enhancement. A soft-spoken, impartial man, as much scholar as physician, Smotrich was trained at Tel Aviv University. He told me recently, “In Israel, there’s a push for people to get pregnant.” As a “disease,” infertility is covered under Israel’s socialized medicine system, while in the United States the procedure is still elective.
In any event, Smotrich didn’t need to present the Hayses with the idea of surrogacy, that is, a carrier for the couple’s fetus who gives birth to the child and gives the child to the parents. The Hayses had already stumbled on the procedure through a friend whose sister had been a surrogate. Suddenly an idea lit up in Cristen; she thought of her older sister Candace, who had three children and who, according to Cristen, gets “pregnant so easily.” Candace wasn’t sure. She hemmed and hawed for months. Antsy, Jeffry called her one afternoon and said, “I appreciate that this is a big decision, but we have to know.” After a half-year of reading, classes, and reflection, Candace agreed.
In vitro with a surrogate requires pit-stop coordination. Candace took drugs to ready her uterus to receive the embryo; Cristen was put on Pergonal to stimulate her egg production; Jeffry kept his calendar open: He would have to arrive at the clinic to supply the sperm on the same day as implantation. Which, good trooper, that’s just what he did — running a stop sign or two on his way to the clinic bathroom when the great day finally arrived.
On Pergonal, Cristen had created 14 eggs, and Smotrich, once he’d removed them from her ovary, fertilized 10 of them. (The odds of fertilization are pretty good, what with 40,000 to 50,000 fresh motile sperm after one egg on the bottom of a petri dish.) He watched the eggs closely, “grading them subjectively,” as he says, on their number of divisions, symmetry, and clarity. He determined that 6 of the 10 were viable. Smotrich and the Hayses decided then to implant 3 in Candace and freeze the other 3 for a (possible) later cycle. Raising high the roof beams, Jeffry and Cristen’s Christmas card showed a picture of an embryo, a one-day-old, six-cell floating clover leaf in its preimplantation petri-dish exile.
Fertilization begins when the pronucleus of the male gamete disperses its material into the pronucleus of the female gamete. With in vitro, it may be necessary to surgically inject a single sperm through the egg’s membrane with a needle. Consummation occurs once 23 chromosomes of each male and female gamete are combined into a single cell, the zygote. The zygote then begins cleavage, dividing many times over the next four days. At day five, the zygote forms a blastocyst, a hollow membrane of primitive cells, some external, but more colonizing internally in a tight clump. Seen under a microscope, the round blastocyst, about as thick as a human hair, or 0.008 inch, resembles an inverted wedding ring with the diamond on the inside of the circle. That diamond is the inner cell clump, elliptically formed and pulsating with switched-on genome joy. The hope is that the blastocyst will keep enlarging and, after seven and a half days, implant its sticky outer cell mass (eventually the placenta) onto and into the uterine wall. The cells forming on the inside of the blastocyst are called stem cells, that is, the undifferentiated master cells from which all other cells in our body stem.
(It is these cells and their medical possibilities that I have come to talk with the Hayses about, though I admit to being circuitous. Stem cells have been touted, just in the last two years, as the greatest medical miracle since antibiotics, because these cells, in their blastocyst stage, have unlimited potential for treating and curing almost all diseases as well as for growing organs from scratch. I hope to discover how Cristen and Jeffry feel about this potential, which, as they know, resides within the embryos they have created, and are keeping, in vitro.)
Back at the clinic, Dr. Smotrich placed three embryos in Candace. Jeffry and Cristen knew their chances were less than 50-50, but they were hopeful. Just one or, perhaps, all three will stick. High hopes, indeed, but the rule is otherwise. The best guesstimate is that only one of ten implanted embryos stays for the full term. We’ve all heard of the exhausted mother with as many as seven embryos implanted, resulting in a multiple birth after which telethons are organized and the neighborhood volunteers in shifts to change diapers. Couples and clinics want pregnancies. That can mean upping the ante with fertility drugs and the questionable practice of putting in a dozen embryos to enhance the odds (in England the law limits the number to four). But the “success rate” of in vitro remains dicey: Only 40 percent of couples who do three cycles or more (each cycle is one implantation of embryos) will get a baby.
Dicey, indeed, for Cristen and Jeffry and Candace, now an even closer triumvirate. But, sadly, none of the three implanted; Candace’s body absorbed them. After consultation, the group decided to unthaw the other three embryos and try again. A month later, that too was a bust. It was “all downhill on the emotional roller coaster,” Cristen recalls. Either they’d start once more from scratch, meaning another $10,000 cycle and the coordinated labor of the female tag team, or quit. Cristen, a fighter, says, “I wasn’t ready to give up,” even after the second failure. Jeffry adds, “We felt the odds increase every time because the doctor learns a little bit more about what he can change to make our chances greater.”
On the third cycle, they created five embryos and Smotrich placed four in Candace. Jeffry calls it “getting more aggressive,” while Cristen acknowledges some desperation. Candace agreed that if all four, or three or two, stuck, she would carry the lot to term. The lone leftover embryo they froze. Though the Hayses and Candace knew about “selective reduction,” whereby they could reduce the number inside Candace if there were complications, in principle the three decided against it. Doing so remained hypothetical: One of the four clung to Candace’s uterus and buried itself in the lining. The embryo-cum-fetus had few problems as it grew to term. In March 1999, Jayden Marie Hays was born, pudgy and healthy, a saucer-eyed charmer who by the time I meet her at age nine months cadges me to pick her up and hold her just so she can push my tape recorder off the table.
Though Cristen and Jeffry and Candace came to a perfect end with Jayden’s birth, which is also the perfect beginning of this little girl’s life, there is another “being” or “life” left to consider. That other frozen, and as yet unused, embryo. And the Hayses have considered it.
Options for the future of frozen embryos are several. Smotrich described four: Use them again for another cycle; not use them again and instruct the clinic to thaw and discard them (couples can request a memorial service); donate them to an infertile couple; donate them to research. “Most couples recognize how difficult it is to create embryos,” he says, “so it’s unusual for them to want to discard them.” Most keep them frozen; the storage fee runs around $150 a year. (The oldest known freezer-to-birth embryo is one that was held for seven years.) Their numbers are also reduced because, according to Smotrich, there’s only a “67 percent successful thaw-rate,” which means one-third of them die.
The Hayses have decided to leave their remaining embryo frozen, for the time being. If they change their minds, they will donate it to medical research.
I ask them how they regard its “moral status.” Quickly, it seems, the joyful ending of Jayden’s conception and birth is left in the dust.
“I don’t know,” Jeffry says. “I guess I see it as — even though it’s frozen, it’s alive.”
“Can you say it’s alive?” Cristen counters. “Because it doesn’t have a heartbeat.”
Jeffry stares at me, his inquisitor. “So the question you’re raising, damn you” — he and I laugh nervously — “who are we to take this potential life’s being and donate it to science when it could live?”
“We’ll use it,” Cristen says with certainty, confiding later that she has a new surrogate picked out, her younger sister. Candace, at 40, has said no thanks to another mission.
“I’d like to think we’d use it,” Jeffry adds. “But if we don’t, our choice was not to donate to another couple to start a family but to donate to science so something could be learned from [the embryo].” His voice is a bit ethereal; Cristen is quiet. There’s a sense — and I can’t quite put my finger on it — not that the Hayses have disregarded the “rights” of this being but that thinking about the “moral status” of a five-day-old blastocyst/embryo yields no firm answer as in, “Oh, yes, it is a full legal and moral person,” or “Oh, no, we have no attachment to it.” Thinking this through for anyone, let alone the parents, while the embryo sits in the cryogenic freezer at minus 196 degrees Celsius in a liquid-nitrogen crystallized state, yields far more questions than answers. (There’s a lot of thinking-through going on these days in America, with 150,000 to 200,000 embryos in their technological purgatory. Waiting and thinking, I coulda been a contender.)
“In essence,” Jeffry says, seemingly not wanting to admit it, “we’re putting this out to pasture, we’re condemning this embryo to death.”
“It’s like organ donation,” Cristen says.
“No, it’s not,” he says. “An organ isn’t a life.”
She agrees, and adds, “Then we’re going to use it.” Jeffry laughs and reminds her that this embryo is “not a very viable one, and so I guess I’m justifying in my own mind that if we don’t use it, then we’ll donate it to science.” But deciding whether to keep it, he admits, is also a way to delay a decision about its status. “I didn’t sit down and think, ‘What if I donate this to science? Then that means I’m not allowing this embryo a chance to live?’ ” And if it’s a life — I believe he understands this but didn’t express it this way — then it’s troubling, because donating the embryo to research will mean terminating its life. “And I’m against abortion,” he says, renewing his moral quandary more than he may want to.
Then, as if to rescue Dad from the Big Muddy, Jayden is pulling herself up the rungs of the chair he’s sitting in, reaching hands up to be hoisted, to feel alive in his lap where there is no uncertainty about her.
It’s not clear that there’s a good place to end our talk, so I say it’s late and I must be getting home. Before leaving I recall that before the Hayses told me the story of Jayden’s birth, I’d asked Cristen if diabetes is hereditary. Yes, she responded. Her father and brother both have it; in fact, complications have meant eye surgery for Cristen and her father.
I looked at Jayden, chewing on a biscuit in the high chair. Does she have diabetes? I asked uncomfortably.
“We’re hoping she won’t,” said Cristen.
Driving home, I imagine Jayden one day not having a brother or sister from the lone embryo and, instead, that intended being donated to research. If Jeffry and Cristen do trade the gift of a sibling for a possible cure for a disease Jayden might inherit, I hope any of us can understand the moral dilemma they have faced.
About the time Jayden was lolling, midway through her gestation, in Candace’s uterus, James Thomson, a molecular biologist at the University of Wisconsin, was testifying to a subcommittee of the United States Senate. He was excited, in that self-possessed unexcited way scientists get, about his research using human embryonic stem cells, those cells that can only be gotten from a five-day-old blastocyst. Thomson had been one of the first U.S. scientists to remove stem cells from a human embryo. The embryo was donated by a couple, much like the Hayses, who had created more than they needed during in vitro treatment. Thomson had isolated the cells on a bed of mouse embryonic stem cells and, after eight months of growing over one trillion (that’s right, with a t), he was amazed at what his research team had accomplished, namely, maintaining a feedstock of these master cells that form the cellular paths for all human development.
Stem cells contain undifferentiated and unspecialized cellular potential and, if harvested in their youngest and purest stage, hold treatments and cures for nearly all types of disease. Harold Varmus, head of the National Institutes of Health, has said, “This research has the potential to revolutionize the practice of medicine.” Further indicative of its promise is the Patient’s Coalition for Urgent Research, which is advocating an increase in federally funded stem cell research: “No research in recent history has offered as much hope to the more than 128 million Americans suffering from debilitating and often fatal diseases.”
The list of possible cures using stem cell treatments is staggering: sickle cell anemia, Parkinson’s and other brain diseases, heart and cardiovascular diseases, certain leukemias and cancers, autoimmune diseases, osteoporosis, spinal-cord injuries, birth defects, and more. There is even a treatment proposed using stem cells to cure Cristen Hays’s disease, juvenile onset diabetes, from which one American dies every three minutes. In addition, work is proceeding with synthetic scaffolds and tissue-specific stem cells to grow cartilage, muscle, pancreas, kidney, liver, heart. Finally, genetic manipulation of stem cells may mean that many diseases will be nipped in the code and never begin.
Thomson’s experiment had to be done in a straitjacket, so to speak. The National Institutes of Health has banned the use of federal funds for any human embryonic research although the government does not forbid privately funded research. So Thomson got funding from the California-based Geron Corporation, a private biotechnology company, and built a lab only for his stem cell experiments. (Word was he bought everything new, including the electrical extension cords.) His comment at the time speaks volumes about government duplicity: “That a sensitive category of research is legal for people who are not publicly accountable but illegal for those who are accountable is just very strange.”
Thomson forged ahead, growing his bank of stem cells, then arresting their growth in the deep freeze. He testified at the senate hearing that such cells could not by themselves make an embryo. Thomson wanted the senators to hear why he feels stem cell research should require the ethical exploration and financial support of the National Institutes of Health. He said, “The current ban…for embryo research discourages the majority of the best U.S. researchers from advancing this promising area of medical research.” One month prior to his testimony, at the time of his discovery, he told the press that the mother of all cells contains “limitless” possibilities. “Our stem cells can give rise to potentially everything, and they never die.” By never dying, he meant that a stem cell’s nature is to self-renew and to differentiate: Most often it divides into two cells, one a duplicate, and another that will differentiate via further growth and division into a particular tissue. By duplicating itself, the stem cell retains its ability to supply whatever new cells the body needs. Thomson made the network news when he called the human embryonic stem cell “immortal.”
Twenty years before Thomson’s pronouncement, another biologist, Lewis Thomas, had written a short essay entitled “On Embryology,” part of his best-selling collection The Lives of the Cell. In the piece he swoons over the first test-tube baby. Thomas is enthralled with embryogenesis, the process by which cells develop into tissues and organs. He writes that from the onset, in the first “cluster of cells,” a huge array of information is “latent inside every cell in the cluster. When the stem cell for the brain emerges, it could be that the special quality of brain-ness is simply switched on. But it could as well be that everything else, every other potential property, is switched off, so that this most specialized of all cells no longer has its precursors’ option of being a thyroid or a liver or whatever, only a brain.”
What wonder fills his words — as much wonder as science. The voice of Montaigne in a junior high student firing up the Bunsen burner. “One cell is switched on,” he continues, “to become the whole trillion-cell, massive apparatus for thinking and imagining and, for that matter, being surprised. All the information needed for learning to read and write, playing the piano, arguing before senatorial subcommittees, walking across a street through traffic, or the marvelous human act of putting out one hand and leaning against a tree, is contained in that first cell. All of grammar, all syntax, all arithmetic, all music.”
How curious that Thomas foresaw James Thomson’s need to testify before a senatorial subcommittee. Such was Thomas’s gift — to be as thrilled by the mystery and meaning of life (“no one has the ghost of an idea how this works,” he noted of the stem cell’s switching-on of its duty) as he was by the explanation of it. He did say that when someone figures out that switch, Thomas himself will “charter a skywriting airplane, maybe a whole fleet of them, and send them aloft to write one great exclamation point after another, around the whole sky, until all my money runs out.”
All cells divide and grow. But when the stem cell divides, one of its daughters grows toward tissue and the other retains its full potential as a stem cell. The daughter cell that has an intended function, to make skin, for example, will grow and divide until it becomes skin tissue. Biologists call this process differentiation or specialization. The specializing skin cell divides into identical daughter cells. But these cells, as they grow, “express” more specialized genes that produce specific proteins, which can become only one type of cell, a skin cell. Like most differentiated cells, the skin cell can divide only so many times. The skin tissue must be reinvigorated by a stem cell, which like a fairy’s wand supplies the skin with new cells once the old ones wear out.
