 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
During the first year of my residency in family practice in Maine, I came home to Los Angeles for Christmas. The climate switch in the seven-hour cross-country journey, from minus 10 to 86 degrees, didn’t trouble me as much as the prospect of getting together that evening with friends I had not seen since high school As my brother John and I drove south toward the floor of the San Fernando Valley, I posed the unsettling question.
“Since before I went to medical school, do I seem different to you?”
He reflected a few moments. “You have joined a kind of fraternity. You have been places the rest of us haven’t. There’s a part of you that the rest of us don’t know and may not understand. That puts some distance between you and us. But you still seem pretty much the same to me.”
More than 3700 college graduates had applied to enter UC San Diego’s School of Medicine class of 1989. UCSD invited 230 to spend the next four years at one of the finest schools in the country; 122 of us accepted the offer and arrived in La Jolla in September 1985.
Why were we chosen?
I had wanted to be a doctor since graduating from elementary school; I never seriously considered anything else. I did not have any doctor role models in my immediate family, but my chain-smoking, wisecracking, New York-bred pediatrician impressed me, as my mother trusted her more than anyone. For example, my inability to consume an entire cookie at age eight concerned my mother, as I was quite skinny then, even more so than I was upon entering med school, but Dr. Mont’s advice reassured my mother. So, in the manner of a great many premedical students before and after me, I had applied myself in a focused fashion to earning the Greek and Latin distinctions (Phi Beta Kappa, magna cum laude) and high numbers (3.8 GPA from Pomona College and a 10, two 11s, and three 12s on my Medical College Admissions Test) that would allow me a chance to obtain my M.D. To eight schools I had presented my credentials, my slender six-foot, four-inch frame (befitting my Dutch heritage), my similarly lengthy convex nose (Jewish ancestors contributed this), and my sincerest pledges to benefit mankind. UCSD extended the invitation and now, at age 22, my time had arrived.
Accompanying me was a diverse collection of individuals, including carpenters, philosophers, athletes. Mormons, Muslims, Catholics, Vietnamese, and Iranians, from places like Stanford, Harvard, Yale, and UCLA. We shared a common trait, which had written our admission ticket to UCSD: our proficiency as test takers. We had mastered the “art" of absorbing huge quantities of information in a short time and regurgitating it onto an examination paper. One might hope that, since we would become some of the most trusted members of society, whose daily decisions would profoundly affect people’s lives, we would also have distinguished ourselves with our honesty, reliability, and sound judgment.

Well, we had not and did not. Once during the first two years, our faculty announced they knew some of us were cheating on exams. They had us fill out an anonymous survey that asked if we had ever witnessed our classmates cheating. I never had, but after one exam my roommate, a test-taking star among stars who seemed out of sorts that day, confided that someone had looked at his answers. The faculty tried from the beginning to downplay competition, emphasizing that they considered each of us an “honors” student, and therefore all courses were graded pass/fail. (From this, we students derived “The Golden Rule of Medical School”: P = MD.) They shot themselves in the foot, however, by including “honors” and “low pass” distinctions in each course, which ensured that the incurably competitive would compete. Many of us competed just within ourselves. Others argued heatedly with professors during post-exam reviews about the fairness of questions answered incorrectly. Some, apparently, resorted to other means to improve their chances. I don’t think the faculty ever caught or disciplined anyone for cheating.
In many ways, we first-year students acted no differently than our undergraduate counterparts at UCSD. In fact, their professors provided almost all our first-quarter lectures in biochemistry and molecular biology. Our corner of the campus, its expansive, lush green lawns surrounding the gray-and-white concrete walls that enclosed our lecture halls, labs, and library, stood apart from the rest of the campus but did not particularly distinguish itself.
Our approaches to learning differed. Some of us attended every lecture, which during the first quarter meant eight hours of class three days a week and four hours the other three days (Saturday included), while others never attended unless it was mandatory. Many who showed up every day bored whoever would listen with complaints of long study hours; others would go to great lengths to hide the number of hours they spent over the books. The quantity of material we had to memorize required that we all work hard, but most of us found time to enjoy life in San Diego. I took a sailing course at Mission Bay in the spring, and many classmates pursued similar outdoor interests. We played intramural football, soccer, basketball, and softball and always finished at or near the top of the standings. Those of us just out of college threw parties, where we drank heavily and danced to “modern rock” (e.g.. Clash, Talking Heads, New Order).
