 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
One afternoon about four years ago, my brother John called me during office hours. I had finished my family practice residency about six months before and was just starting my own practice in Berkeley, California. I do not remember if he wanted advice or was just relaying information. He had been dating Laura, a graceful, reddish-brown-haired woman in her mid-30s for over four years.
“Laura went to see a neurologist recently,” he told me in a tone of both amusement and concern, not knowing which was appropriate. Several weeks previously, she had been driving home on the Bay Bridge from San Francisco to Oakland when she noticed a powerful odor without any apparent source that lasted for several minutes before resolving. She had several similar episodes in succeeding days and therefore made an appointment with her family physician. He subsequently referred her to the neurologist.
As a physician, I get to listen to all kinds of complaints and stories, most of which do not frighten me because they do not suggest a serious problem. Statements such as “The bottom of my foot hurts when I first get up to walk in the morning" or “I’ve had this cough for over a week now” do not ruin my day. Often, the context makes a big difference. “I have recurring pain in the center of my chest" arming from a 20-year-old nonsmoking art major who has just begun lifting weights doesn’t concern me as would the same complaint coming from a 48-year-old two-pack-a-day smoker whose father and two brothers died in their 40s of heart attacks.
Sometimes I hear a story to which my mind responds, “Oh, shit!” The first one I can remember happened in August 1989, about six weeks after my graduation from UCSD School of Medicine, during my first emergency room rotation as an intern at the Maine Dartmouth Family Practice Residency. As usual, I grabbed the clipboard of my next patient and strolled into the treatment room, where I found an adorable five-year-old, potbellied blond boy and his parents, each about 30 years old and oblivious to what would be the outcome of that day’s visit.
As the boy smiled up at me, his mother explained his recent troubles. “For the past several weeks, he urinates all the time, even during the night. His thirst seems unquenchable, and he has a voracious appetite.” I could have stopped right there; this was a classic presentation of new-onset juvenile diabetes. His blood sugar was 835 (normal would have been about 100).
Before I could say anything about his diagnosis, he offered without prompting, “I hate shots.” Well, kiddo, welcome to your worst nightmare; hospitalization, relentless venous punctures for blood samples, strict dietary restrictions, and multiple shots of insulin every day for the rest of your life.
Laura’s was also an “Oh, shit!” story, though I didn’t dare say that to my brother. She was describing olfactory seizures. Seizures are random uncontrolled electrical discharges within the brain that result in a variety of syndromes. The most common syndrome we think about when we hear the term seizure (or epilepsy, the illness of having seizures) is grand mal epilepsy, where a person loses consciousness and has frenetic, uncontrollable movements of the arms and legs. Laura’s random electrical discharges affected the area of the brain that processes the sensory input from the nose, so she experienced these events as powerful odors. They did not involve her motor cortex, which sends the messages that affect muscular activity, so she did not have any problems controlling her movements. Nor did she suffer loss of consciousness, the criterion we use to separate “partial” from “complex” seizures.
The bad news for Laura wasn’t that she was having seizures, although seizures are potentially dangerous events. Many people have seizures, and usually we can stop them with medication. The context was the bigger issue; she was a healthy woman who had never seized before. Her story immediately brought to my mind a 51-year-old woman whom I had seen as a resident three years before in the emergency room. As she was watching her television that afternoon, the TV began to move away from her, as though it was fading into a remote tunnel. Like Laura, she was having a temporal lobe seizure, but hers affected her vision. Like Laura, she had never had a seizure before. Like Laura, this meant almost certainly that she had a brain tumor.
I told John that I did not like the sound of this; Laura had something in her brain that did not belong there. I said it would not do us any good to speculate until she had her MRI scan, which I knew the neurologist would recommend. The 51-year-old woman from my residency days had a benign tumor, a meningioma (derived from the meninges, the thin layer that surrounds the brain and spinal cord) the size of an orange, which a neurosurgeon removed without touching the rest of her brain. We could still hope that Laura would be as fortunate. A couple of days later, John notified me that she would have the MRI that Saturday and asked if I could go. I had call duty that day, which meant I might be working at the time of the scan, but 1 would try to be there.