Stem cells in the one- to five-day-old embryo are called pluripotent cells because they have not yet differentiated and, thus, will generate most other cells in the body. Pluripotent cells are paper heavyweights, ready to do many duties but as yet unleashed, much like a set of first-round draft choices headed for the nfl. Once cells begin dividing toward their intended tissue, in blood, nerves, or organs, they become multipotent or adult. Some cells hold on to their “stemness” as they differentiate. The hematopoietic stem cell is an example of a multipotent stem cell, one that resides in the bone marrow, supplying the blood with new cells as well as self-renewing. Multipotent cells exist for the brain, blood, liver, skin, heart muscle, and other tissues, but not for every tissue and not for every organ. (To complete the spectrum, the totipotent cell is the first two divisions of the fertilized egg — all cells come from it; the unipotent cell can realize only one goal, a particular cell type.)
Cells are the basic element of life. Not only is their quantity of 75 trillion in one human body mind-boggling, but their quality as efficiency experts is equally astonishing. Cells are vital to the body’s metabolism, reproduction, and organ growth. The 200 cell types in our bodies do their developmental work as four basic tissue types. A tissue is the end result of cellular growth and combination. We have epithelial tissues, which form the body’s skin and line the internal organs; muscle tissues, which expand and contract; nerve tissues, which conduct electrical impulses through the nervous system; and connective tissues, which hold together various parts of the body, among them bone and cartilage. Organs are groups of tissue: the heart, for instance, is composed of all four tissues.
What powers the cells? One fuel source common to each cell is its genetic code. Our chromosomal uniqueness comes from the code, that 0.1 percent difference between us. The individual code, lying in the nucleus of every cell, is programmed to undergo, generally, about 100 years of division. The rate is uneven because some cells live longer and work harder than other cells, and some cells simply lose their reproductive ability or else remain dormant. Biologists call cell death either necrosis, from external factors like injury or disease, or apoptosis, from internal causes, like aging or the everyday cell division that insures growth and development. When cells wear out via accidental or programmed death, there’s no need to ask for whom the bell tolls.
Scientists believe generally that once an early cell stemmed toward its intended tissue — for instance, a liver cell began making liver tissue — there was no way to change (one huggable term doctors use is “to coax,” another, less friendly, is “to trick”) its direction. But at least one researcher I spoke with said that a few biologists are discovering that cells may be rerouted from one stem-direction to another.
Dr. Edward Ball, who directs the UCSD Bone Marrow and Stem Cell Transplant Program, told me of newly found cellular trade winds, much like Portuguese explorers seeking routes to the East. “In muscle there are stem cells that give rise to blood; in bone marrow you can see evidence of liver stem cells; in brain there are cells that can give rise to bone marrow. So the stemness of these cells is much more diverse than we thought.” These are, please note, evidence only of the cells’ presence and inclination. No one knows how to nudge one toward its goal. But, as Ball said, the experiment with Dolly the sheep proved that a given cell could form a whole new organism. In fact, Ian Wilmut, the British embryologist who cloned Dolly, placed adult sheep cells in an embryoniclike culture where they “thought” they were growing inside an embryo just like stem cells. He then fused one of their nuclei with an unfertilized donor egg whose original dna was removed. One hundred forty-seven days later, baa-baa-baa-baa, it worked. Genetic medicine and molecular biology haven’t been the same since.
UCSD, as pluripotent a research-intensive school as you’ll find anywhere, is bristling with stem cell inquiry. Doctors Lawrence Goldstein and Ewa Carrier, in medicine, and Bernhard Palsson, in bioengineering, oversee labs that, in their insufferable nondescript gray buildings, are at least within earshot of each other. The lab research, done largely by graduate students and technicians, centers on mouse stem cells and other applications. For example, Dr. Carrier specializes in stem cell transplants, while Dr. Palsson and his staff are recording the migration and metabolism of stem cells with some dazzling time-lapse video. Broad-shouldered labs packed with incubators, microscopes, sterilization tanks for petri dishes, and shelves sagging with colored three-ring binders are abuzz with ongoing experiments and the occasional flurry of discovery.
In Lawrence Goldstein’s lab, technician Liz Roberts is opening an incubator where she’s cultured mouse embryonic stem cells. She brings out several dishes to show Goldstein and me a succession of experiments. First, she’s grown a feeder layer of cells on which she has placed stem cells. (What I’ll be looking at are the descendants of a mouse stem cell that was removed from a blastocyst and frozen a decade ago in Canada.) Roberts, who worked with handicapped children before joining the lab, has stopped the cells’ propagation after three and a half days. She wants me to see a ragtag cluster of 32 or 64 stem cells in their near-perfect pluripotent state. She says they’re “quite happy” clustering together on the feeder bed. “If they aggregate too quickly, they start differentiating. We try to keep them in a single-cell suspension” — that is, separated — so “each cell is left to divide and form its own colony.” And to colonize is what these cells crave.
The clump of cells in the dish is what Roberts calls “an embryoid body,” not an embryo but a colony of stem cells that thinks it is making an embryo. Without the mother’s uterine environment, however, the cells can’t do it.
On this note Goldstein joins the discussion. An investigator for the Howard Hughes Medical Institute (that is, the Spruce Goose himself), Goldstein is a one-time triathlete (he blew an ankle out) who now manages a careful four miles a day. With premature gray hair and a nose like a knife, he enjoys explaining the particular intelligence of cells. “They’re confused,” Goldstein says of the cells Roberts has isolated in the dish. “They usually rely on signals from their neighbors” (other kinds of cells, growing and differentiating, around them) to proceed. And yet, they “remember” being a mouse embryo. Goldstein’s anthropomorphism feels deliberate: He insists that we compare the behavioral model of mouse stem cells to their human counterpart because gene and cell research, now reserved for mice, will begin on human embryonic stem cells, sooner than later. Those human stem cells will not be in a growing embryo. Mouse embryonic stem cells, at rest in a petri dish, “cannot become a mouse,” he says. And this, he states, is the same for our species. Biologists are “always very careful to distinguish that human stem cells [removed] from embryos are not themselves humans. They do not have the capacity to become human any more than a cell from your arm at the moment can become a human. Genetically they’re the same. It’s just that the cells in the early embryo know how to become a lot of different kinds of tissues and organs.”
With a little poking, Roberts is able to bring a few individual cells into view. “If you look at ten o’clock, you’ll see one smooth, circular cell — that’s what we like.” With her glass needle, she can pick one up or, if necessary, puncture and retrieve its dna from the nucleus. In fact, this technique is what Goldstein’s lab does regularly — genetically modify these stem cells and inject them into mouse embryos. Then they study what those cells do down the cellular line as the mouse ages.
Finally, Roberts shows me a few stem cells that have begun differentiating. These she’s cultured in another petri dish so they would mature as if they were in an embryo. At two weeks, this embryoid body is spectacular, a ball as pocked and still as a harvest moon. Roberts calls it “incredible, [like] a hollow golf ball.” The body is already beginning, in its cellular spectacle, to differentiate into the tissue properties of a mouse. But it can only go so far, lacking its uterine home. By adding certain proteins to the media, Roberts might convince the cells that they were in the brain and, thus, they might turn on their brain switches and start dreaming about cheese. But in this case, she is coaxing the cells to become heart cells and, if we’re lucky, begin beating with the recognizable rhythm of cardiac muscle tissue. Roberts says she’ll call if the cells start pulsing, but, alas, she never does.
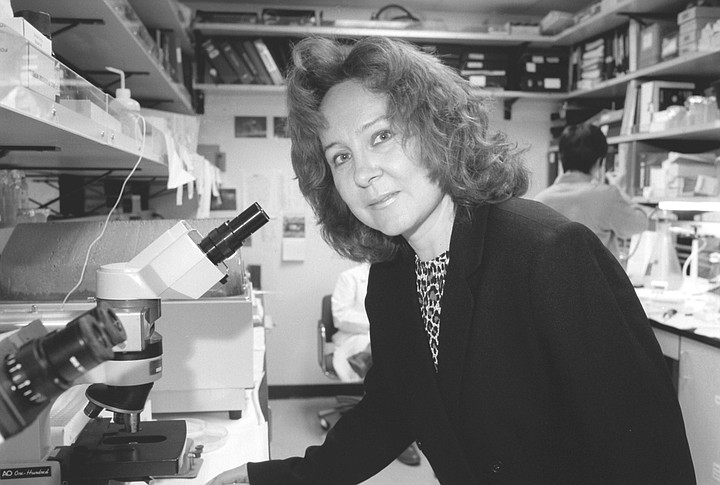
Across the street in another crowded lab shared by Dr. Ball and Dr. Carrier, work is progressing on bone marrow and stem cell transplants in humans and on stem cell applications in the uteruses of mice. Ewa Carrier speaks in rushes of technicalities about her research, as though every treatment she hopes to administer is bursting from her at once. Today in a green jacket and black turtleneck, the Polish national has a cherubic face, brownish-red hair, and open-tap energy. Having worked with lymphoma patients at Stanford, she now devotes herself to pediatrics and prenatal transplantation with hematopoietic stem cells. Her specialty, though, is rarely done: helping children born without immune systems, commonly known as the “boy[s] in the bubble.” She has developed a fetal transplant model using stem cells that she believes will save them. Otherwise, exposed to our surroundings, they will die.
She describes her inquiry as cell, not gene, therapy because the immunodeficiency diseases she studies occur in the cell. “When you provide healthy stem cells, they will cure the disease,” she says. Cellular therapy can be combined with gene therapy. “You take stem cells, put them in a tube with a healthy gene, mix them, then put them back.” But there’s a caution: If Carrier introduces genes to provide an immune system to a child born without one, she is unsure she can control the gene transfer at the embryonic level. Even if the gene therapy works in the patient, there may be complications in the hereditary germ line of his or her offspring. Not enough is known about propagation down the genetic highway after transplantation. Thus, Carrier has agreed with the finding of the National Institutes of Health that more study needs to be done before actual gene-cell therapy in humans occurs.
Carrier’s nongenetic “in utero transplant protocol” for humans has been approved by the fda, but she has not yet performed one. She has done a similar transplant in mice, which, she says, is very difficult. “You have to expose the fetuses, which are in the uterus, transilluminate them, and [work with] a delicate microcapillary tube [like a glass pipette]. You need magnification [to] introduce the stem cell solution to each fetus. Put the fetus back, let it grow, be delivered, and study its life to see what happens.”
Children born without an immune system must be kept in a germ-free environment, the bubble, in order to live. Eight fetal stem cell transplants on such children have occurred throughout the world. One, she says, has been quite successful, with a boy surviving with a strengthened immune system now for 12 years.
Her protocol ready, Carrier’s next step is to advertise on the Internet for patients, who are quite rare. She hopes to locate a history of immunodeficiency disease in a family, preferably in a child whose mother is thinking of getting or has gotten pregnant again. If the mother is pregnant, Carrier can present her and the father with options — abort the fetus, treat the disease in utero, or wait for a postnatal transplant, which can be toxic. Treatment options are highly experimental and risky. If the couple consents to treatment, Carrier will take the hematopoietic stem cells from the father and inject a five-milliliter solution into the liver of the in utero fetus in the second trimester. Finally, she will track the fetus through birth and into childhood to see how robust an immune system the child will grow.
Jody Donahue is Carrier’s chief technician. The former ballet dancer turned stem cell researcher focuses on fetal transplantation using mouse stem cells. She shows me a photograph of an anesthetized pregnant mouse, splayed out on a cloth, her abdomen open and bulging out (like large intestines) a multifetal uterus. I count nine mouse embryos in whose livers Donahue, with microscope-glasses, injects purified stem cells. In the photo, the fetuses are entombed in their sacs. How do you know where to stick the needle? I ask. Donahue says, “Wait,” and reaches to a stand of capped glass vials, each the size of my pinkie. She hands me one. There in alcohol bob a half-dozen mouse fetuses, yellowy-white and stillborn at 12 days of gestation out of the mouse’s normal 20 days. “See that dark blotch?” It’s like the half-moon dark under a fingernail. “That’s the liver.” That’s where she injects stem cells into the living fetuses. With a healthy liver, the mouse will double its stem cell count every day until the 14th day of gestation.
Surgical candidates, these mice have thalassemia, which is an anemic disorder that occurs in mice and humans. (Thalassemia is inherited among people of Mediterranean descent much the way sickle-cell anemia, a recessive genetic disorder, is inherited by people of African descent.) Donahue and Dr. Carrier hope to discover whether stem cells can cure the disease. And so far their experiments have yielded mostly healthy mice after the transplant.
Donahue is fascinated by the potency of the stem cell. Although she cautions, “Stop me if I start to lecture,” her explanations are concise. This cell, she says, “is one that renewed itself, then stopped. It created a daughter but didn’t change itself. There’s only one cell in the body that can do this and that’s the stem cell. Their progeny create the entire system” of the body. She smiles reverently, telling me of a Japanese researcher who “lethally irradiated” a mouse (destroyed its immune system) and then transplanted only one stem cell. The mouse grew an entirely new immune system.
But how the stem cell does this from its initial divisions is, she says, “not well understood.” Researchers know pluripotent stem cells start in the yolk sac, migrate to the fetal liver, then settle in the bone marrow, becoming stromal cells. Next, they move inside the bone, “form a latticework,” and pack themselves into “little niches.” She says they both divide and rest, much less active than other cells.
In the animal vivaria, or mouse house, at UCSD, Donahue and I are joined by Dr. Phil Richtor, the campus veterinarian. It’s another hospital-like ward of shiny corridors and small sunless rooms, now smelling of rodent. Getting in takes a few more who-what-why answers than normal, since the occasional animal-rights protester has tried (and failed) to liberate these cages. Donahue untops an elaborate box and pulls out from a pile of vibrating straw what Richtor calls “your typical research mouse.” Wearing pale yellow plastic gloves, Donahue holds up a mouse who “was transplanted with stem cells from a different strain of mouse, an unmatched donor.” Her voice softens, her maternal instinct rising palpably. “She survived” the transplant, she says, “but she’s a little nervous right now. Curious, but nervous.”
One of hundreds of types of white mice, this one’s “a laboratory-specific mouse, originated, I’d say, 30 years ago, an inbred strain so that all the littermates are genetically identical.” Donahue next cups a very pregnant brown mouse, with about a dozen little sacs pushing out like Santa Claus’s bag of toys from under the skin.
What is it about the mouse that lends itself to so much prehuman research?
Humans and mice have very similar hematopoietic systems. Mice also make perfect subjects: Diseases can be bred in them that could never be bred in humans. Most of what we know about human immunology has been gathered from experiments on mice. Donahue next shows me a seven-day-old pup, sniff-snooping the air, blind as a bat. She pets, oohs and aahs, seems to love her tiny charges. Clearly, her care for mice she experiments upon is not a contradiction. It is gratifying to hear Jody Donahue and Liz Roberts mention children as the main impetus for their work, children born with diseases who may soon be aided by pre- and postnatal transplants using stem cells.
Elegantly attired Bernhard Palsson, born and raised in Iceland, “of all places,” he tells me, has an office perch on the sixth floor of the Irwin and Joan Jacobs School of Engineering building. There, he is working (like Dr. Carrier) on the hematopoietic stem cell, those cells from which our blood cells originate.