I spent much of my spare time with a few single men in my class doing what they enjoyed doing: going to bars (the Elephant Bar, Carlos Murphy’s, the Belly Up Tavern, and others) to drink, dance, and pick up women. The latter, for me, was always a vicarious experience, because I never succeeded in picking up anyone at a bar (I stopped trying in 1986); several of my friends almost never went home alone. This was pretty frustrating; I remained a virgin until December 1987, narrowly averting a celebration of a quarter century of celibacy at my birthday party three months later. But my experiences in the bars of San Diego helped when I began my hospital clerkships at the start of my third year, because as frightening as a cross-examination by an attending physician could be, it never intimidated me as much as the women in the bars.
Other students led more responsible lives with spouses and children. We were 85 men and 37 women: two were married to each other, two were engaged but later broke up. We averaged 26 years of age. Most of us lived in the graduate student housing (“the ghetto" of La Jolla) east of campus; the apartments had modern kitchens and large rooms for about $150 per student per month. I couldn’t get in there the first year and a half, so I found a room in a Pacific Beach apartment with a 33-year-old divorced dental hygienist just recovering from leaving her alcoholic husband. We had grown up in the same San Fernando Valley town but had never previously met. Her closely cropped brown hair and pleasant personality did not prepare me for her quirks related to tidiness, one of which required that all utensils used to prepare meals be cleaned before I sat down to eat. This didn’t cause problems until I severed three ligaments in my left ankle during a basketball game and subsequently underwent surgery, after which I wore a cast on my ankle for six weeks. One evening, after a draining day at school, I limped around the kitchen to prepare my dinner and then dared to sit down before cleaning out the pans on the stove. She threw a fit, unimpressed by my crutches, sad dark eyes, and imprisoned lower leg. Other than that, I liked her. But when a classmate called with news that a college friend of his had just moved to San Diego and needed a roommate, I did not hesitate.
Perhaps the most important perk to many of us was the low cost of a UC education. When I started medical school, the annual tuition at Georgetown University in Washington, D.C., had reached $25,000. Georgetown represented the high end of the price range, but most private schools checked in at well over $15,000 annually. The University of California’s cost, about $500 per quarter, saved those who lived in California when they enrolled nearly six figures of debt over the four years. Almost all of us entered med school with an undergraduate debt load; mine totaled about $7000. To minimize my debt, I worked part-time as a typesetter for the Guardian, UCSD’s school paper, during my first two years. Four years later, I graduated $30,000 in debt; many of my present colleagues who went to private schools had debts ten times mine. Doctors who are just starting out, often after buying a practice, are commonly faced with a debt load approaching half a million dollars before they see their first private patient.
Some among us had a head start: born in Beverly Hills, educated in Ivy league schools on their parents’ accounts... one drove a Porsche. He was the youngest of our class (20 years old in 1985) and had a charming exuberance that endeared him to most of us. His entire immediate family died in a plane crash during our third year. Enough catastrophes confront third-year students to test their sanity limits anyway, so I admired Derek for the way he handled the most tragic event to happen to a class member in our four years, never losing his kind, gentle manner. The last I heard he had finished his pediatrics residency.
We had your typical dwarfish, rotund Yale grad with round, rimmed glasses covering owlish eyes, who would commemorate the end of many a lecture with an indecipherable question about some obscure detail that neither the professor nor any of the rest of us cared about. Another otherwise likable fellow had the same annoying habit, although his questions generally maintained a relevant thread. Many of us left the auditorium between lectures while those two finished their business.
Truthfully, most of what happened during the first two years bored us at the time and isn’t exciting to recollect here. Gross anatomy broke the routine. Taught during the first year at most medical schools, anatomy opened the second year at UCSD, immediately preceding the pathology (study of disease) courses.
Anatomy carried an aura of intrigue. Legends, the truth of which purveyors of the oral “history” were never quite sure, were part of course orientation. One tells of a student who borrowed part of his male cadaver to take to the local movie theater. After entering the restroom of the movie house, he strode up to a stall and hurriedly took care of his business. Upon finishing, he frantically yanked up his zipper, paused, and then let out a long howl and ran from the bathroom doubled over in mock pain, leaving “his” penis on the floor, to the horror of the old fellow using the adjoining stall. Another tale claims that a medical student startled an East Coast toll collector by handing him a pair of testicles in lieu of the usual fee and sped off. There were countless others.