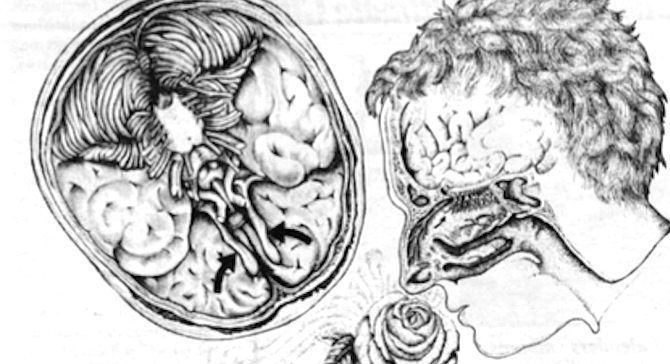
About ten minutes after the technician had finished, I arrived and caught a glimpse of Laura’s MRI scan through the reception window. MRI, or magnetic resonance imaging, is a technique that takes pictures of the insides of our bodies with such clarity that an MRI scan looks like a large black-and-white cross-sectional photograph of the targeted body area. Each of the intricate structures of the brain, every fold (“sulcus"), fluid-filled space (“ventricle”), and cortical layer, shows in near-perfect anatomical detail. Benign tumors have symmetrical shapes, uniform composition, and sharp, discrete borders, which were what I had hoped to see.
Instead my eyes met an ugly, dense, swirling white mass that looked like an expanding galaxy invading her temporal lobe, with linear white rays streaking outward from the center into the surrounding cortex. It could have been a diagram of a small white explosion. Malignant tumors such as this gliocytoma grow rapidly and therefore often cause symptoms of increasing pressure inside the head (“intracranial pressure”), including headaches, vision changes, and altered levels of consciousness (drowsiness, lethargy). They also show “mass effect” on the MRI scan, pushing brain tissue into areas of lesser density, such as the fluid-filled ventricles, which show up black on the scan in contrast to the white and gray cortical structures. Laura’s scan showed compression of one of her ventricles.
I walked through the door separating the patient waiting area from the computer controlling the MRI scanner. Todd, the radiologist on duty that Saturday, looked up at me. Being new in town at the time, I introduced myself to him and explained that Laura was a close friend of the family.
We both realized we were dealing with an otherwise healthy young woman with a brain cancer that looked incurable. The cancer was invading the surrounding brain tissue so aggressively that it would be impossible to try to remove the whole thing without disabling vital cognitive structures. “Obviously, this is a terribly abnormal scan,” Todd began. “This puts you in an awkward position, because it will be at least two days before she can consult a neurosurgeon to get the answers she needs once she learns her diagnosis. It would not be fair to tell her the results now without access to that information.”
As a rule, I don't lie to patients. Ever. But when a physician gives terrible news to a patient, within a few minutes the patient wants to know what will happen next and what his chances of survival are, and neither Todd nor I could give reliable answers to those questions. This is the one situation I can recall in my career that I did lie. I thought it was better to tell Laura that I didn’t see the results than tell her she had a deadly-looking brain cancer on a Saturday and make her wait for 48 hours. Because of that experience, I don’t recommend getting important tests on weekends, even if it is more convenient
Laura saw a local neurosurgeon the next week, and he confirmed what we already knew; he couldn't operate on the tumor and therefore could not cure it. I found this out when John called me later in the week and asked if there was anything I could do. Had I been living almost anywhere except the San Francisco Bay Area, the answer would have been no.
Up until that time, I had heard of but never dealt with Dr. Charlie Wilson, Chief of Neurosurgery at UC San Francisco. He was more famous than any physician to whom I had ever spoken in my life, and I did not have any idea whether he would accept a referral from me. But after I left a message, he called me back, took the referral with courtesy and gratitude, and arranged to see Laura the following week.