After a handshake, he directs my attention to the scientist’s equivalent of the baby’s portrait on the desk — a framed copy of an enlarged cover of the journal Blood. On the cover is a photograph of a hematopoietic fetal liver stem cell, which his lab caught in some exotic dance. Attached to the cell is a podia, a cytoplasmic extension or tubule, very narrow and extremely long. In the color-dye-enhanced photo, cell and podia look like a ball with a long tether or noodle loose in space. Some stem cells, he tells me, are 5 to 10 microns wide and send out podia 300 or 400 microns in length. “It’s like you, being 6 feet tall, reaching 200 feet away.” The photographic discovery has “caused a lot of excitement,” he says. “It is something totally new in cell biology.”
What do these podia do? “In cell biology it’s very hard to prove a cause and an effect,” Palsson admits. “I don’t know what that [podia] is — an antenna, maybe.” Cells are blind, so the extension may be like a cane, tapping down the sidewalk toward new tissue. “It may,” he continues, “be going to touch another cell, so it could be a new [kind of] cell communication. It reaches out and touches someone. Sometimes we see nodules, a ball in the membrane, moving up and down the line of the podia. Sometimes we observe the podia grab on to something and then reel it in like a fisherman reels in a line. The other cell is stuck [on the podia] to the point of attachment.”
Palsson seems comfortable with being not sure. With a degree in chemical engineering, he’s been involved in clinical trials for bone marrow transplants and stem cell research as well as developing “tech-transfer” applications, whereby academics convert their discoveries into biotech products and, they hope, profitable companies.
When asked why stem cells are so important today, Palsson responds that they are “the source from which you can derive a large number of cells to transplant or manipulate.” He notes that bone marrow is “the body’s most prolific tissue; it generates as many cells as it’s comprised of every three days. It’s unbelievable.” If you calculate such zeal over 70 years, you find bone marrow producing 500 times one’s body mass in a lifetime. Bone marrow is “driven,” he says, “by these highly prolific stem cells.”
Palsson employs the word “quiescent” as the stem cell’s main state, but, when stimulated, “They can generate tens of millions of cells. Like ticking time bombs ready to go off.” He explains how a stem cell can halve itself into identical cells; into two nonidentical specialized cells; or, a third way, asymmetrical division: one, a daughter cell, the other, a cell that will specialize. Palsson questions the putative “immortality” of the stem cell, because no one has demonstrated that they “stick around forever.” He says “their proliferative capacity…diminishes with age.” The stem cell is most productive in the fetal liver, next in the umbilical-cord blood, last in the adult. “The younger the source, the better.” And that, he says, opens all sorts of ethical questions.
One case he knows of involves parents of a child suffering from a blood disease who had another child to harvest stem cells from the umbilical-cord blood. Of course they did not dispose of the new child. But, quite purposefully, they had a second child to save the first one. Another idea, untried as yet, says Palsson, is to abort a fetus in order to harvest the fetal liver cells, which are the most “proliferative,” in order to cure a fatal disease. In yet another scenario, which he stresses no one he knows has attempted on humans, is to split up the first four stem cells (that is, after two divisions following fertilization) and grow them in four separate uteruses. (Recently such a birth was accomplished with one of four surgically divided and implanted embryonic stem cells of a monkey.)
A particular question Palsson’s lab is investigating concerns what happens to stem cells as they divide and begin to specialize or migrate to their tissue sites over time. To describe this visually on film would summon the most creative of video-savvy bioengineers. Enter Karl Francis, a former robotics operator at Pasadena’s Jet Propulsion Laboratory, who helped fly Voyager and Galileo unmanned spacecraft and has, with a Ph.D. in bioengineering, turned his ingenuity to good use in Palsson’s lab.
Francis’s time-lapse digital camera system, still and video, studies stem cell migration and division. To do so he built a large plastic box to fit around a multiwired camera and temperature-controlled system, “essentially,” he says, “an incubator around a microscope.” The media in which the stem cells grow has a bicarbonate of soda base and must be infused regularly with carbon dioxide. In order to maintain an atmosphere perfect for stem cell growth, sometimes for up to a month, Francis installed as his heat source an Oster dog dryer he got at the pet store. The resulting balm is a toasty 98.6 degrees Fahrenheit, a Tahitian climate for cellular productivity.
In a five-minute video of time-lapse and real-time tape, Francis shows me stem cell division along with the modern dance of their podia. The real-time film begins in an apparent swimming randomness of cells, and then a stem cell cleaves in two. Next, a cell shoots out a tentacle, the podia, which the deadpan Francis says, reflecting on the first time he saw it, looked to him like, “I don’t know, an octopus. Here’s a mouse stem cell,” he gets a bit animated, “and you see a lasso at the end of it, which loops back and adheres to itself.” Some podia tips come into contact with other cells, presumably to trigger a chemical reaction, then snap back, jilted or kissed. (It’s hard not to anthropomorphize cells in this microscopic rodeo.) He describes one podia as forming a “string of pearls,” while another podia breaks off from its owner. Maybe, he hypothesizes, it’s sending out “a note in a bottle.” Another podia, tugging on a cell, shows some material being transferred, like reeling in (or out) “the clothes on a clothes line.” I compliment his metaphors, though he mentions having practiced by showing this tape a dozen times. In none of what he observes can Francis say which of the dividing cells is the daughter and which is the specializing cell. Nor can he say what that specialized cell will become. But he can say that these stem cells face Everest-like climbs, which he, Palsson, and other scientists are only beginning to grok.
Not all stem cells are free from worry like those healthy tribes grown in Bernhard Palsson’s lab. Some stem cells can be diseased or can carry an illness, sometimes for generations. Leukemia, or cancer of the blood, is believed to be caused by a mutation in a hematopoietic stem cell residing in the bone marrow. Like a dormant cancer cell, this blood stem cell may or may not become active within a person’s lifetime. However, if a genetically diseased stem cell switches on, the cell will divide and send out progeny with the same characteristics, in effect, cloning itself as leukemic cells. The worst is, anyone can develop an acute leukemia, at any age and without warning. Before current treatments, such a disease killed more than 90 percent of its victims.
No one knows this better than Heiju, a woman of 33, born and raised in Taiwan and now living in San Diego. (Heiju requested I use only her given name, which is Chinese.) In May 1999, Heiju and her husband were trimming a rubber tree in their yard one weekend, no overly physical activity. That evening Heiju noticed her hands were bruised. She asked her husband whether he’d gotten any bruises; he said he had one or two. The second day, she had more bruises and swollen glands. She also noticed on her leg “red dots under the skin,” then discovered “bloodlike lines” underneath her eyes. There was no pain, only these persistent symptoms.
On Monday Heiju went to work. She felt fluey, but otherwise normal. Soon she suspected the bruising was too strange not to be serious, so she drove herself to a Mira Mesa clinic, where she was told to go to an emergency room. There, a doctor said he wasn’t sure what disease she’d contracted, but she needed urgent care. Admitted to UCSD Medical Center in Hillcrest, she learned from an oncologist that she had leukemia. A few blood tests later they diagnosed it as acute lymphoblastic leukemia. Her white cell count was so high that it kept the red cells from functioning. Her platelets were severely curtailed: Without platelets clotting the blood, she might bleed to death; with too few red cells, she could become anemic; without oxygen or nutrition being carried to the tissues and organs — the purpose of red cells — she could not live. The doctors began chemotherapy at once, to boost the red cells and lower the whites.
Had anyone in her family had leukemia?
Heiju tells me, over lunch recently at the Hong Kong Chef, “none that we know of.” Her great-great-grandfather came from Fujian province on mainland China, one family branch she and her mother have not kept in contact with. Had that man had leukemia, say a century ago, he would probably have bled to death. Heiju may have acquired the disease, but she says the doctors can’t explain how. At first she understood the illness, but now, thinking back, she says confidently, “I had no idea of the depth of the disease.”
Her chemo treatments progressed for a month. She reports feeling “spacey,” trying to focus while she and her husband searched Internet reference sites to learn about their options and her survivability. The latter was not good. One source reported only 20 to 30 percent odds of pushing the leukemia into remission. Heiju says she didn’t panic or suffer major depression; she studied, read, asked questions. In the process, though, she learned so much about leukemia that she ping-ponged between feeling “out of control” and certain she’d survive. Quickly she found her mantra: “I know I have a strong will to live. I know there is a reason for me to continue living. All I have to do is start planning” for one of the treatment options.
At this point Heiju’s care was transferred from Hillcrest to UCSD’s Thornton Hospital where Dr. Ewa Carrier arrived on the scene. Carrier told Heiju she could stay on the chemo for a year and a half, with injections every month. The survival rate was 30 percent. Another possibility was a stem cell transplant. It would require passing a number of “eligibility” criteria — the stage of the disease, the sex and age of the candidate, the availability of a donor. Once deemed eligible for a transplant by Carrier and a team of doctors, Heiju was buoyed, in part, because she feared she couldn’t endure a year and a half of chemo. But, even with a transplant, complications might arise: permanent damage to the liver and the lung, the macabre-sounding graft-versus-host disease, where rejection of the new cells can occur. The survival rate for the stem cell treatment, however, doubled that of the chemo. Heiju wanted that chance.
She didn’t have to look far for a donor. One of Heiju’s three sisters in Taiwan volunteered to be tested. When the call came that her sister was a match, Heiju was only half-pleased. She had one more treatment, perhaps the most difficult — irradiating the leukemic cells in her body. She was bombarded with radiation and an equal assault of chemo, which, she says, “killed everything that you can possibly see [in the blood]. My white cells actually dropped to zero.” This was the “condition,” albeit it severely weakened, the doctors wanted — total decimation of the leukemic whites. Now she was ready for the stem cells.
Heiju’s sister and mother flew in from Taiwan, and the sister, no sooner than she was off the plane, had to endure apheresis, or blood collection. This meant drawing blood via one catheter out of her right arm, passing it through a device that filtered out the stem cells, then pumping the blood back through another catheter for its return to her left arm. Heiju’s sister underwent blood culling for four days, some days being drained and replenished for up to six hours.
Finally, Heiju got the full weight of stem cells from eight packets of blood, much like a transfusion. She felt dizzy as a chemical in the thawed stem cell solution filled her lungs, and, for 15 seconds, she got “less and less air [and] my face got hotter and redder.” But the vertigo stopped and, within 20 minutes, the transplant was done, a far easier regimen than the radiation and chemo treatments that had prepared her. In all, four months had passed between the appearance of the bruises and the transplant. Two weeks later Heiju was out of the hospital and has been recuperating steadily without any side effects. When we have lunch in early February, she is quite healthy, lively, at times zestful. She’s back working (in computer graphics) from her home.
I ask if she and her sister (who now share the sister’s blood type) are closer. “It changed my perspective on life,” Heiju says. At a stem cell transplant support group soon after the operation, she says she was able to testify to others about how much she now values “family relationships. I feel so much closer to my mother and my sister. Life in general is easier. I used to be upset by petty things. Not anymore. And most of all, I feel like I’m three years younger.”
We share a laugh, after which I remark that Heiju probably feels rejuvenated because she swiped all those good stem cells from her little sister.
She says that’s true. But her sister felt no physical complications from the apheresis. “Once you donate your stem cells,” Heiju says, “20 or 30 minutes later you’ve got them all back.” Those rear guards who hide in their bone marrow niches know what has happened and quickly — as is their nature — self-renew.
Dr. Gail Naughton is the president of Advanced Tissue Sciences, a biotech company of 200 employees that sits across from the golf course on North Torrey Pines Road. In the 15 years since she began the business with her husband (they are now divorced), she has grown human skin and other tissue types, mostly to aid burn victims. So far she has avoided using stem cells. She’s still not comfortable with it because, as she tells me in a small conference room (she is dressed in a red pantsuit with pearls and a black turtleneck), “Society doesn’t understand how to deal with stem cells” yet. She knows the universities haven’t researched and tested these cells nearly enough. In fact, she predicts, “Embryonic stem cells are years and hundreds of millions of dollars” from their highest rung, growing organs. Still, she’d like nothing better than to be making liver with human stem cells. “I think,” she leans forward, her large brown eyes very serious, “embryonic stem cells will be the key to guaranteeing every person who needs an organ can get one.
“If I wanted to grow a liver today, can I grow one? Yes.” Naughton is confident, like a betting woman putting her money on a favored filly at Del Mar. I hold out my hands to mime (fish-story caricature) the size of a liver: What? about 16 inches? “Well,” she counters, “I can’t grow a whole liver. But I can grow enough to help somebody with an enzymatic deficiency.” The possibility enthuses her words. “We know how to grow liver, we know [how] to keep it alive outside the body for months, absolutely functional, making all the right proteins, all the right enzymes, and liver’s a very complicated organ.” (In what may be science fiction, a team of researchers at a recent Toronto conference set themselves the goal of growing an entire human heart from scratch within ten years.)
“If you give me an embryonic stem cell,” Naughton continues, “and tell me how to direct it into a hepatocyte [a liver cell] chemically,” she can grow a liver. Scientists, she says, will look at the genetic code and determine what type of tissue this stem cell will stem toward. Once they know this — turn the switch on — then biologists can create the host environment that “mimics” conditions that cells recognize. Biochemical trickery.
Naughton says Advanced Tissue forgoes using embryonic stem cells because the company is “product focused.” The cells they do use to make skin and cartilage come from donated foreskin fibroblasts, after routine circumcisions. Fibroblast is made not of stem cells but of specialized cells that make connective tissue. This is, Naughton says, “young healthy tissue” whose mother and child donors, once they have consented to the foreskin donation, are tested “extensively” for viruses and diseases. This tissue is good, Naughton insists, because it “always comes from the same age, same sex, same anatomical location, [minimizing] the difference from one starting material to another. It helps us make a uniform product. It also has huge expansion potential.” In the company’s dozen cell banks, their present stash will take them “through decades of production.”
I get an idea how huge an expansion it is from a tour of their facilities. Rob Sorenson, director of manufacturing operations, lets me peer through windows at sterile areas watched over by technicians in head-to-toe gowns, cycling and recycling nutrients in order to keep the growing skin tissues alive in their two main products — Dermagraft, to treat diabetic foot ulcers, and Transcyte, to treat burns. One itsy piece of foreskin, he says, can, through eight cycles of cultured division or some five million scaffolded cells later, cover six football fields.
At last it’s time for me to touch some advanced living tissue. I’m escorted, wearing a nylon lab coat, into Twana Davisson’s lab, where she is growing cartilage. An under-30 African-American woman working on her Ph.D. in cell biology at UCSD, she is making human, equine, and bovine “constructs,” that is, cartilage tissue that can be shaped for animal and human transplants. For cartilage in large animals and humans, she says, the major similarity is their “weight-bearing,” which horse, cow, and human put on this small but virile substance.
“Tomorrow,” she says, “I’m getting in cow knees. We’ll take the cartilage off the bone, digest it down, and take the cells out. Then we’ll passage [divide] the cells and seed them onto pieces of felt.” Compute passage at Advanced Tissue like this: 100 cells, grown in roller bottles, become in a few days 1,000,000 cells; remove them and divide them into groups of 100 and grow those 100 again to 1,000,000; that’s a passage.