The atmosphere added to the aura. A distinctive formaldehyde stench greeted the nose of everyone who wandered into the basement lab, where the 30 or so preserved bodies rested on dissecting tables under drop cloths. The cool, windowless laboratory featured blocklike workstations with sinks and drawers of typical lab design. It also featured laminated specimens of preserved human structures, including cross sections of the abdomen (about an inch thick) and a human skeleton. With classmates present and in the context of learning, most of us enjoyed the class, but the few times I went down there to a study session at night, the air was heavy with death’s stale, penetrating odor, and upon exiting into the still, black night, my body couldn’t suppress a shudder or two.
Dr. Halasz, a Greek general surgeon with a bushy gray mustache, ran the course. While students dissected cadavers, five or six professors roamed among us. Dr. Laurenson, a poetic Canadian, complete with beret and wry wit, always kept things in the proper perspective (when asked for advice before the first exam, he counseled us, “Always drive the Mercedes”). Dr. Wilson, a soft-spoken, gentle, matronly sort, periodically suffered attacks of Meniere’s disease, a poorly understood inner-ear condition causing intermittent attacks of severe dizziness and nausea, but she rarely complained while detailing the development of bodily structures from their embryologic origins. Dr. Breisch, a young New Jersey stud who dazzled us with knowledge and tall hunting tales, didn’t publish enough research, so despite his unusual gift for teaching, the university served him his walking papers after he finished with us.
Dr. Halasz began the introduction to our cadavers with a philosophical discussion of the difference between human bodies and human “remains”; drawing such a distinction made our work easier on the conscience, although once we started, the task at hand often made us forget that we were cutting up dead people. We divided into teams of four. My team’s “remains” had belonged to a woman who was about 90 when she died. All teams named their cadavers; we could not come up with anything we felt appropriate, so we respectfully called her "Ma’am.”
I do not remember much about the dissection, except that dead tissue almost always had a very tough and leathery feel to it, which I later discovered contrasted with the soft, elastic, and sensual fullness of living tissue. My only prior exposure to a dead human was six years earlier after my girlfriend’s father had dropped dead of a heart attack at the dinner table. I recall peering into his open casket and noting how peaceful he looked. What I really saw was the absence of color and expression that life gives a face.
While we worked on the bodies, the cadavers’ heads hid under wraps. Before their unveiling. Dr. Halasz called us together to prepare us. He explained that life brings a tremendous amount to a face, and that fact never is more evident than when one looks at the faces of the deceased, for they all look remarkably alike. Much of our unique appearance dies with us. I had trembled when I thought of slicing into Ma’am’s face, but death had stolen her human qualities. The warm, gentle, grandmotherly countenance I had expected wasn’t there; the vacancy of death had replaced it. Within a few minutes of making the first incision into her cheek, I once again immersed myself in learning.
Each of our examinations in anatomy had a written component and a lab practicum component. For the latter, the faculty would label parts of our cadavers with numbers and ask us to name the parts. During our first exam, I noticed that many students were taking longer than usual to look at one item, and when I arrived, I understood. Before me rested an amorphous body part, separated from the cadaver, lying sprawled out, limp, and composed mostly of soft, oily, yellow globs of stuff (fat). After 45 to 60 seconds, I walked around the specimen and found the skin over the front, at which time it dawned on me that I was looking at a female breast. Why anyone felt the need to detach it completely to label one of Cooper’s ligaments, which support the breast. I’ll never know, as I have never since had to identify one without a woman attached. I later noticed a bumper sticker in the lab that read “Parts is parts.”
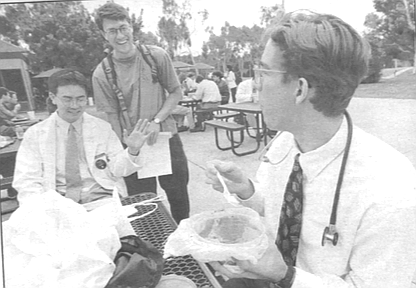
Stuff like that took much of the human empathy out of the first two years of medical school and made it challenging for me and others in my class to maintain the focus of what this was supposed to be about: taking care of living human beings. Amongst the memorization of often trivial facts and the obsession over examination scores, glimpses of patients were rare until our Introduction to Clinical Medicine courses, which began in the winter quarter of the second year. This was our first chance to put on white coats and use stethoscopes and other tools of the trade on a semi-regular basis.