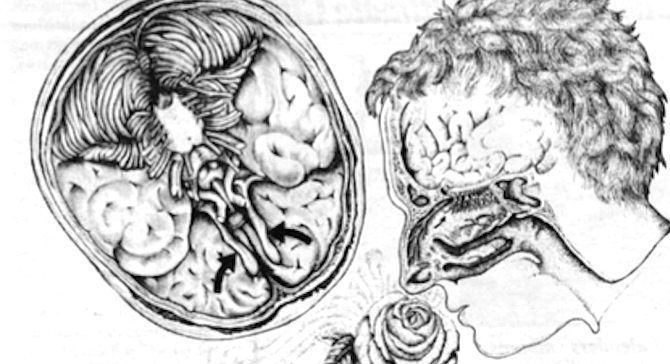
Dr. Wilson had recently pioneered a surgical technique for which he believed Laura would bean excellent candidate. Under local anesthesia with the patient awake, he stimulates each area of the brain he wants to remove to see whether he is disturbing vital processes. He can then make a precise map of where he can cut and where he cannot, allowing him to be much more aggressive in his attempts to resect as much of the cancer as possible without creating disability. When the only other option is certain death, brain surgery while awake makes sense.
After surgery, Laura underwent radiation treatments aimed at eliminating any residual tumor. Radiation and chemotherapy treatments work because they selectively damage the most rapidly dividing cells in the treated area, which are often the cancer cells. Of course, many normal cells in the body are also dividing during the period of treatment, so these cells die as well. This is why these treatments cause, among other things, hair loss and anemia, because hair cells and blood cells are among the most frequently produced and rapidly turned-over cells in the body.
So Laura lost much of her hair from the radiation treatments. The next time I saw her, four months after her surgery, she was sporting a buzz cut that almost covered the circular scalp scar surrounding a slight indentation in the side of her head Dr. Wilson had removed almost all of the tumor, something 1 can barely believe to this day. The day I saw her, Laura had just gone for a follow-up MRI scan that did not show any evidence of residual tumor. She had resumed full-time work and recreational dancing and was feeling well.
She then did something that caught me off guard; she thanked me. All I had done was make one phone call, I reminded her. I was just thrilled that she was doing so well. But she pointed out that her primary care physician had not suggested she do anything beyond consulting the local neurosurgeon, an experienced, talented, and highly respected individual, who had given her the initial dismal news.
One of the realities of primary care is that most of what we do goes unnoticed For example, we have to treat 65 people with high cholesterol to prevent one heart attack. But in this one instance, I did something very easy and received a tremendous reward. Three and a half years later, Laura’s MRI still shows no evidence of tumor. That’s why I do this.

One afternoon about four years ago, my brother John called me during office hours. I had finished my family practice residency about six months before and was just starting my own practice in Berkeley, California. I do not remember if he wanted advice or was just relaying information. He had been dating Laura, a graceful, reddish-brown-haired woman in her mid-30s for over four years.
“Laura went to see a neurologist recently,” he told me in a tone of both amusement and concern, not knowing which was appropriate. Several weeks previously, she had been driving home on the Bay Bridge from San Francisco to Oakland when she noticed a powerful odor without any apparent source that lasted for several minutes before resolving. She had several similar episodes in succeeding days and therefore made an appointment with her family physician. He subsequently referred her to the neurologist.
As a physician, I get to listen to all kinds of complaints and stories, most of which do not frighten me because they do not suggest a serious problem. Statements such as “The bottom of my foot hurts when I first get up to walk in the morning" or “I’ve had this cough for over a week now” do not ruin my day. Often, the context makes a big difference. “I have recurring pain in the center of my chest" arming from a 20-year-old nonsmoking art major who has just begun lifting weights doesn’t concern me as would the same complaint coming from a 48-year-old two-pack-a-day smoker whose father and two brothers died in their 40s of heart attacks.