“We grow them in an incubator for weeks at a time,” Davisson says, “and they come out looking like — ” She points to a pint vial of liquid, where a little frosty white chip of human cartilage floats. “Like this,” she says nonchalantly. She tells me, as I don plastic gloves, not to inhale the Formalin, an asphyxiant that, breathed in, will affect my brain. I avert my face; the hard patch of goo is laid in my open hand. This cartilage — like most everyone, I’ve never handled live cartilage before — feels otherworldly, a sort of bumptious, dense plastic, not so much alive as gelatinously rigid. Certainly not pulsing with life. I test its tensile strength and, oops, it breaks in two. Davisson retrieves it, saying not to worry, she can grow more, although I wonder if I’ve just ripped up something destined for Ryan Leaf’s throwing arm.
Next, Davisson shows me a flask in which cartilage cells will, in a petri-dish media solution, proliferate. The medium is a red Kool-Aid–like liquid, nutrients that keep the cells supplied with food. This is one of the most interesting aspects of tissue engineering — the nutritional concentrate that mimics the body’s vicinity, in this case cartilage, where the cells grow. All these cells “know” is that the medium is providing sufficient nutrients to sustain them. Under the microscope, at 40-power magnification, I can see the colonies of cells, the chondrocytes, like curled eyelash-tip ends clustered together in small lumps of division: two, four, six. Davisson says that these “cobblestone” clusters “will become confluent, and there will be cells everywhere.” Once they divide into millions, Davisson will lay them onto a scaffold, a three-dimensional polymer, where the cells spread out and connect with each other, creating a matrix protein. The scaffold is biodegradable. Once the chondrocytes colonize the space — that is, fill the scaffold — they stop dividing. Then the scaffold dissolves. Presto, in its place is three-dimensional tissue.
Naughton sees a rosy future for building organs with embryonic stem cells once geneticists learn how to switch the cells’ codes on and off. Roger Pedersen, a biologist at the University of California, San Francisco, calls this switching a “language of signals and receptors,” the signals coming from chemicals that secrete into the cell’s neighbors and the home-grown receptors that hear the signals. “We know the semantics,” Pedersen writes in Scientific American, “but we don’t understand them because we can’t eavesdrop on the embryo very well, where this intimate conversation is going on.” Eventually Naughton will be able, she says, to coax stem cells “into liver cells, into neurons, into pancreas. We’ll be able to make those organs cost-effectively and safely because this one cell bank [of human embryonic stem cells] will give rise to all of it. That’s what you will see this decade.”
Preempting the competition, Advanced Tissue already owns a patent on creating tissue from what are called mesenchymal stem cells. These are the master cells from which fibroblasts and other connective tissue differentiate. Naughton says, with research on the “next level” of mesenchymal stem cells, her company will prove “how quickly products can be brought to market.” She believes “when science gives us answers about embryonic stem cells,” Advanced Tissue will be — ready, set, go — in the business of “making new organs.”
Two things are clear from discussions I’ve had with doctors and patients about stem cells. One, the cells’ potential is astronomical, and two, such potential is weighed down by the following choices: Do we or do we not derive, do we or do we not use, stem cells from aborted fetuses or donated embryos after in vitro treatments? (Deriving and using adult stem cells to treat leukemia poses no problem, as long as there’s an adult donor.) No one wants to make an embryo, that is, make “life,” only to derive its stem cells, then discard the embryo. And yet most people support the medical and research use of an embryo and its stem cells, if it is going to be discarded. An embryo’s “right” is a difficult nut to crack because only the early-stage embryo contains the most pluripotent of stem cells. Nothing seems more apt than Roger Rosenblatt’s labeling the embryo, in his book on abortion, Life Itself, “an entity of uncertainty.”
Derivation versus use drives the way we talk about embryos and stem cells. For example, what do we mean by the idea of an “excess” embryo? Do we even call one an “excess”? Can we even talk about an embryo — think of Jeffry and Cristen’s indecision about their embryo’s physical and moral status — as having given its “life” to science?
When I ask UCSD investigator Lawrence Goldstein what happens to the embryo after the stem cells are removed, he says he would “look at [the question] differently. During the derivation of embryonic stem cells from a blastocyst, they are derived from blastocysts that are destined for discard anyway,” his final word pinging. These are “excess embryos” from fertility clinics “beyond the need of the donor parents. The act of taking the stem cells has not changed the ultimate fate of those embryos.” Which means — I will say what I think needs stating — the embryos die.
Goldstein then topsy-turvies my question. “Would it be possible to remove the stem cells from an embryo and have that embryo remain viable? I would argue that it’s completely unethical even to do the experiment.” His distinction is this: One does not manipulate embryos that are destined to be implanted in women. But one can do research on embryos that are “in excess of clinical use,” a definition Goldstein feels most comfortable with. He wants me to know that he has friends who are anti-abortion and who also believe “it unethical not to use the tissue left” after any fetal discard. “In that sense,” he says, “it’s the same as an auto accident. Nobody wants an auto accident for organ donation. We would not go out and terminate people for organs. But if it happens, then we should take advantage of that in some ethical way.”
David Smotrich says that for patients the decision to freeze an embryo is as “emotionally difficult” as it is to thaw it out, for donation or discard. Smotrich wishes the public, too often incited by abortion politics, would be more sensitive about the phrase “in excess of clinical need.” He cites the recent concerted move by in vitro clinics in England to notify patients who had embryos still on ice and were not paying for their storage. After a massive get-out-the-word campaign, the clinics thawed out all the unclaimed embryos. In England, he says, the outcry was nearly inaudible. But in the United States such a move would create a “tremendous uproar,” perhaps inciting street fights and re-igniting the abortion war. Indeed, who would march on behalf of destroying embryos? Smotrich admits to having difficulty saying at the embryo stage, before implantation, that it is “life,” but he does “respect the fact that it [has] potential for life.” His hoped-for sensitivity reminds me that Americans’ view of “excess” can never be clear-cut, since the antiabortion wing has concluded that fetal rights exist at the moment of physical conception, in or out of the womb.
Ewa Carrier describes her research as misunderstood, especially where the fear of abortion struggles with the need for embryonic stem cells. To develop a plan, Carrier spoke with a French physician, Dr. Touraine, who advocated the creation of a fetal-liver bank in which, postabortion, small “chunk[s] of fetal liver” would be frozen. To help his countrymen understand why, Touraine published a book describing the fate of immunodeficient children who might be cured by stem cell transplant using these livers. Carrier says he “activated” the public to support him. The French Assembly followed and now regulates the collection of fetal livers.
That happened in France, Carrier remarks, a “very progressive country.” In the United States, it’s much different — lack of regulations accompanies political and religious opposition. She says people here fear her procedure “will promote abortion.” If there’s a private bank, people will, so goes the claim, provide aborted fetuses to make money.
Still, Carrier recognizes the difference between “research” abortions (which some have dubbed “embryo commodification”) and “necessary” abortions for severely diseased fetuses. “People have the option of abortion when they detect a disease prenatally. Prenatal diagnosis is the standard of care right now. What I would like to do is provide the option for treatments [on the fetus itself] so they don’t need to abort.”
Carrier speculates that the Catholic Church’s greatest fear is abortions for science. She says Catholics believe that if “you start terminating life, you may go on to terminate adults. With children who watch lots of violence on television, after some time they think that violence is just part of life. They get used to it. The threshold goes down. The Church has concerns I can respect. [But] abortion is different than therapeutic [surgery]. I have no problem with this, being Catholic myself.”
Congressman Brian Bilbray, a pro-choice Catholic, worries also about confusing abortion politics with the regulated, therapeutic use of stem cells. Bilbray supports stem cell research. In a recent interview at his Mission Valley office, he told me that he believes strongly in the benefits of donation after his three-month-old son died in 1984 of sudden infant death syndrome. Bilbray says he and his wife “felt a moral obligation that [our] baby’s death could have helped another baby.” At the time, they wanted to offer the child’s organs for transplantation, but the option wasn’t possible. What was possible for Bilbray was to support, with moral authority and political advocacy, the “good” to come of research and transplants.
He thinks that when sperm hits egg there is no “full legal person,” but there is a “moral person. From my theological point of view, life is created at conception. That is not identified as a legal person.” If the embryo is a legal person, he says, then “legally there isn’t any way to address it. Fertility clinics would be outlawed. If you have ten fertilized eggs, you have ten persons. What do you do with the other nine that are not being used? There is no way legally for our society to address that. If the fertilized egg is not going to be used, then you have a moral obligation that there’s as much beneficial use of those fertilized eggs as possible.”
Abortion politics and emotionalism, says Bilbray, go hand in hand. The main problem with such politics is that people use “the emotion of the abortion issue for other agendas.” He doesn’t believe that stem cell research, the creation of excess in vitro embryos, fantasies about “embryo farming” and “bioslavery,” will encourage abortions. Instead, these things will promote “fearmongering. The emotionalism played for political reasons…doesn’t scare me. We need ethical standards. I have no problem with saying there shouldn’t be the creation of life or the destruction of life. I also believe that if there is going to be a loss of life, there should be the maximum benefit made from that life. That life should mean as much as possible.”
I ask about Washington’s role in all this. He says “as usual” he’s wary of governmental intrusion into private family decisions. “The well-intentioned insensitive big government walking in to help many times creates more problems than it solves.” He says it may be politically advantageous for him to say that “this [research] is a threat to the parents’ right to decide. But I think we have a responsibility to make sure that federal funds are utilized appropriately. Some believe that means no federal funds involved in stem cell research. I disagree. It means we set up appropriate moral guidelines to make sure that the federal funds are not used to abuse the privilege of the research.”
On cloning or on stem cells, he says, both are “a great boon to mankind.” He hopes we use San Diego’s “brain trust” at UCSD and in the biotech firms of Sorrento Valley to develop stem cell therapies. (Incidentally, I hoped to but did not find human embryonic stem cell experimentation going on locally; only the brave, the few, and the privately funded elsewhere are involved.) Bilbray disagrees with his Republican colleague Rep. Jay Dickey of Arkansas, an antiabortion antagonist to stem cell research. Dickey says embryos have “the same moral status as a live human baby.” While Bilbray is in step with the House Republican majority on some abortion issues, he says, “I think I stand where the average person stands on this one.” His position may soon be vindicated when guidelines recommending federal funding for human embryonic research are approved by the National Institutes of Health. The battle may begin anew, for Dickey and his House cohorts, some 70 in all, are vowing to fight the National Institutes of Health and ban embryonic stem cell research altogether.
Some parting observations.
Lawrence Hinman, ethics professor and head of the Values Institute at the University of San Diego, joined me one day to discuss stem cell research. Perhaps his most valuable point was this: We are facing such difficult bioethical issues today because new technologies, which came about entirely from our tinkering, have brought us choices we would have never had to make. The fact that in vitro embryos exist, in the hundreds of thousands, coupled with the fact that we will use their stem cells, is indicative that technology, not science and surely not ethics, is running our lives. “The presence of certain technologies,” Hinman told me, “creates a pressure to employ the technology.
“Let’s say that you could choose your children’s eye color,” he suggested. “If it became technologically feasible and affordable, then wouldn’t that establish some pressure on prospective parents to choose it? If as parents we are short in stature, and they discover the switch for tallness, then look at the ethical dilemma. Should we turn the switch on so as to insure tallness, knowing that models and athletes in our society have, supposedly, better lives? Or should we turn the switch off and insure shortness so the child will be like us?” Is this a problem that humans should even be contemplating, Hinman wondered, or is this a technologically imposed dilemma, a purely manufactured construct that suddenly, like it or not, we have to answer?
Developing a Holy Grail of stem cell treatments is no different. Any breakthrough in its fast-track technology will create the pressure to employ that technology and leave us with new ethical conundrums, perhaps at the glad tradeoff of eradicating our most virulent diseases. But the question remains, will we be able to adapt to a world in which the mechanics of molecular biology and gene therapy drives our political decisions, our human rights, our health care, our religious sensibility?
Taken together, ethical concerns, political showdowns, medical treatments, product development — all these things feel distant from the embryo in the cryo-tank, alive yet not alive, like T.S. Eliot’s “patient etherised upon a table.” Such a multitude of views seems out of whack with the tininess of the stem cell clump inside that microscopic entity. It’s as if our understanding grows less certain the smaller the micro-environment gets — cells, chromosomes, dna, telomeres, those tips at the ends of chromosomes that, as they shorten, signal mortality. Biotechnology grows more miniaturized, and so, too, must its inquiry and treatments, to be effective, to uncover more of the unseen.
What’s hard is making stem cells real to us, despite seeing how their recent applications, for example with Heiju’s leukemia, almost insure a cure. These cells are abstract, paradoxical, archetypal. I was told they are very hard to see in adult blood; they like to hide in bone marrow niches; they are like night watchmen, fully awake and fully asleep; they go into spontaneous division when many of our tissues or organs are damaged. They seem subservient and essential to whatever organism they inhabit. On the other hand, human beings, a farrago of cells, seem palpably enabled. We relate to ourselves only as full-fledged tissue — our skin, for example, the still-dividing richness of cellular life but at its end stage, not its beginning. We (Lewis Thomas and a few biologists like him are exceptions) relate to ourselves cellularly or genetically not at all. Not yet, at least.
Still, on the level of the infinitesimal, stem cells stir our fears of technopoly. Who will control that miniature multiplex world inside the stem cell, which has so much directive power to differentiate our entire beings and all the beings that make of us a lineage? No wonder we worry about the ethical consequences of this new medicine. We worry whether we will be manipulated by a few bio-wizards who use their language, secrecy, screening for treatment, private and federal funding, things we cannot control. Dare I say, the Mengele of genetic engineering to come.
The ethical questions we face will keep dividing, much like the cellular division that is germane to the development of all organisms. Perhaps this is natural, the way of science, that is, not to resolve questions but to keep posing them. The psychology here is especially confusing. My sense is, there won’t be a lot right or wrong to argue about with new geno-cellular medicine because what it promises is too great to deny. To deal with it, we will rely on an old axiom, that ironical faith we have in the “specialization pathways” of research — more research equals better living.
Prognoses: One or two stem cells might be extracted and stored from every person’s embryonic opening act for a late-in-life “retreading” of the body. Medically undesirable genetic traits might be fixed or eliminated by the introduction of new or different stem cells in the embryo. “Therapeutic hybrid cloning” (it’s already been done) occurs when the nucleus of my adult skin cell is combined with a cow embryo and from it a culture of fresh, unmistakably-me stem cells is coaxed into being and, thus, becomes my lifelong fix-it kit.
Consider that in the previous century, life expectancy in the industrialized nations rose on average from 47 years to 76, an incredible 62 percent increase. If equaled in our new century, people would live to be 123! It’s possible. But despite the hope, questions in my ears keep ringing like a gym teacher’s whistle. If all parents have the right to a healthy child, how do we enforce, let alone pay for, such a right? Will this medical technology, promising the renewal of organs, ensure longer life? Will that life be any better merely because it is longer? Who will get to live it? Most La Jollans? Some Chula Vistans? A handful of Tijuanans? And, finally, will we continue to anoint technological progress even as technology makes us more harried, more open to invasive treatments, and, ironically, less individually secure than we have ever been?


Like many newly married couples, Cristen and Jeffry Hays wanted to get pregnant soon after their wedding in 1992 but felt it best to wait.
They used birth control until Jeffry finished three years of chiropractic school, passed his preceptorship, and established a practice in San Diego. Then, in their mid-30s, with “it’s now or never” nagging them, they dropped their protective shields and went at it, a pleasure as often as it was a duty.