A fourth-year medical student, Bill, taught the physical examination we would perform on patients our third year. He showed us everything except the gynecologic exam; nurse practitioners taught that, using themselves as models and subjects for our first exams. For everything else, we practiced what we learned by examining fellow students. Each of us chose a partner. The couples in class had an advantage, as one learns more by practicing with a member of the opposite sex. I don’t remember much about these sessions, except the part when Bill told us that the exam involved inserting the index finger into the patient’s rectum, feeling the anatomy within, and extracting a lump of shit to wipe on a card, onto which we then dropped a clear liquid that turned blue if the “sample” contained occult blood. They spared us the indignity of doing this to one another.
Soon we began to practice our newly acquired skills on hospital patients. I found myself trying to behave as I believed a doctor would, thinking that would reassure the patient that I knew what I was doing. Perhaps this is why some doctors never stop presenting themselves to patients in a way that implies the doctor knows more than he or she really does.
My first patient, an attractive and pleasant 51- year-old blond woman with a fair complexion and crippling arthritis, treated me with an almost motherly kindness and respect. Sporting white coat, button-down shirt, and tie, I made my best effort to present myself professionally, and I managed quite nicely through the lengthy interview and the examination of her head and neck. This despite the inconveniently low height of the hospital bed she sat on, which was causing my back to ache in a way I could barely conceal. I then proceeded to examine her breasts, and at first this went well; neither of us seemed ill at ease as she sat bare from the waist up and 1 hunched over trying not to create any impression that I could think of her as a sex object. But women still made me nervous, and suddenly my antiperspirant and every other antisweat mechanism in my body gave way. I had to sheepishly excuse myself to dry my soaking-wet face and neck with a handful of paper towels from the dispenser above the sink. My recollection is that she thoughtfully offered some comment about the heat in the room (or maybe I did), as though we had suddenly transported ourselves from the San Diego winter to summer in Death Valley. I felt very much the naked emperor in front of my half-naked patient. Her grace, not mine, allowed me to finish, and my thoughtful write-up earned high praise from my preceptor. We doctors all have patients we owe for what they teach us about our profession and about ourselves; I’m eternally grateful to that woman.
I overcame most of my anxiety about examining women quickly, thanks to the nurse practitioners who so calmly allowed us to perform pelvic exams on them and taught us how to do so thoroughly and gently. Women wonder what goes through our minds when we touch their genitals, insert instruments in their vaginas, and probe their insides with our fingers. When we’re just starting out, I think most men feel as I did. I feared that my women patients would think I was having fun at their expense, and this made me nervous enough to sweat and far too nervous to have any sexual fantasies. On a few occasions, when my fingers would slide into a vagina that had unusually profuse lubrication, my stomach would gnaw at the thought that the patient was having more fun than I was comfortable sharing.
Later, as I grew more confident and understood better what I was doing, I found that the concentration required to do the job generally precluded any nasty thoughts. I examine women of all shapes, sizes, and ages, but what determines how I feel about the exam is their maturity and self-esteem. Good hygiene helps, but I can work through even the most nauseating of odors. Examining women who are comfortable with themselves is easy, no matter how they look. I would be lying, however, if I claimed that looks do not matter. It is easier and more pleasant to do a thorough exam on an attractive person, just as it is easier to look at one. If a woman looks and smells terrible, a careful exam is more difficult to do, although many of us, myself included, are aware of this and make a special effort to take enough time with such patients. Women who are suspicious, nervous, or unable to suppress giggles present a challenge, but my nine years of experience have given me enough composure that I cannot remember the last time I or a patient had emotional difficulties during a pelvic exam. Many women have an easier time with female providers, but some prefer a male physician; I’m not sure why that is and I would like to find out. In any event, for me and most of us, once we overcome our fears when we are rookies, we’re just doing our jobs when we examine women. Our patients do enter our fantasies once in a while (and we enter theirs), but it’s rare and, for most women, not worth worrying about (in my male opinion).