Sometimes I hear a story to which my mind responds, “Oh, shit!” The first one I can remember happened in August 1989, about six weeks after my graduation from UCSD School of Medicine, during my first emergency room rotation as an intern at the Maine Dartmouth Family Practice Residency. As usual, I grabbed the clipboard of my next patient and strolled into the treatment room, where I found an adorable five-year-old, potbellied blond boy and his parents, each about 30 years old and oblivious to what would be the outcome of that day’s visit.
As the boy smiled up at me, his mother explained his recent troubles. “For the past several weeks, he urinates all the time, even during the night. His thirst seems unquenchable, and he has a voracious appetite.” I could have stopped right there; this was a classic presentation of new-onset juvenile diabetes. His blood sugar was 835 (normal would have been about 100).
Before I could say anything about his diagnosis, he offered without prompting, “I hate shots.” Well, kiddo, welcome to your worst nightmare; hospitalization, relentless venous punctures for blood samples, strict dietary restrictions, and multiple shots of insulin every day for the rest of your life.
Laura’s was also an “Oh, shit!” story, though I didn’t dare say that to my brother. She was describing olfactory seizures. Seizures are random uncontrolled electrical discharges within the brain that result in a variety of syndromes. The most common syndrome we think about when we hear the term seizure (or epilepsy, the illness of having seizures) is grand mal epilepsy, where a person loses consciousness and has frenetic, uncontrollable movements of the arms and legs. Laura’s random electrical discharges affected the area of the brain that processes the sensory input from the nose, so she experienced these events as powerful odors. They did not involve her motor cortex, which sends the messages that affect muscular activity, so she did not have any problems controlling her movements. Nor did she suffer loss of consciousness, the criterion we use to separate “partial” from “complex” seizures.
The bad news for Laura wasn’t that she was having seizures, although seizures are potentially dangerous events. Many people have seizures, and usually we can stop them with medication. The context was the bigger issue; she was a healthy woman who had never seized before. Her story immediately brought to my mind a 51-year-old woman whom I had seen as a resident three years before in the emergency room. As she was watching her television that afternoon, the TV began to move away from her, as though it was fading into a remote tunnel. Like Laura, she was having a temporal lobe seizure, but hers affected her vision. Like Laura, she had never had a seizure before. Like Laura, this meant almost certainly that she had a brain tumor.
I told John that I did not like the sound of this; Laura had something in her brain that did not belong there. I said it would not do us any good to speculate until she had her MRI scan, which I knew the neurologist would recommend. The 51-year-old woman from my residency days had a benign tumor, a meningioma (derived from the meninges, the thin layer that surrounds the brain and spinal cord) the size of an orange, which a neurosurgeon removed without touching the rest of her brain. We could still hope that Laura would be as fortunate. A couple of days later, John notified me that she would have the MRI that Saturday and asked if I could go. I had call duty that day, which meant I might be working at the time of the scan, but 1 would try to be there.
About ten minutes after the technician had finished, I arrived and caught a glimpse of Laura’s MRI scan through the reception window. MRI, or magnetic resonance imaging, is a technique that takes pictures of the insides of our bodies with such clarity that an MRI scan looks like a large black-and-white cross-sectional photograph of the targeted body area. Each of the intricate structures of the brain, every fold (“sulcus"), fluid-filled space (“ventricle”), and cortical layer, shows in near-perfect anatomical detail. Benign tumors have symmetrical shapes, uniform composition, and sharp, discrete borders, which were what I had hoped to see.
Instead my eyes met an ugly, dense, swirling white mass that looked like an expanding galaxy invading her temporal lobe, with linear white rays streaking outward from the center into the surrounding cortex. It could have been a diagram of a small white explosion. Malignant tumors such as this gliocytoma grow rapidly and therefore often cause symptoms of increasing pressure inside the head (“intracranial pressure”), including headaches, vision changes, and altered levels of consciousness (drowsiness, lethargy). They also show “mass effect” on the MRI scan, pushing brain tissue into areas of lesser density, such as the fluid-filled ventricles, which show up black on the scan in contrast to the white and gray cortical structures. Laura’s scan showed compression of one of her ventricles.