For a year, nothing happened. Something was wrong, and the Bakersfield natives suspected the problem was inside Cristen. An insulin-dependent diabetic since 12, Cristen wears an insulin pump, monitors her intake by pricking her finger and testing her blood-sugar level ten times a day, and lives at times emotionally weakened by the high maintenance her illness requires. Tests suggested that either the diabetes or scar tissue from the disease was blocking her fallopian tubes. She was ovulating regularly, but the incoming sperm couldn’t find an egg. They considered laparoscopy, a “roto-rooter,” Cristen calls it, to open up the tubes. But the operation guaranteed nothing, except another invasive procedure.
Diabetics do have healthy babies every day, Cristen tells me on a warm evening in January when she and her husband are lounging at the dining room table in drawstring shorts and cotton T-shirts at their Scripps Ranch home. Cristen is 37, athletic and fit, able to work, but weary of her daily regimen. Jeffry, a year older and a former personal trainer, possesses (literally) a hands-on grasp of anatomy as well as empathy for his wife’s condition. “Yes, [pregnancy] is doable,” he says. “But Cristen had had complications with her eyes, some stages of kidney dysfunction. Throw a pregnancy in there, throw some hormones in there, throw all that together and try to manage your blood sugar. If the blood sugars get out of control, it can wreak havoc. Some higher power was saying that this was not meant to be.” So they gave up on getting pregnant and turned to the higher power of science.

In vitro fertilization, it’s called. The now-22-year-old technique whereby conception can occur outside the body is routinely performed at seven San Diego fertility clinics. Cristen and Jeffry met Dr. David Smotrich at his Smotrich Center for Reproductive Enhancement. A soft-spoken, impartial man, as much scholar as physician, Smotrich was trained at Tel Aviv University. He told me recently, “In Israel, there’s a push for people to get pregnant.” As a “disease,” infertility is covered under Israel’s socialized medicine system, while in the United States the procedure is still elective.
In any event, Smotrich didn’t need to present the Hayses with the idea of surrogacy, that is, a carrier for the couple’s fetus who gives birth to the child and gives the child to the parents. The Hayses had already stumbled on the procedure through a friend whose sister had been a surrogate. Suddenly an idea lit up in Cristen; she thought of her older sister Candace, who had three children and who, according to Cristen, gets “pregnant so easily.” Candace wasn’t sure. She hemmed and hawed for months. Antsy, Jeffry called her one afternoon and said, “I appreciate that this is a big decision, but we have to know.” After a half-year of reading, classes, and reflection, Candace agreed.
In vitro with a surrogate requires pit-stop coordination. Candace took drugs to ready her uterus to receive the embryo; Cristen was put on Pergonal to stimulate her egg production; Jeffry kept his calendar open: He would have to arrive at the clinic to supply the sperm on the same day as implantation. Which, good trooper, that’s just what he did — running a stop sign or two on his way to the clinic bathroom when the great day finally arrived.
On Pergonal, Cristen had created 14 eggs, and Smotrich, once he’d removed them from her ovary, fertilized 10 of them. (The odds of fertilization are pretty good, what with 40,000 to 50,000 fresh motile sperm after one egg on the bottom of a petri dish.) He watched the eggs closely, “grading them subjectively,” as he says, on their number of divisions, symmetry, and clarity. He determined that 6 of the 10 were viable. Smotrich and the Hayses decided then to implant 3 in Candace and freeze the other 3 for a (possible) later cycle. Raising high the roof beams, Jeffry and Cristen’s Christmas card showed a picture of an embryo, a one-day-old, six-cell floating clover leaf in its preimplantation petri-dish exile.
Fertilization begins when the pronucleus of the male gamete disperses its material into the pronucleus of the female gamete. With in vitro, it may be necessary to surgically inject a single sperm through the egg’s membrane with a needle. Consummation occurs once 23 chromosomes of each male and female gamete are combined into a single cell, the zygote. The zygote then begins cleavage, dividing many times over the next four days. At day five, the zygote forms a blastocyst, a hollow membrane of primitive cells, some external, but more colonizing internally in a tight clump. Seen under a microscope, the round blastocyst, about as thick as a human hair, or 0.008 inch, resembles an inverted wedding ring with the diamond on the inside of the circle. That diamond is the inner cell clump, elliptically formed and pulsating with switched-on genome joy. The hope is that the blastocyst will keep enlarging and, after seven and a half days, implant its sticky outer cell mass (eventually the placenta) onto and into the uterine wall. The cells forming on the inside of the blastocyst are called stem cells, that is, the undifferentiated master cells from which all other cells in our body stem.
(It is these cells and their medical possibilities that I have come to talk with the Hayses about, though I admit to being circuitous. Stem cells have been touted, just in the last two years, as the greatest medical miracle since antibiotics, because these cells, in their blastocyst stage, have unlimited potential for treating and curing almost all diseases as well as for growing organs from scratch. I hope to discover how Cristen and Jeffry feel about this potential, which, as they know, resides within the embryos they have created, and are keeping, in vitro.)
Back at the clinic, Dr. Smotrich placed three embryos in Candace. Jeffry and Cristen knew their chances were less than 50-50, but they were hopeful. Just one or, perhaps, all three will stick. High hopes, indeed, but the rule is otherwise. The best guesstimate is that only one of ten implanted embryos stays for the full term. We’ve all heard of the exhausted mother with as many as seven embryos implanted, resulting in a multiple birth after which telethons are organized and the neighborhood volunteers in shifts to change diapers. Couples and clinics want pregnancies. That can mean upping the ante with fertility drugs and the questionable practice of putting in a dozen embryos to enhance the odds (in England the law limits the number to four). But the “success rate” of in vitro remains dicey: Only 40 percent of couples who do three cycles or more (each cycle is one implantation of embryos) will get a baby.
Dicey, indeed, for Cristen and Jeffry and Candace, now an even closer triumvirate. But, sadly, none of the three implanted; Candace’s body absorbed them. After consultation, the group decided to unthaw the other three embryos and try again. A month later, that too was a bust. It was “all downhill on the emotional roller coaster,” Cristen recalls. Either they’d start once more from scratch, meaning another $10,000 cycle and the coordinated labor of the female tag team, or quit. Cristen, a fighter, says, “I wasn’t ready to give up,” even after the second failure. Jeffry adds, “We felt the odds increase every time because the doctor learns a little bit more about what he can change to make our chances greater.”
On the third cycle, they created five embryos and Smotrich placed four in Candace. Jeffry calls it “getting more aggressive,” while Cristen acknowledges some desperation. Candace agreed that if all four, or three or two, stuck, she would carry the lot to term. The lone leftover embryo they froze. Though the Hayses and Candace knew about “selective reduction,” whereby they could reduce the number inside Candace if there were complications, in principle the three decided against it. Doing so remained hypothetical: One of the four clung to Candace’s uterus and buried itself in the lining. The embryo-cum-fetus had few problems as it grew to term. In March 1999, Jayden Marie Hays was born, pudgy and healthy, a saucer-eyed charmer who by the time I meet her at age nine months cadges me to pick her up and hold her just so she can push my tape recorder off the table.
Though Cristen and Jeffry and Candace came to a perfect end with Jayden’s birth, which is also the perfect beginning of this little girl’s life, there is another “being” or “life” left to consider. That other frozen, and as yet unused, embryo. And the Hayses have considered it.
Options for the future of frozen embryos are several. Smotrich described four: Use them again for another cycle; not use them again and instruct the clinic to thaw and discard them (couples can request a memorial service); donate them to an infertile couple; donate them to research. “Most couples recognize how difficult it is to create embryos,” he says, “so it’s unusual for them to want to discard them.” Most keep them frozen; the storage fee runs around $150 a year. (The oldest known freezer-to-birth embryo is one that was held for seven years.) Their numbers are also reduced because, according to Smotrich, there’s only a “67 percent successful thaw-rate,” which means one-third of them die.
The Hayses have decided to leave their remaining embryo frozen, for the time being. If they change their minds, they will donate it to medical research.
I ask them how they regard its “moral status.” Quickly, it seems, the joyful ending of Jayden’s conception and birth is left in the dust.
“I don’t know,” Jeffry says. “I guess I see it as — even though it’s frozen, it’s alive.”
“Can you say it’s alive?” Cristen counters. “Because it doesn’t have a heartbeat.”
Jeffry stares at me, his inquisitor. “So the question you’re raising, damn you” — he and I laugh nervously — “who are we to take this potential life’s being and donate it to science when it could live?”
“We’ll use it,” Cristen says with certainty, confiding later that she has a new surrogate picked out, her younger sister. Candace, at 40, has said no thanks to another mission.
“I’d like to think we’d use it,” Jeffry adds. “But if we don’t, our choice was not to donate to another couple to start a family but to donate to science so something could be learned from [the embryo].” His voice is a bit ethereal; Cristen is quiet. There’s a sense — and I can’t quite put my finger on it — not that the Hayses have disregarded the “rights” of this being but that thinking about the “moral status” of a five-day-old blastocyst/embryo yields no firm answer as in, “Oh, yes, it is a full legal and moral person,” or “Oh, no, we have no attachment to it.” Thinking this through for anyone, let alone the parents, while the embryo sits in the cryogenic freezer at minus 196 degrees Celsius in a liquid-nitrogen crystallized state, yields far more questions than answers. (There’s a lot of thinking-through going on these days in America, with 150,000 to 200,000 embryos in their technological purgatory. Waiting and thinking, I coulda been a contender.)
“In essence,” Jeffry says, seemingly not wanting to admit it, “we’re putting this out to pasture, we’re condemning this embryo to death.”
“It’s like organ donation,” Cristen says.
“No, it’s not,” he says. “An organ isn’t a life.”
She agrees, and adds, “Then we’re going to use it.” Jeffry laughs and reminds her that this embryo is “not a very viable one, and so I guess I’m justifying in my own mind that if we don’t use it, then we’ll donate it to science.” But deciding whether to keep it, he admits, is also a way to delay a decision about its status. “I didn’t sit down and think, ‘What if I donate this to science? Then that means I’m not allowing this embryo a chance to live?’ ” And if it’s a life — I believe he understands this but didn’t express it this way — then it’s troubling, because donating the embryo to research will mean terminating its life. “And I’m against abortion,” he says, renewing his moral quandary more than he may want to.
Then, as if to rescue Dad from the Big Muddy, Jayden is pulling herself up the rungs of the chair he’s sitting in, reaching hands up to be hoisted, to feel alive in his lap where there is no uncertainty about her.
It’s not clear that there’s a good place to end our talk, so I say it’s late and I must be getting home. Before leaving I recall that before the Hayses told me the story of Jayden’s birth, I’d asked Cristen if diabetes is hereditary. Yes, she responded. Her father and brother both have it; in fact, complications have meant eye surgery for Cristen and her father.
I looked at Jayden, chewing on a biscuit in the high chair. Does she have diabetes? I asked uncomfortably.
“We’re hoping she won’t,” said Cristen.
Driving home, I imagine Jayden one day not having a brother or sister from the lone embryo and, instead, that intended being donated to research. If Jeffry and Cristen do trade the gift of a sibling for a possible cure for a disease Jayden might inherit, I hope any of us can understand the moral dilemma they have faced.
About the time Jayden was lolling, midway through her gestation, in Candace’s uterus, James Thomson, a molecular biologist at the University of Wisconsin, was testifying to a subcommittee of the United States Senate. He was excited, in that self-possessed unexcited way scientists get, about his research using human embryonic stem cells, those cells that can only be gotten from a five-day-old blastocyst. Thomson had been one of the first U.S. scientists to remove stem cells from a human embryo. The embryo was donated by a couple, much like the Hayses, who had created more than they needed during in vitro treatment. Thomson had isolated the cells on a bed of mouse embryonic stem cells and, after eight months of growing over one trillion (that’s right, with a t), he was amazed at what his research team had accomplished, namely, maintaining a feedstock of these master cells that form the cellular paths for all human development.
Stem cells contain undifferentiated and unspecialized cellular potential and, if harvested in their youngest and purest stage, hold treatments and cures for nearly all types of disease. Harold Varmus, head of the National Institutes of Health, has said, “This research has the potential to revolutionize the practice of medicine.” Further indicative of its promise is the Patient’s Coalition for Urgent Research, which is advocating an increase in federally funded stem cell research: “No research in recent history has offered as much hope to the more than 128 million Americans suffering from debilitating and often fatal diseases.”
The list of possible cures using stem cell treatments is staggering: sickle cell anemia, Parkinson’s and other brain diseases, heart and cardiovascular diseases, certain leukemias and cancers, autoimmune diseases, osteoporosis, spinal-cord injuries, birth defects, and more. There is even a treatment proposed using stem cells to cure Cristen Hays’s disease, juvenile onset diabetes, from which one American dies every three minutes. In addition, work is proceeding with synthetic scaffolds and tissue-specific stem cells to grow cartilage, muscle, pancreas, kidney, liver, heart. Finally, genetic manipulation of stem cells may mean that many diseases will be nipped in the code and never begin.
Thomson’s experiment had to be done in a straitjacket, so to speak. The National Institutes of Health has banned the use of federal funds for any human embryonic research although the government does not forbid privately funded research. So Thomson got funding from the California-based Geron Corporation, a private biotechnology company, and built a lab only for his stem cell experiments. (Word was he bought everything new, including the electrical extension cords.) His comment at the time speaks volumes about government duplicity: “That a sensitive category of research is legal for people who are not publicly accountable but illegal for those who are accountable is just very strange.”
Thomson forged ahead, growing his bank of stem cells, then arresting their growth in the deep freeze. He testified at the senate hearing that such cells could not by themselves make an embryo. Thomson wanted the senators to hear why he feels stem cell research should require the ethical exploration and financial support of the National Institutes of Health. He said, “The current ban…for embryo research discourages the majority of the best U.S. researchers from advancing this promising area of medical research.” One month prior to his testimony, at the time of his discovery, he told the press that the mother of all cells contains “limitless” possibilities. “Our stem cells can give rise to potentially everything, and they never die.” By never dying, he meant that a stem cell’s nature is to self-renew and to differentiate: Most often it divides into two cells, one a duplicate, and another that will differentiate via further growth and division into a particular tissue. By duplicating itself, the stem cell retains its ability to supply whatever new cells the body needs. Thomson made the network news when he called the human embryonic stem cell “immortal.”
Twenty years before Thomson’s pronouncement, another biologist, Lewis Thomas, had written a short essay entitled “On Embryology,” part of his best-selling collection The Lives of the Cell. In the piece he swoons over the first test-tube baby. Thomas is enthralled with embryogenesis, the process by which cells develop into tissues and organs. He writes that from the onset, in the first “cluster of cells,” a huge array of information is “latent inside every cell in the cluster. When the stem cell for the brain emerges, it could be that the special quality of brain-ness is simply switched on. But it could as well be that everything else, every other potential property, is switched off, so that this most specialized of all cells no longer has its precursors’ option of being a thyroid or a liver or whatever, only a brain.”
What wonder fills his words — as much wonder as science. The voice of Montaigne in a junior high student firing up the Bunsen burner. “One cell is switched on,” he continues, “to become the whole trillion-cell, massive apparatus for thinking and imagining and, for that matter, being surprised. All the information needed for learning to read and write, playing the piano, arguing before senatorial subcommittees, walking across a street through traffic, or the marvelous human act of putting out one hand and leaning against a tree, is contained in that first cell. All of grammar, all syntax, all arithmetic, all music.”