Perhaps this is the time to mention that pornographic movies were a part of our core curriculum during the first year. The idea was to confront us with different sexual orientations and experiences so we could deal with our reactions before patients challenged us with their “lifestyle-related” problems. Despite much anticipation and preparation (many of us came to class that morning with popcorn and Milk Duds), the event disappointed me. The films showing male and female masturbation, gay males, and lesbians didn’t have any plot or character development, and consequently didn’t offer much to those of us who had lived in urban areas. By far the most stimulating of the offerings involved a heterosexual couple in their 60s, which, as my oldest (33) classmate pointed out, gave us hope for our future. The advertised video of a young heterosexual couple was not available; too bad for those who came to class hoping to learn something new.
After two years in the lecture hall and laboratory, we spent two days answering the 999 multiple-choice questions on the National Board of Medical Examiners’ Examination: Part I. This is the first and toughest of the three National Board examinations one must pass to qualify for a medical license in the United States. We take Part II during the fourth year of medical school and Part III at the close of our internships. The completion of Part I marks the end of daily treks to the lecture hall and the beginning of hospital clerkships, where we finally begin to take care of patients. Unlike the first two years, when we all share pretty much the same experiences, the class separates during the clinical years, never meeting as a whole again, and each of us has a highly individual experience. The following vignettes give some details of mine.
MR. CLEAN
The month of August 1987 brought me to my first hospital clerkship: neurology at the VA Hospital. My only previous exposure to medical neurology came during the spring quarter of our first year in a basic neurology course, the most interesting course of the least stressful quarter of the first two years. No organ surpasses the brain for complexity and intrigue; learning how the brain works and how each area exerts its influence fascinated me. Of course, one cannot deny the macabre nature of cutting up and studying brains, as we did in neuroanatomy lab. Our favorite neuropathologist, a cheerful and engaging British chap, Dr. Powell, led us through the ceremonious “Brain Cutting” sessions, in which he unlocked the mysteries kept within the brains of persons recently deceased from or with neuro-logic diseases. Boyish in appearance due to his short stature, despite his middle age and white coat, his enthusiasm captivated his audience of 10 or 15 students, interns, and residents. We were seated above him on several rows of wooden bleacher seats in the tiny theater downstairs. Carefully he sliced the brains into thin sections in the manner of one preparing a fine salmon loaf. Thusly he demonstrated the atrophied cortex and mammilary bodies (the “breasts” of the brain) in the alcoholic, the compromised substantia nigra (an area of “black substance”) of Parkinson’s disease, and other abnormalities of such regions as the “pale globe” (globus pallidus), the “tail” (caudate), and the “almond” (amygdala), all of which resemble their namesakes.
We spent more time with live patients. People with neurologic problems, particularly those localized to specific areas of the brain, can be interesting and sometimes cruelly entertaining to study and observe. Oliver Sacks describes extraordinary cases in his books, but I had not yet read these, so I was unprepared for what I encountered.
Adam and Paul, two witty transplanted Ivy Leaguers, were my partners for our four-week neurology rotation at the “Va spa,” the euphemistic nickname we physicians in training gave the Veterans Administration Hospital in La Jolla. Although it is one of the newest and nicest of the VA hospitals, one would never willingly stay inside long. It features cheerless, faded gray-white hospital corridors, interrupted by outpatient waiting areas crowded with the day's patients. Interns, medical students, and other hospital personnel, some responding to operators’ messages resonating from the intercom, passed quickly by patients strolling the halls in hospital gowns, pushing IV poles with bags of yellow urine from the Foley catheters wrapped around their legs. Paul dressed up as a veteran at our Halloween party that year, complete with gown, Foley, and cigarette. His and Adam’s senses of humor, laced with cynicism, helped get me through what was otherwise a dreary month.
Among other things, most veterans learned to smoke and drink in the military, and the “spa” was where they were treated for the consequences.
We frequently revisited the subject of alcoholism during our month on the neurology ward because of the academically interesting and humanly tragic effects it has on the brain. One patient, J.M., suffered from Korsakoff s psychosis, a condition in which the ability to form new memories is destroyed. To compensate, affected individuals confabulate, which renders them interesting interview subjects. When asked, “Do helicopters eat their young?” a patient with Korsakoff s might answer, “Only when they’re hungry.” Paul thoughtfully asked J.M., who was sitting with several other demented patients one afternoon during lunch, “Would you like some grapes, Mr. M.?” The pale, wheelchair-bound gentleman reflected for a moment before replying, “No thanks. I just had a bar of soap."