I walked through the door separating the patient waiting area from the computer controlling the MRI scanner. Todd, the radiologist on duty that Saturday, looked up at me. Being new in town at the time, I introduced myself to him and explained that Laura was a close friend of the family.
We both realized we were dealing with an otherwise healthy young woman with a brain cancer that looked incurable. The cancer was invading the surrounding brain tissue so aggressively that it would be impossible to try to remove the whole thing without disabling vital cognitive structures. “Obviously, this is a terribly abnormal scan,” Todd began. “This puts you in an awkward position, because it will be at least two days before she can consult a neurosurgeon to get the answers she needs once she learns her diagnosis. It would not be fair to tell her the results now without access to that information.”
As a rule, I don't lie to patients. Ever. But when a physician gives terrible news to a patient, within a few minutes the patient wants to know what will happen next and what his chances of survival are, and neither Todd nor I could give reliable answers to those questions. This is the one situation I can recall in my career that I did lie. I thought it was better to tell Laura that I didn’t see the results than tell her she had a deadly-looking brain cancer on a Saturday and make her wait for 48 hours. Because of that experience, I don’t recommend getting important tests on weekends, even if it is more convenient
Laura saw a local neurosurgeon the next week, and he confirmed what we already knew; he couldn't operate on the tumor and therefore could not cure it. I found this out when John called me later in the week and asked if there was anything I could do. Had I been living almost anywhere except the San Francisco Bay Area, the answer would have been no.
Up until that time, I had heard of but never dealt with Dr. Charlie Wilson, Chief of Neurosurgery at UC San Francisco. He was more famous than any physician to whom I had ever spoken in my life, and I did not have any idea whether he would accept a referral from me. But after I left a message, he called me back, took the referral with courtesy and gratitude, and arranged to see Laura the following week.
Dr. Wilson had recently pioneered a surgical technique for which he believed Laura would bean excellent candidate. Under local anesthesia with the patient awake, he stimulates each area of the brain he wants to remove to see whether he is disturbing vital processes. He can then make a precise map of where he can cut and where he cannot, allowing him to be much more aggressive in his attempts to resect as much of the cancer as possible without creating disability. When the only other option is certain death, brain surgery while awake makes sense.
After surgery, Laura underwent radiation treatments aimed at eliminating any residual tumor. Radiation and chemotherapy treatments work because they selectively damage the most rapidly dividing cells in the treated area, which are often the cancer cells. Of course, many normal cells in the body are also dividing during the period of treatment, so these cells die as well. This is why these treatments cause, among other things, hair loss and anemia, because hair cells and blood cells are among the most frequently produced and rapidly turned-over cells in the body.
So Laura lost much of her hair from the radiation treatments. The next time I saw her, four months after her surgery, she was sporting a buzz cut that almost covered the circular scalp scar surrounding a slight indentation in the side of her head Dr. Wilson had removed almost all of the tumor, something 1 can barely believe to this day. The day I saw her, Laura had just gone for a follow-up MRI scan that did not show any evidence of residual tumor. She had resumed full-time work and recreational dancing and was feeling well.
She then did something that caught me off guard; she thanked me. All I had done was make one phone call, I reminded her. I was just thrilled that she was doing so well. But she pointed out that her primary care physician had not suggested she do anything beyond consulting the local neurosurgeon, an experienced, talented, and highly respected individual, who had given her the initial dismal news.
One of the realities of primary care is that most of what we do goes unnoticed For example, we have to treat 65 people with high cholesterol to prevent one heart attack. But in this one instance, I did something very easy and received a tremendous reward. Three and a half years later, Laura’s MRI still shows no evidence of tumor. That’s why I do this.
Comments