How curious that Thomas foresaw James Thomson’s need to testify before a senatorial subcommittee. Such was Thomas’s gift — to be as thrilled by the mystery and meaning of life (“no one has the ghost of an idea how this works,” he noted of the stem cell’s switching-on of its duty) as he was by the explanation of it. He did say that when someone figures out that switch, Thomas himself will “charter a skywriting airplane, maybe a whole fleet of them, and send them aloft to write one great exclamation point after another, around the whole sky, until all my money runs out.”
All cells divide and grow. But when the stem cell divides, one of its daughters grows toward tissue and the other retains its full potential as a stem cell. The daughter cell that has an intended function, to make skin, for example, will grow and divide until it becomes skin tissue. Biologists call this process differentiation or specialization. The specializing skin cell divides into identical daughter cells. But these cells, as they grow, “express” more specialized genes that produce specific proteins, which can become only one type of cell, a skin cell. Like most differentiated cells, the skin cell can divide only so many times. The skin tissue must be reinvigorated by a stem cell, which like a fairy’s wand supplies the skin with new cells once the old ones wear out.
Stem cells in the one- to five-day-old embryo are called pluripotent cells because they have not yet differentiated and, thus, will generate most other cells in the body. Pluripotent cells are paper heavyweights, ready to do many duties but as yet unleashed, much like a set of first-round draft choices headed for the nfl. Once cells begin dividing toward their intended tissue, in blood, nerves, or organs, they become multipotent or adult. Some cells hold on to their “stemness” as they differentiate. The hematopoietic stem cell is an example of a multipotent stem cell, one that resides in the bone marrow, supplying the blood with new cells as well as self-renewing. Multipotent cells exist for the brain, blood, liver, skin, heart muscle, and other tissues, but not for every tissue and not for every organ. (To complete the spectrum, the totipotent cell is the first two divisions of the fertilized egg — all cells come from it; the unipotent cell can realize only one goal, a particular cell type.)
Cells are the basic element of life. Not only is their quantity of 75 trillion in one human body mind-boggling, but their quality as efficiency experts is equally astonishing. Cells are vital to the body’s metabolism, reproduction, and organ growth. The 200 cell types in our bodies do their developmental work as four basic tissue types. A tissue is the end result of cellular growth and combination. We have epithelial tissues, which form the body’s skin and line the internal organs; muscle tissues, which expand and contract; nerve tissues, which conduct electrical impulses through the nervous system; and connective tissues, which hold together various parts of the body, among them bone and cartilage. Organs are groups of tissue: the heart, for instance, is composed of all four tissues.
What powers the cells? One fuel source common to each cell is its genetic code. Our chromosomal uniqueness comes from the code, that 0.1 percent difference between us. The individual code, lying in the nucleus of every cell, is programmed to undergo, generally, about 100 years of division. The rate is uneven because some cells live longer and work harder than other cells, and some cells simply lose their reproductive ability or else remain dormant. Biologists call cell death either necrosis, from external factors like injury or disease, or apoptosis, from internal causes, like aging or the everyday cell division that insures growth and development. When cells wear out via accidental or programmed death, there’s no need to ask for whom the bell tolls.
Scientists believe generally that once an early cell stemmed toward its intended tissue — for instance, a liver cell began making liver tissue — there was no way to change (one huggable term doctors use is “to coax,” another, less friendly, is “to trick”) its direction. But at least one researcher I spoke with said that a few biologists are discovering that cells may be rerouted from one stem-direction to another.
Dr. Edward Ball, who directs the UCSD Bone Marrow and Stem Cell Transplant Program, told me of newly found cellular trade winds, much like Portuguese explorers seeking routes to the East. “In muscle there are stem cells that give rise to blood; in bone marrow you can see evidence of liver stem cells; in brain there are cells that can give rise to bone marrow. So the stemness of these cells is much more diverse than we thought.” These are, please note, evidence only of the cells’ presence and inclination. No one knows how to nudge one toward its goal. But, as Ball said, the experiment with Dolly the sheep proved that a given cell could form a whole new organism. In fact, Ian Wilmut, the British embryologist who cloned Dolly, placed adult sheep cells in an embryoniclike culture where they “thought” they were growing inside an embryo just like stem cells. He then fused one of their nuclei with an unfertilized donor egg whose original dna was removed. One hundred forty-seven days later, baa-baa-baa-baa, it worked. Genetic medicine and molecular biology haven’t been the same since.
UCSD, as pluripotent a research-intensive school as you’ll find anywhere, is bristling with stem cell inquiry. Doctors Lawrence Goldstein and Ewa Carrier, in medicine, and Bernhard Palsson, in bioengineering, oversee labs that, in their insufferable nondescript gray buildings, are at least within earshot of each other. The lab research, done largely by graduate students and technicians, centers on mouse stem cells and other applications. For example, Dr. Carrier specializes in stem cell transplants, while Dr. Palsson and his staff are recording the migration and metabolism of stem cells with some dazzling time-lapse video. Broad-shouldered labs packed with incubators, microscopes, sterilization tanks for petri dishes, and shelves sagging with colored three-ring binders are abuzz with ongoing experiments and the occasional flurry of discovery.
In Lawrence Goldstein’s lab, technician Liz Roberts is opening an incubator where she’s cultured mouse embryonic stem cells. She brings out several dishes to show Goldstein and me a succession of experiments. First, she’s grown a feeder layer of cells on which she has placed stem cells. (What I’ll be looking at are the descendants of a mouse stem cell that was removed from a blastocyst and frozen a decade ago in Canada.) Roberts, who worked with handicapped children before joining the lab, has stopped the cells’ propagation after three and a half days. She wants me to see a ragtag cluster of 32 or 64 stem cells in their near-perfect pluripotent state. She says they’re “quite happy” clustering together on the feeder bed. “If they aggregate too quickly, they start differentiating. We try to keep them in a single-cell suspension” — that is, separated — so “each cell is left to divide and form its own colony.” And to colonize is what these cells crave.
The clump of cells in the dish is what Roberts calls “an embryoid body,” not an embryo but a colony of stem cells that thinks it is making an embryo. Without the mother’s uterine environment, however, the cells can’t do it.
On this note Goldstein joins the discussion. An investigator for the Howard Hughes Medical Institute (that is, the Spruce Goose himself), Goldstein is a one-time triathlete (he blew an ankle out) who now manages a careful four miles a day. With premature gray hair and a nose like a knife, he enjoys explaining the particular intelligence of cells. “They’re confused,” Goldstein says of the cells Roberts has isolated in the dish. “They usually rely on signals from their neighbors” (other kinds of cells, growing and differentiating, around them) to proceed. And yet, they “remember” being a mouse embryo. Goldstein’s anthropomorphism feels deliberate: He insists that we compare the behavioral model of mouse stem cells to their human counterpart because gene and cell research, now reserved for mice, will begin on human embryonic stem cells, sooner than later. Those human stem cells will not be in a growing embryo. Mouse embryonic stem cells, at rest in a petri dish, “cannot become a mouse,” he says. And this, he states, is the same for our species. Biologists are “always very careful to distinguish that human stem cells [removed] from embryos are not themselves humans. They do not have the capacity to become human any more than a cell from your arm at the moment can become a human. Genetically they’re the same. It’s just that the cells in the early embryo know how to become a lot of different kinds of tissues and organs.”
With a little poking, Roberts is able to bring a few individual cells into view. “If you look at ten o’clock, you’ll see one smooth, circular cell — that’s what we like.” With her glass needle, she can pick one up or, if necessary, puncture and retrieve its dna from the nucleus. In fact, this technique is what Goldstein’s lab does regularly — genetically modify these stem cells and inject them into mouse embryos. Then they study what those cells do down the cellular line as the mouse ages.
Finally, Roberts shows me a few stem cells that have begun differentiating. These she’s cultured in another petri dish so they would mature as if they were in an embryo. At two weeks, this embryoid body is spectacular, a ball as pocked and still as a harvest moon. Roberts calls it “incredible, [like] a hollow golf ball.” The body is already beginning, in its cellular spectacle, to differentiate into the tissue properties of a mouse. But it can only go so far, lacking its uterine home. By adding certain proteins to the media, Roberts might convince the cells that they were in the brain and, thus, they might turn on their brain switches and start dreaming about cheese. But in this case, she is coaxing the cells to become heart cells and, if we’re lucky, begin beating with the recognizable rhythm of cardiac muscle tissue. Roberts says she’ll call if the cells start pulsing, but, alas, she never does.
Across the street in another crowded lab shared by Dr. Ball and Dr. Carrier, work is progressing on bone marrow and stem cell transplants in humans and on stem cell applications in the uteruses of mice. Ewa Carrier speaks in rushes of technicalities about her research, as though every treatment she hopes to administer is bursting from her at once. Today in a green jacket and black turtleneck, the Polish national has a cherubic face, brownish-red hair, and open-tap energy. Having worked with lymphoma patients at Stanford, she now devotes herself to pediatrics and prenatal transplantation with hematopoietic stem cells. Her specialty, though, is rarely done: helping children born without immune systems, commonly known as the “boy[s] in the bubble.” She has developed a fetal transplant model using stem cells that she believes will save them. Otherwise, exposed to our surroundings, they will die.
She describes her inquiry as cell, not gene, therapy because the immunodeficiency diseases she studies occur in the cell. “When you provide healthy stem cells, they will cure the disease,” she says. Cellular therapy can be combined with gene therapy. “You take stem cells, put them in a tube with a healthy gene, mix them, then put them back.” But there’s a caution: If Carrier introduces genes to provide an immune system to a child born without one, she is unsure she can control the gene transfer at the embryonic level. Even if the gene therapy works in the patient, there may be complications in the hereditary germ line of his or her offspring. Not enough is known about propagation down the genetic highway after transplantation. Thus, Carrier has agreed with the finding of the National Institutes of Health that more study needs to be done before actual gene-cell therapy in humans occurs.
Carrier’s nongenetic “in utero transplant protocol” for humans has been approved by the fda, but she has not yet performed one. She has done a similar transplant in mice, which, she says, is very difficult. “You have to expose the fetuses, which are in the uterus, transilluminate them, and [work with] a delicate microcapillary tube [like a glass pipette]. You need magnification [to] introduce the stem cell solution to each fetus. Put the fetus back, let it grow, be delivered, and study its life to see what happens.”
Children born without an immune system must be kept in a germ-free environment, the bubble, in order to live. Eight fetal stem cell transplants on such children have occurred throughout the world. One, she says, has been quite successful, with a boy surviving with a strengthened immune system now for 12 years.
Her protocol ready, Carrier’s next step is to advertise on the Internet for patients, who are quite rare. She hopes to locate a history of immunodeficiency disease in a family, preferably in a child whose mother is thinking of getting or has gotten pregnant again. If the mother is pregnant, Carrier can present her and the father with options — abort the fetus, treat the disease in utero, or wait for a postnatal transplant, which can be toxic. Treatment options are highly experimental and risky. If the couple consents to treatment, Carrier will take the hematopoietic stem cells from the father and inject a five-milliliter solution into the liver of the in utero fetus in the second trimester. Finally, she will track the fetus through birth and into childhood to see how robust an immune system the child will grow.
Jody Donahue is Carrier’s chief technician. The former ballet dancer turned stem cell researcher focuses on fetal transplantation using mouse stem cells. She shows me a photograph of an anesthetized pregnant mouse, splayed out on a cloth, her abdomen open and bulging out (like large intestines) a multifetal uterus. I count nine mouse embryos in whose livers Donahue, with microscope-glasses, injects purified stem cells. In the photo, the fetuses are entombed in their sacs. How do you know where to stick the needle? I ask. Donahue says, “Wait,” and reaches to a stand of capped glass vials, each the size of my pinkie. She hands me one. There in alcohol bob a half-dozen mouse fetuses, yellowy-white and stillborn at 12 days of gestation out of the mouse’s normal 20 days. “See that dark blotch?” It’s like the half-moon dark under a fingernail. “That’s the liver.” That’s where she injects stem cells into the living fetuses. With a healthy liver, the mouse will double its stem cell count every day until the 14th day of gestation.
Surgical candidates, these mice have thalassemia, which is an anemic disorder that occurs in mice and humans. (Thalassemia is inherited among people of Mediterranean descent much the way sickle-cell anemia, a recessive genetic disorder, is inherited by people of African descent.) Donahue and Dr. Carrier hope to discover whether stem cells can cure the disease. And so far their experiments have yielded mostly healthy mice after the transplant.
Donahue is fascinated by the potency of the stem cell. Although she cautions, “Stop me if I start to lecture,” her explanations are concise. This cell, she says, “is one that renewed itself, then stopped. It created a daughter but didn’t change itself. There’s only one cell in the body that can do this and that’s the stem cell. Their progeny create the entire system” of the body. She smiles reverently, telling me of a Japanese researcher who “lethally irradiated” a mouse (destroyed its immune system) and then transplanted only one stem cell. The mouse grew an entirely new immune system.
But how the stem cell does this from its initial divisions is, she says, “not well understood.” Researchers know pluripotent stem cells start in the yolk sac, migrate to the fetal liver, then settle in the bone marrow, becoming stromal cells. Next, they move inside the bone, “form a latticework,” and pack themselves into “little niches.” She says they both divide and rest, much less active than other cells.
In the animal vivaria, or mouse house, at UCSD, Donahue and I are joined by Dr. Phil Richtor, the campus veterinarian. It’s another hospital-like ward of shiny corridors and small sunless rooms, now smelling of rodent. Getting in takes a few more who-what-why answers than normal, since the occasional animal-rights protester has tried (and failed) to liberate these cages. Donahue untops an elaborate box and pulls out from a pile of vibrating straw what Richtor calls “your typical research mouse.” Wearing pale yellow plastic gloves, Donahue holds up a mouse who “was transplanted with stem cells from a different strain of mouse, an unmatched donor.” Her voice softens, her maternal instinct rising palpably. “She survived” the transplant, she says, “but she’s a little nervous right now. Curious, but nervous.”
One of hundreds of types of white mice, this one’s “a laboratory-specific mouse, originated, I’d say, 30 years ago, an inbred strain so that all the littermates are genetically identical.” Donahue next cups a very pregnant brown mouse, with about a dozen little sacs pushing out like Santa Claus’s bag of toys from under the skin.
What is it about the mouse that lends itself to so much prehuman research?
Humans and mice have very similar hematopoietic systems. Mice also make perfect subjects: Diseases can be bred in them that could never be bred in humans. Most of what we know about human immunology has been gathered from experiments on mice. Donahue next shows me a seven-day-old pup, sniff-snooping the air, blind as a bat. She pets, oohs and aahs, seems to love her tiny charges. Clearly, her care for mice she experiments upon is not a contradiction. It is gratifying to hear Jody Donahue and Liz Roberts mention children as the main impetus for their work, children born with diseases who may soon be aided by pre- and postnatal transplants using stem cells.
Elegantly attired Bernhard Palsson, born and raised in Iceland, “of all places,” he tells me, has an office perch on the sixth floor of the Irwin and Joan Jacobs School of Engineering building. There, he is working (like Dr. Carrier) on the hematopoietic stem cell, those cells from which our blood cells originate.