More sobering were the stroke victims. Veterans, because of their smoking habits, frequently acquired during the years our government provided servicemen with free or cheap cigarettes, often succumb to complications of atherosclerotic disease, which clogs the arteries. Heart attacks and strokes are common examples of these complications.
One tragic case was an elderly gentleman who had already lost the function of his left arm and leg from a previous stroke. He came to us because he had suddenly lost his ability to make new memories; he forgot within a minute anything that happened to him. He did not show any other new deficits in his sensation abilities or in his movements or reflexes. An alarming scenario for him and his more youthful brunette wife, this was a particularly curious one for us, because sudden isolated memory loss is rarely seen; most memory loss, such as that of Alzheimer’s disease or Parkinson’s disease, occurs gradually. It is puzzles such as this that attract neurologists into their specialty, because for most neurological syndromes there is a logical answer awaiting the clever doctor/detective. In this case, we tracked down the head CT scan from his previous stroke, which showed an impressive dark discoloration of much of his right hemisphere typical of a stroke affecting the right middle cerebral artery. The attending neurologist looked it over thoughtfully and came up with the solution. The first stroke had affected the hippocampus, one of the key memory centers, but only on the right side. Stroking out the hippocampus on one side often fails to produce any measurable memory deficits, but if you knock out both sides, you get profound deficits. A CT scan several days later confirmed the diagnosis: a new stroke affecting almost exclusively the left hippocampus. Why didn’t it show up on the CT done the day of the stroke? Because nonhemorrhagic strokes do not immediately show up on the scan; it takes about 48 hours for the dead brain tissue to lose enough density to be visible on an x-ray.
As is often the case with neurologic disease, once we solved the puzzle, we could not do much for the patient. He now not only could not use half his body, but he could not remember that fact or almost anything else, which led to frequent, dangerous attempts to get up and walk that always ended with him on the floor. He was one of the cases that convinced me that 1 would not become a neurologist. I value recovery from illness much more than the thrill of the diagnostic chase.
FRESH AIR
Changing venues from the VA neurology ward to Children’s Hospital was like moving from Detroit to San Diego. Optimism, a rare commodity at the VA, overflowed at Children’s. The pace and energy of the place picked up the spirits of many disgruntled students who wandered in after four weeks of slow-moving patients at the VA.
Our workload also picked up a bit, including overnight call every fourth night. Early one evening on call, I admitted to the medical ward an asthmatic dark-haired, chubby-cheeked Mexican boy, about 14 months old. At that age, one has a well-developed sense of fear and a need to protect oneself from the unknown, so imagine being dragged in that frame of mind into a large, unfamiliar building full of strangers, many of whom are trying to probe you with needles to fill your veins with antibiotics and theophylline (a caffeine-like medicine that opens bronchial tubes) or blow cold mist (containing oxygen and bronchodilators) into your face. All of this is happening while you feel as though you are drowning: you can’t get enough air. So this little boy made no effort to hide his feelings about me or my attempt to examine him. He screamed. He punched. He kicked. He bit. We prevailed. I left him to his mother, his nurse, his medication, and his breathing treatments and continued my evening’s work with other patients.
Several hours later, after his mother had left for the night, I dared to venture back into his room to check on him. I intended to listen to his lungs and hoped that if I approached slowly his protests would be mild enough to allow me to do so without bringing in Marines to help. As I approached, he stood up in his crib and gripped the vertical metal bars in a pose that was becoming familiar to me on the pediatric ward: that of children doing their time until they were fit to be released into society. He began to cry as I raised the upper bars to reach him, but I was able to press my stethoscope against his back to listen, noting that the wheezes and other adventitious musical sounds were louder than previously, which meant he was moving more air into his lungs. Then, the unexpected happened: as he cried more loudly, he stretched his arms out toward me with an expression of terror on his little face. I let out a big “Aw.. picked him up, rocked him in my arms, and told him he really was going to be okay. This was one of the few moments of pure human sweetness I would be allowed during my third year of school, and I enjoyed it fully. After a few minutes, I had to leave and replaced the crying child into his little cell-like crib.
In retrospect, I wonder which of us benefited more from that encounter. For me, it was one of the defining moments of my career, it helped convince me that my choice to'become a primary care physician, a family practitioner, was the right one. The little boy recovered and went home two days later.
BOOMER AND THE BROOMSTICK
We all dreaded our 12-week surgical clerkships. Workdays of 14 to 20 hours were routine, and the stories of student abuse made many of us hit the antacids before we started. Later we discovered that some surgery residents drank Mylanta or Maalox during morning rounds.
One brilliant attending surgeon, who enjoyed a worldwide reputation for many reasons, earned most of his notoriety on campus with his blatant disrespect for students, particularly women. “Medical students are like undescended testicles,” he used to say, only partially in jest. “They are always late, and when they arrive, they are useless.”
“You are doing the work of two people,” he informed one exhausted student during a lengthy operation. “An idiot and an asshole. Pretend like you are trying to help me.”
To him, any female student was named Veronica, that is, when he wasn’t calling her his favorite nickname: sexpot. “You are only good for one thing,” he would frequently remind his current Veronica during surgery. And if Veronica happened to be holding the suction when he needed it, he would demand of her, “Suck me.”
Hospital rounds were no picnic either. He did not trust students to say anything to his patients. If a patient asked Veronica, “What time is it?” she was expected to answer, “I don’t know. I’ll have to ask Dr......
Knowing his reputation, I knew I wanted to do my six weeks of general surgery where he would never find me: the Balboa Naval Hospital. I got my wish. I could never stomach a long-term relationship with a military institution, but I’m grateful for the six weeks of grueling work, relentless questioning, ridiculous hours, and minimal sleep I spent there. The residents and attendings (attending physicians) valued my presence and my work and made sure I learned something.
As I had expected, the patriarchal structure of the military resulted in a male-dominant atmosphere the testosterone-laden dialogue often seemed more appropriate for a locker room than a hospital, and I occasionally felt more like a member of a high-school basketball team than of a surgical team. Boomer, the chief resident of our team, had the boyish face and pouting lips to match his nickname and a coach’s penchant for lectures about teamwork and motivation. Of the three chief residents. Boomer headed the class, with an extensive fund of medical knowledge, excellent clinical judgment, and supreme self-confidence. I had none of that and assumed the role of “raw young pup,” as Boomer later remembered me.
Our schedule ran in three-day cycles: one day admitting surgical patients to the hospital (pre-op day), one day in the operating room and one day in outpatient surgery clinic. Every day began at 5:30 a.m. with work rounds, when we would see patients who were recovering from surgery, determine their condition, formulate that day’s treatment plan, and then, in my case, have the plan shot down by the chief resident. On pre-op days, we would then get our assigned patients, perform their histories and physical examinations, write them up, and get ready for pre-op conference in the afternoon. At these conferences, medical students and interns presented the patients admitted that morning for surgery, and then answered a three-hour barrage of questions about them and their medical conditions. Our attending physician, Captain Carlisle, chaired the afternoon sessions.
One afternoon I presented a patient who would be undergoing a vein-stripping operation to treat painful varicose veins caused by abnormalities in her venous circulation. This led to a discussion of venous anatomy and circulation. After the usual review of the anatomy of deep veins, perforating veins, and venous valves, Captain Carlisle took a more personal approach. He turned his bald head and dark gray mustache to launch his deep, booming, staccato voice
“Just exactly where is the greater saphenous vein, James?” he demanded. An easy question to answer.
“It runs over the medial malleolus...”
“Show me YOUR saphenous vein, James!”
I felt a pounding at my temples, heralding the onset of one of my frequent migraines, as I quickly, though reluctantly, pulled up my left pants leg to demonstrate my easily visible vein.
"Not everyone's as large and obvious as yours, but remember, it is ALWAYS there. When you need venous access [to give intravenous fluids in emergencies] immediately, it is ALWAYS there.”
Point taken. Although I had unpleasant visions of future conferences (e.g., “Show me YOUR genitals, James!”), Captain Carlisle never repeated this tactic.
On operating days, we would go from rounds to the operating room. Two residents and the attending physician usually performed the operation; my job was to pull consistently and firmly on retractors so they could see, while I could not, and to field questions about the anatomy that seemed always just out of view. Later in the day, the number of surgeons would diminish, and one assistant for a lone surgeon, usually Boomer. These were the real learning opportunities.