After a handshake, he directs my attention to the scientist’s equivalent of the baby’s portrait on the desk — a framed copy of an enlarged cover of the journal Blood. On the cover is a photograph of a hematopoietic fetal liver stem cell, which his lab caught in some exotic dance. Attached to the cell is a podia, a cytoplasmic extension or tubule, very narrow and extremely long. In the color-dye-enhanced photo, cell and podia look like a ball with a long tether or noodle loose in space. Some stem cells, he tells me, are 5 to 10 microns wide and send out podia 300 or 400 microns in length. “It’s like you, being 6 feet tall, reaching 200 feet away.” The photographic discovery has “caused a lot of excitement,” he says. “It is something totally new in cell biology.”
What do these podia do? “In cell biology it’s very hard to prove a cause and an effect,” Palsson admits. “I don’t know what that [podia] is — an antenna, maybe.” Cells are blind, so the extension may be like a cane, tapping down the sidewalk toward new tissue. “It may,” he continues, “be going to touch another cell, so it could be a new [kind of] cell communication. It reaches out and touches someone. Sometimes we see nodules, a ball in the membrane, moving up and down the line of the podia. Sometimes we observe the podia grab on to something and then reel it in like a fisherman reels in a line. The other cell is stuck [on the podia] to the point of attachment.”
Palsson seems comfortable with being not sure. With a degree in chemical engineering, he’s been involved in clinical trials for bone marrow transplants and stem cell research as well as developing “tech-transfer” applications, whereby academics convert their discoveries into biotech products and, they hope, profitable companies.
When asked why stem cells are so important today, Palsson responds that they are “the source from which you can derive a large number of cells to transplant or manipulate.” He notes that bone marrow is “the body’s most prolific tissue; it generates as many cells as it’s comprised of every three days. It’s unbelievable.” If you calculate such zeal over 70 years, you find bone marrow producing 500 times one’s body mass in a lifetime. Bone marrow is “driven,” he says, “by these highly prolific stem cells.”
Palsson employs the word “quiescent” as the stem cell’s main state, but, when stimulated, “They can generate tens of millions of cells. Like ticking time bombs ready to go off.” He explains how a stem cell can halve itself into identical cells; into two nonidentical specialized cells; or, a third way, asymmetrical division: one, a daughter cell, the other, a cell that will specialize. Palsson questions the putative “immortality” of the stem cell, because no one has demonstrated that they “stick around forever.” He says “their proliferative capacity…diminishes with age.” The stem cell is most productive in the fetal liver, next in the umbilical-cord blood, last in the adult. “The younger the source, the better.” And that, he says, opens all sorts of ethical questions.
One case he knows of involves parents of a child suffering from a blood disease who had another child to harvest stem cells from the umbilical-cord blood. Of course they did not dispose of the new child. But, quite purposefully, they had a second child to save the first one. Another idea, untried as yet, says Palsson, is to abort a fetus in order to harvest the fetal liver cells, which are the most “proliferative,” in order to cure a fatal disease. In yet another scenario, which he stresses no one he knows has attempted on humans, is to split up the first four stem cells (that is, after two divisions following fertilization) and grow them in four separate uteruses. (Recently such a birth was accomplished with one of four surgically divided and implanted embryonic stem cells of a monkey.)
A particular question Palsson’s lab is investigating concerns what happens to stem cells as they divide and begin to specialize or migrate to their tissue sites over time. To describe this visually on film would summon the most creative of video-savvy bioengineers. Enter Karl Francis, a former robotics operator at Pasadena’s Jet Propulsion Laboratory, who helped fly Voyager and Galileo unmanned spacecraft and has, with a Ph.D. in bioengineering, turned his ingenuity to good use in Palsson’s lab.
Francis’s time-lapse digital camera system, still and video, studies stem cell migration and division. To do so he built a large plastic box to fit around a multiwired camera and temperature-controlled system, “essentially,” he says, “an incubator around a microscope.” The media in which the stem cells grow has a bicarbonate of soda base and must be infused regularly with carbon dioxide. In order to maintain an atmosphere perfect for stem cell growth, sometimes for up to a month, Francis installed as his heat source an Oster dog dryer he got at the pet store. The resulting balm is a toasty 98.6 degrees Fahrenheit, a Tahitian climate for cellular productivity.
In a five-minute video of time-lapse and real-time tape, Francis shows me stem cell division along with the modern dance of their podia. The real-time film begins in an apparent swimming randomness of cells, and then a stem cell cleaves in two. Next, a cell shoots out a tentacle, the podia, which the deadpan Francis says, reflecting on the first time he saw it, looked to him like, “I don’t know, an octopus. Here’s a mouse stem cell,” he gets a bit animated, “and you see a lasso at the end of it, which loops back and adheres to itself.” Some podia tips come into contact with other cells, presumably to trigger a chemical reaction, then snap back, jilted or kissed. (It’s hard not to anthropomorphize cells in this microscopic rodeo.) He describes one podia as forming a “string of pearls,” while another podia breaks off from its owner. Maybe, he hypothesizes, it’s sending out “a note in a bottle.” Another podia, tugging on a cell, shows some material being transferred, like reeling in (or out) “the clothes on a clothes line.” I compliment his metaphors, though he mentions having practiced by showing this tape a dozen times. In none of what he observes can Francis say which of the dividing cells is the daughter and which is the specializing cell. Nor can he say what that specialized cell will become. But he can say that these stem cells face Everest-like climbs, which he, Palsson, and other scientists are only beginning to grok.
Not all stem cells are free from worry like those healthy tribes grown in Bernhard Palsson’s lab. Some stem cells can be diseased or can carry an illness, sometimes for generations. Leukemia, or cancer of the blood, is believed to be caused by a mutation in a hematopoietic stem cell residing in the bone marrow. Like a dormant cancer cell, this blood stem cell may or may not become active within a person’s lifetime. However, if a genetically diseased stem cell switches on, the cell will divide and send out progeny with the same characteristics, in effect, cloning itself as leukemic cells. The worst is, anyone can develop an acute leukemia, at any age and without warning. Before current treatments, such a disease killed more than 90 percent of its victims.
No one knows this better than Heiju, a woman of 33, born and raised in Taiwan and now living in San Diego. (Heiju requested I use only her given name, which is Chinese.) In May 1999, Heiju and her husband were trimming a rubber tree in their yard one weekend, no overly physical activity. That evening Heiju noticed her hands were bruised. She asked her husband whether he’d gotten any bruises; he said he had one or two. The second day, she had more bruises and swollen glands. She also noticed on her leg “red dots under the skin,” then discovered “bloodlike lines” underneath her eyes. There was no pain, only these persistent symptoms.
On Monday Heiju went to work. She felt fluey, but otherwise normal. Soon she suspected the bruising was too strange not to be serious, so she drove herself to a Mira Mesa clinic, where she was told to go to an emergency room. There, a doctor said he wasn’t sure what disease she’d contracted, but she needed urgent care. Admitted to UCSD Medical Center in Hillcrest, she learned from an oncologist that she had leukemia. A few blood tests later they diagnosed it as acute lymphoblastic leukemia. Her white cell count was so high that it kept the red cells from functioning. Her platelets were severely curtailed: Without platelets clotting the blood, she might bleed to death; with too few red cells, she could become anemic; without oxygen or nutrition being carried to the tissues and organs — the purpose of red cells — she could not live. The doctors began chemotherapy at once, to boost the red cells and lower the whites.
Had anyone in her family had leukemia?
Heiju tells me, over lunch recently at the Hong Kong Chef, “none that we know of.” Her great-great-grandfather came from Fujian province on mainland China, one family branch she and her mother have not kept in contact with. Had that man had leukemia, say a century ago, he would probably have bled to death. Heiju may have acquired the disease, but she says the doctors can’t explain how. At first she understood the illness, but now, thinking back, she says confidently, “I had no idea of the depth of the disease.”
Her chemo treatments progressed for a month. She reports feeling “spacey,” trying to focus while she and her husband searched Internet reference sites to learn about their options and her survivability. The latter was not good. One source reported only 20 to 30 percent odds of pushing the leukemia into remission. Heiju says she didn’t panic or suffer major depression; she studied, read, asked questions. In the process, though, she learned so much about leukemia that she ping-ponged between feeling “out of control” and certain she’d survive. Quickly she found her mantra: “I know I have a strong will to live. I know there is a reason for me to continue living. All I have to do is start planning” for one of the treatment options.
At this point Heiju’s care was transferred from Hillcrest to UCSD’s Thornton Hospital where Dr. Ewa Carrier arrived on the scene. Carrier told Heiju she could stay on the chemo for a year and a half, with injections every month. The survival rate was 30 percent. Another possibility was a stem cell transplant. It would require passing a number of “eligibility” criteria — the stage of the disease, the sex and age of the candidate, the availability of a donor. Once deemed eligible for a transplant by Carrier and a team of doctors, Heiju was buoyed, in part, because she feared she couldn’t endure a year and a half of chemo. But, even with a transplant, complications might arise: permanent damage to the liver and the lung, the macabre-sounding graft-versus-host disease, where rejection of the new cells can occur. The survival rate for the stem cell treatment, however, doubled that of the chemo. Heiju wanted that chance.
She didn’t have to look far for a donor. One of Heiju’s three sisters in Taiwan volunteered to be tested. When the call came that her sister was a match, Heiju was only half-pleased. She had one more treatment, perhaps the most difficult — irradiating the leukemic cells in her body. She was bombarded with radiation and an equal assault of chemo, which, she says, “killed everything that you can possibly see [in the blood]. My white cells actually dropped to zero.” This was the “condition,” albeit it severely weakened, the doctors wanted — total decimation of the leukemic whites. Now she was ready for the stem cells.
Heiju’s sister and mother flew in from Taiwan, and the sister, no sooner than she was off the plane, had to endure apheresis, or blood collection. This meant drawing blood via one catheter out of her right arm, passing it through a device that filtered out the stem cells, then pumping the blood back through another catheter for its return to her left arm. Heiju’s sister underwent blood culling for four days, some days being drained and replenished for up to six hours.
Finally, Heiju got the full weight of stem cells from eight packets of blood, much like a transfusion. She felt dizzy as a chemical in the thawed stem cell solution filled her lungs, and, for 15 seconds, she got “less and less air [and] my face got hotter and redder.” But the vertigo stopped and, within 20 minutes, the transplant was done, a far easier regimen than the radiation and chemo treatments that had prepared her. In all, four months had passed between the appearance of the bruises and the transplant. Two weeks later Heiju was out of the hospital and has been recuperating steadily without any side effects. When we have lunch in early February, she is quite healthy, lively, at times zestful. She’s back working (in computer graphics) from her home.
I ask if she and her sister (who now share the sister’s blood type) are closer. “It changed my perspective on life,” Heiju says. At a stem cell transplant support group soon after the operation, she says she was able to testify to others about how much she now values “family relationships. I feel so much closer to my mother and my sister. Life in general is easier. I used to be upset by petty things. Not anymore. And most of all, I feel like I’m three years younger.”
We share a laugh, after which I remark that Heiju probably feels rejuvenated because she swiped all those good stem cells from her little sister.
She says that’s true. But her sister felt no physical complications from the apheresis. “Once you donate your stem cells,” Heiju says, “20 or 30 minutes later you’ve got them all back.” Those rear guards who hide in their bone marrow niches know what has happened and quickly — as is their nature — self-renew.
Dr. Gail Naughton is the president of Advanced Tissue Sciences, a biotech company of 200 employees that sits across from the golf course on North Torrey Pines Road. In the 15 years since she began the business with her husband (they are now divorced), she has grown human skin and other tissue types, mostly to aid burn victims. So far she has avoided using stem cells. She’s still not comfortable with it because, as she tells me in a small conference room (she is dressed in a red pantsuit with pearls and a black turtleneck), “Society doesn’t understand how to deal with stem cells” yet. She knows the universities haven’t researched and tested these cells nearly enough. In fact, she predicts, “Embryonic stem cells are years and hundreds of millions of dollars” from their highest rung, growing organs. Still, she’d like nothing better than to be making liver with human stem cells. “I think,” she leans forward, her large brown eyes very serious, “embryonic stem cells will be the key to guaranteeing every person who needs an organ can get one.
“If I wanted to grow a liver today, can I grow one? Yes.” Naughton is confident, like a betting woman putting her money on a favored filly at Del Mar. I hold out my hands to mime (fish-story caricature) the size of a liver: What? about 16 inches? “Well,” she counters, “I can’t grow a whole liver. But I can grow enough to help somebody with an enzymatic deficiency.” The possibility enthuses her words. “We know how to grow liver, we know [how] to keep it alive outside the body for months, absolutely functional, making all the right proteins, all the right enzymes, and liver’s a very complicated organ.” (In what may be science fiction, a team of researchers at a recent Toronto conference set themselves the goal of growing an entire human heart from scratch within ten years.)
“If you give me an embryonic stem cell,” Naughton continues, “and tell me how to direct it into a hepatocyte [a liver cell] chemically,” she can grow a liver. Scientists, she says, will look at the genetic code and determine what type of tissue this stem cell will stem toward. Once they know this — turn the switch on — then biologists can create the host environment that “mimics” conditions that cells recognize. Biochemical trickery.
Naughton says Advanced Tissue forgoes using embryonic stem cells because the company is “product focused.” The cells they do use to make skin and cartilage come from donated foreskin fibroblasts, after routine circumcisions. Fibroblast is made not of stem cells but of specialized cells that make connective tissue. This is, Naughton says, “young healthy tissue” whose mother and child donors, once they have consented to the foreskin donation, are tested “extensively” for viruses and diseases. This tissue is good, Naughton insists, because it “always comes from the same age, same sex, same anatomical location, [minimizing] the difference from one starting material to another. It helps us make a uniform product. It also has huge expansion potential.” In the company’s dozen cell banks, their present stash will take them “through decades of production.”
I get an idea how huge an expansion it is from a tour of their facilities. Rob Sorenson, director of manufacturing operations, lets me peer through windows at sterile areas watched over by technicians in head-to-toe gowns, cycling and recycling nutrients in order to keep the growing skin tissues alive in their two main products — Dermagraft, to treat diabetic foot ulcers, and Transcyte, to treat burns. One itsy piece of foreskin, he says, can, through eight cycles of cultured division or some five million scaffolded cells later, cover six football fields.
At last it’s time for me to touch some advanced living tissue. I’m escorted, wearing a nylon lab coat, into Twana Davisson’s lab, where she is growing cartilage. An under-30 African-American woman working on her Ph.D. in cell biology at UCSD, she is making human, equine, and bovine “constructs,” that is, cartilage tissue that can be shaped for animal and human transplants. For cartilage in large animals and humans, she says, the major similarity is their “weight-bearing,” which horse, cow, and human put on this small but virile substance.
“Tomorrow,” she says, “I’m getting in cow knees. We’ll take the cartilage off the bone, digest it down, and take the cells out. Then we’ll passage [divide] the cells and seed them onto pieces of felt.” Compute passage at Advanced Tissue like this: 100 cells, grown in roller bottles, become in a few days 1,000,000 cells; remove them and divide them into groups of 100 and grow those 100 again to 1,000,000; that’s a passage.
“We grow them in an incubator for weeks at a time,” Davisson says, “and they come out looking like — ” She points to a pint vial of liquid, where a little frosty white chip of human cartilage floats. “Like this,” she says nonchalantly. She tells me, as I don plastic gloves, not to inhale the Formalin, an asphyxiant that, breathed in, will affect my brain. I avert my face; the hard patch of goo is laid in my open hand. This cartilage — like most everyone, I’ve never handled live cartilage before — feels otherworldly, a sort of bumptious, dense plastic, not so much alive as gelatinously rigid. Certainly not pulsing with life. I test its tensile strength and, oops, it breaks in two. Davisson retrieves it, saying not to worry, she can grow more, although I wonder if I’ve just ripped up something destined for Ryan Leaf’s throwing arm.
Next, Davisson shows me a flask in which cartilage cells will, in a petri-dish media solution, proliferate. The medium is a red Kool-Aid–like liquid, nutrients that keep the cells supplied with food. This is one of the most interesting aspects of tissue engineering — the nutritional concentrate that mimics the body’s vicinity, in this case cartilage, where the cells grow. All these cells “know” is that the medium is providing sufficient nutrients to sustain them. Under the microscope, at 40-power magnification, I can see the colonies of cells, the chondrocytes, like curled eyelash-tip ends clustered together in small lumps of division: two, four, six. Davisson says that these “cobblestone” clusters “will become confluent, and there will be cells everywhere.” Once they divide into millions, Davisson will lay them onto a scaffold, a three-dimensional polymer, where the cells spread out and connect with each other, creating a matrix protein. The scaffold is biodegradable. Once the chondrocytes colonize the space — that is, fill the scaffold — they stop dividing. Then the scaffold dissolves. Presto, in its place is three-dimensional tissue.
Naughton sees a rosy future for building organs with embryonic stem cells once geneticists learn how to switch the cells’ codes on and off. Roger Pedersen, a biologist at the University of California, San Francisco, calls this switching a “language of signals and receptors,” the signals coming from chemicals that secrete into the cell’s neighbors and the home-grown receptors that hear the signals. “We know the semantics,” Pedersen writes in Scientific American, “but we don’t understand them because we can’t eavesdrop on the embryo very well, where this intimate conversation is going on.” Eventually Naughton will be able, she says, to coax stem cells “into liver cells, into neurons, into pancreas. We’ll be able to make those organs cost-effectively and safely because this one cell bank [of human embryonic stem cells] will give rise to all of it. That’s what you will see this decade.”
Preempting the competition, Advanced Tissue already owns a patent on creating tissue from what are called mesenchymal stem cells. These are the master cells from which fibroblasts and other connective tissue differentiate. Naughton says, with research on the “next level” of mesenchymal stem cells, her company will prove “how quickly products can be brought to market.” She believes “when science gives us answers about embryonic stem cells,” Advanced Tissue will be — ready, set, go — in the business of “making new organs.”
Two things are clear from discussions I’ve had with doctors and patients about stem cells. One, the cells’ potential is astronomical, and two, such potential is weighed down by the following choices: Do we or do we not derive, do we or do we not use, stem cells from aborted fetuses or donated embryos after in vitro treatments? (Deriving and using adult stem cells to treat leukemia poses no problem, as long as there’s an adult donor.) No one wants to make an embryo, that is, make “life,” only to derive its stem cells, then discard the embryo. And yet most people support the medical and research use of an embryo and its stem cells, if it is going to be discarded. An embryo’s “right” is a difficult nut to crack because only the early-stage embryo contains the most pluripotent of stem cells. Nothing seems more apt than Roger Rosenblatt’s labeling the embryo, in his book on abortion, Life Itself, “an entity of uncertainty.”
Derivation versus use drives the way we talk about embryos and stem cells. For example, what do we mean by the idea of an “excess” embryo? Do we even call one an “excess”? Can we even talk about an embryo — think of Jeffry and Cristen’s indecision about their embryo’s physical and moral status — as having given its “life” to science?
When I ask UCSD investigator Lawrence Goldstein what happens to the embryo after the stem cells are removed, he says he would “look at [the question] differently. During the derivation of embryonic stem cells from a blastocyst, they are derived from blastocysts that are destined for discard anyway,” his final word pinging. These are “excess embryos” from fertility clinics “beyond the need of the donor parents. The act of taking the stem cells has not changed the ultimate fate of those embryos.” Which means — I will say what I think needs stating — the embryos die.
Goldstein then topsy-turvies my question. “Would it be possible to remove the stem cells from an embryo and have that embryo remain viable? I would argue that it’s completely unethical even to do the experiment.” His distinction is this: One does not manipulate embryos that are destined to be implanted in women. But one can do research on embryos that are “in excess of clinical use,” a definition Goldstein feels most comfortable with. He wants me to know that he has friends who are anti-abortion and who also believe “it unethical not to use the tissue left” after any fetal discard. “In that sense,” he says, “it’s the same as an auto accident. Nobody wants an auto accident for organ donation. We would not go out and terminate people for organs. But if it happens, then we should take advantage of that in some ethical way.”
David Smotrich says that for patients the decision to freeze an embryo is as “emotionally difficult” as it is to thaw it out, for donation or discard. Smotrich wishes the public, too often incited by abortion politics, would be more sensitive about the phrase “in excess of clinical need.” He cites the recent concerted move by in vitro clinics in England to notify patients who had embryos still on ice and were not paying for their storage. After a massive get-out-the-word campaign, the clinics thawed out all the unclaimed embryos. In England, he says, the outcry was nearly inaudible. But in the United States such a move would create a “tremendous uproar,” perhaps inciting street fights and re-igniting the abortion war. Indeed, who would march on behalf of destroying embryos? Smotrich admits to having difficulty saying at the embryo stage, before implantation, that it is “life,” but he does “respect the fact that it [has] potential for life.” His hoped-for sensitivity reminds me that Americans’ view of “excess” can never be clear-cut, since the antiabortion wing has concluded that fetal rights exist at the moment of physical conception, in or out of the womb.
Ewa Carrier describes her research as misunderstood, especially where the fear of abortion struggles with the need for embryonic stem cells. To develop a plan, Carrier spoke with a French physician, Dr. Touraine, who advocated the creation of a fetal-liver bank in which, postabortion, small “chunk[s] of fetal liver” would be frozen. To help his countrymen understand why, Touraine published a book describing the fate of immunodeficient children who might be cured by stem cell transplant using these livers. Carrier says he “activated” the public to support him. The French Assembly followed and now regulates the collection of fetal livers.
That happened in France, Carrier remarks, a “very progressive country.” In the United States, it’s much different — lack of regulations accompanies political and religious opposition. She says people here fear her procedure “will promote abortion.” If there’s a private bank, people will, so goes the claim, provide aborted fetuses to make money.
Still, Carrier recognizes the difference between “research” abortions (which some have dubbed “embryo commodification”) and “necessary” abortions for severely diseased fetuses. “People have the option of abortion when they detect a disease prenatally. Prenatal diagnosis is the standard of care right now. What I would like to do is provide the option for treatments [on the fetus itself] so they don’t need to abort.”
Carrier speculates that the Catholic Church’s greatest fear is abortions for science. She says Catholics believe that if “you start terminating life, you may go on to terminate adults. With children who watch lots of violence on television, after some time they think that violence is just part of life. They get used to it. The threshold goes down. The Church has concerns I can respect. [But] abortion is different than therapeutic [surgery]. I have no problem with this, being Catholic myself.”
Congressman Brian Bilbray, a pro-choice Catholic, worries also about confusing abortion politics with the regulated, therapeutic use of stem cells. Bilbray supports stem cell research. In a recent interview at his Mission Valley office, he told me that he believes strongly in the benefits of donation after his three-month-old son died in 1984 of sudden infant death syndrome. Bilbray says he and his wife “felt a moral obligation that [our] baby’s death could have helped another baby.” At the time, they wanted to offer the child’s organs for transplantation, but the option wasn’t possible. What was possible for Bilbray was to support, with moral authority and political advocacy, the “good” to come of research and transplants.
He thinks that when sperm hits egg there is no “full legal person,” but there is a “moral person. From my theological point of view, life is created at conception. That is not identified as a legal person.” If the embryo is a legal person, he says, then “legally there isn’t any way to address it. Fertility clinics would be outlawed. If you have ten fertilized eggs, you have ten persons. What do you do with the other nine that are not being used? There is no way legally for our society to address that. If the fertilized egg is not going to be used, then you have a moral obligation that there’s as much beneficial use of those fertilized eggs as possible.”
Abortion politics and emotionalism, says Bilbray, go hand in hand. The main problem with such politics is that people use “the emotion of the abortion issue for other agendas.” He doesn’t believe that stem cell research, the creation of excess in vitro embryos, fantasies about “embryo farming” and “bioslavery,” will encourage abortions. Instead, these things will promote “fearmongering. The emotionalism played for political reasons…doesn’t scare me. We need ethical standards. I have no problem with saying there shouldn’t be the creation of life or the destruction of life. I also believe that if there is going to be a loss of life, there should be the maximum benefit made from that life. That life should mean as much as possible.”
I ask about Washington’s role in all this. He says “as usual” he’s wary of governmental intrusion into private family decisions. “The well-intentioned insensitive big government walking in to help many times creates more problems than it solves.” He says it may be politically advantageous for him to say that “this [research] is a threat to the parents’ right to decide. But I think we have a responsibility to make sure that federal funds are utilized appropriately. Some believe that means no federal funds involved in stem cell research. I disagree. It means we set up appropriate moral guidelines to make sure that the federal funds are not used to abuse the privilege of the research.”
On cloning or on stem cells, he says, both are “a great boon to mankind.” He hopes we use San Diego’s “brain trust” at UCSD and in the biotech firms of Sorrento Valley to develop stem cell therapies. (Incidentally, I hoped to but did not find human embryonic stem cell experimentation going on locally; only the brave, the few, and the privately funded elsewhere are involved.) Bilbray disagrees with his Republican colleague Rep. Jay Dickey of Arkansas, an antiabortion antagonist to stem cell research. Dickey says embryos have “the same moral status as a live human baby.” While Bilbray is in step with the House Republican majority on some abortion issues, he says, “I think I stand where the average person stands on this one.” His position may soon be vindicated when guidelines recommending federal funding for human embryonic research are approved by the National Institutes of Health. The battle may begin anew, for Dickey and his House cohorts, some 70 in all, are vowing to fight the National Institutes of Health and ban embryonic stem cell research altogether.
Some parting observations.
Lawrence Hinman, ethics professor and head of the Values Institute at the University of San Diego, joined me one day to discuss stem cell research. Perhaps his most valuable point was this: We are facing such difficult bioethical issues today because new technologies, which came about entirely from our tinkering, have brought us choices we would have never had to make. The fact that in vitro embryos exist, in the hundreds of thousands, coupled with the fact that we will use their stem cells, is indicative that technology, not science and surely not ethics, is running our lives. “The presence of certain technologies,” Hinman told me, “creates a pressure to employ the technology.
“Let’s say that you could choose your children’s eye color,” he suggested. “If it became technologically feasible and affordable, then wouldn’t that establish some pressure on prospective parents to choose it? If as parents we are short in stature, and they discover the switch for tallness, then look at the ethical dilemma. Should we turn the switch on so as to insure tallness, knowing that models and athletes in our society have, supposedly, better lives? Or should we turn the switch off and insure shortness so the child will be like us?” Is this a problem that humans should even be contemplating, Hinman wondered, or is this a technologically imposed dilemma, a purely manufactured construct that suddenly, like it or not, we have to answer?
Developing a Holy Grail of stem cell treatments is no different. Any breakthrough in its fast-track technology will create the pressure to employ that technology and leave us with new ethical conundrums, perhaps at the glad tradeoff of eradicating our most virulent diseases. But the question remains, will we be able to adapt to a world in which the mechanics of molecular biology and gene therapy drives our political decisions, our human rights, our health care, our religious sensibility?
Taken together, ethical concerns, political showdowns, medical treatments, product development — all these things feel distant from the embryo in the cryo-tank, alive yet not alive, like T.S. Eliot’s “patient etherised upon a table.” Such a multitude of views seems out of whack with the tininess of the stem cell clump inside that microscopic entity. It’s as if our understanding grows less certain the smaller the micro-environment gets — cells, chromosomes, dna, telomeres, those tips at the ends of chromosomes that, as they shorten, signal mortality. Biotechnology grows more miniaturized, and so, too, must its inquiry and treatments, to be effective, to uncover more of the unseen.
What’s hard is making stem cells real to us, despite seeing how their recent applications, for example with Heiju’s leukemia, almost insure a cure. These cells are abstract, paradoxical, archetypal. I was told they are very hard to see in adult blood; they like to hide in bone marrow niches; they are like night watchmen, fully awake and fully asleep; they go into spontaneous division when many of our tissues or organs are damaged. They seem subservient and essential to whatever organism they inhabit. On the other hand, human beings, a farrago of cells, seem palpably enabled. We relate to ourselves only as full-fledged tissue — our skin, for example, the still-dividing richness of cellular life but at its end stage, not its beginning. We (Lewis Thomas and a few biologists like him are exceptions) relate to ourselves cellularly or genetically not at all. Not yet, at least.
Still, on the level of the infinitesimal, stem cells stir our fears of technopoly. Who will control that miniature multiplex world inside the stem cell, which has so much directive power to differentiate our entire beings and all the beings that make of us a lineage? No wonder we worry about the ethical consequences of this new medicine. We worry whether we will be manipulated by a few bio-wizards who use their language, secrecy, screening for treatment, private and federal funding, things we cannot control. Dare I say, the Mengele of genetic engineering to come.
The ethical questions we face will keep dividing, much like the cellular division that is germane to the development of all organisms. Perhaps this is natural, the way of science, that is, not to resolve questions but to keep posing them. The psychology here is especially confusing. My sense is, there won’t be a lot right or wrong to argue about with new geno-cellular medicine because what it promises is too great to deny. To deal with it, we will rely on an old axiom, that ironical faith we have in the “specialization pathways” of research — more research equals better living.
Prognoses: One or two stem cells might be extracted and stored from every person’s embryonic opening act for a late-in-life “retreading” of the body. Medically undesirable genetic traits might be fixed or eliminated by the introduction of new or different stem cells in the embryo. “Therapeutic hybrid cloning” (it’s already been done) occurs when the nucleus of my adult skin cell is combined with a cow embryo and from it a culture of fresh, unmistakably-me stem cells is coaxed into being and, thus, becomes my lifelong fix-it kit.
Consider that in the previous century, life expectancy in the industrialized nations rose on average from 47 years to 76, an incredible 62 percent increase. If equaled in our new century, people would live to be 123! It’s possible. But despite the hope, questions in my ears keep ringing like a gym teacher’s whistle. If all parents have the right to a healthy child, how do we enforce, let alone pay for, such a right? Will this medical technology, promising the renewal of organs, ensure longer life? Will that life be any better merely because it is longer? Who will get to live it? Most La Jollans? Some Chula Vistans? A handful of Tijuanans? And, finally, will we continue to anoint technological progress even as technology makes us more harried, more open to invasive treatments, and, ironically, less individually secure than we have ever been?
Comments