One night we got a call from the emergency room. A young midshipman had come in complaining that he had sat on a broomstick and, much to his chagrin, it had broken, and he couldn’t get the stick out of his rectum. This being a military hospital, it became apparent to me that the retained broomstick probably represented far less a problem than the disciplinary measures he would almost certainly face because of this closet-betraying incident. After Boomer and I rummaged through the operating room supply areas to find tools to retrieve the mislaid stick, we entered the OR where the cowering, terrified 'patient lay on his back with his legs elevated (in stirrups, I think). I can’t remember his face, just the feeling in his expression. A couple of pushes on his abdomen resulted in a colonic spasm that delivered the stick within easy reach of the anus, so Boomer just pulled it out. Elated at the ease of the procedure, and with his glove covered with shit, Boomer couldn’t resist offering his suffocatingly malodorous hand to the OR nurse, saying with an impish grin, “Damn glad to meet ya.” He then went up to the young victim and sternly warned him, “This time, you were lucky, but don’t let anyone find you doing that anymore.”
The next morning, I got a good look at the downside of staying up most of the night in the name of education: I slammed into the rear of a four-door sedan that had suddenly stopped in the fast lane on I-5. My car fared worse than either driver, and my insurance company paid for the damage. To this day, that remains my only accident.
THE PUMP ROOM
Sleep deprivation didn’t become a way of life until my three-week introduction to cardio-thoracic (CT) surgery. The workday began at 4:30 a.m. and ended at 10:30 p.m., and if you happened to be on call that night, you didn’t even get those other six hours off. But believe me, when you get inside a living person’s chest cavity, staying awake is not a problem.
Nothing one experiences, neither in the first two years of medical school nor in ordinary life, prepares one to enter the realm of such things as cardioplegia and extracorporeal oxygenation. I had never witnessed the beating of a human heart, the inflation and deflation of human lungs, or the bony cage of human chest wall within which this life-defining activity ceaselessly continues. On my first day I was led into the operating room to the area just above the patient’s head, where the anesthesiologist resides. A second-year surgical resident was cracking open the patient’s chest, buzzing through the sternum with something similar to a Black & Decker circular saw. The vital structures quickly came into view.
Then the fun really began. The surgeons inserted a large cannula (tube) in the aorta and another in the vena cava, thus bypassing the heart and lungs and directing almost all the patient’s blood to “the pump,” within which the blood exchanged carbon dioxide for oxygen, a task normally handled in the lungs. This is extracorporeal oxygenation.
No one had briefed me on the details of cardioplegia. I did my best to maintain an ostensibly curious, calm, and interested demeanor, while my surgical mask hid my gaping jaw, as the surgeons stopped the heart and cooled the body to four degrees centigrade (39 degrees Fahrenheit). This “cooling down" diminishes the body’s requirements for oxygen and nutrients, giving the surgeons time to accomplish a heart operation, such as bypassing dogged arteries to the heart or replacing a defective heart valve.
The warm, wet odor of the open chest took me back to the dog labs of the winter quarter of our first year. These labs demonstrated some of the principles of cardiovascular physiology and pharmacology that our professors had described during lectures. The dogs we worked on had come from the animal shelter, where they had escaped immediate execution by volunteering to be our helpful subjects. Senior pharmacology students and others who administered the laboratory course anesthetized the dogs deeply, intubated them (placed a breathing tube down the trachea), hooked them up to a respirator (breathing machine), stuck pressure transducers into one of the large arteries to give us accurate graphs of each dog’s blood pressure, and inserted an intravenous line through which the lab assistants could give medications. I vividly remember our dog volunteer, a young German shepherd, whose little heart beat like a machine gun when we injected it with norepinephrine, epinephrine, or isoproterenol, all of which are powerful stimulants of the sympathetic nervous system. The point of the exercise was to demonstrate that norepinephrine acted on sympathetic nerve receptors in such a way that the heart rate, systolic blood pressure (the pressure during the heartbeat), and diastolic blood pressure (the pressure between heartbeats) would all rise; epinephrine stimulated a slightly different subset of receptors that caused only the heart rate and the systolic blood pressure to rise, while the diastolic pressure actually fell slightly, and isoproterenol acted only on one class of receptors and caused minimal change in the systolic pressure and a fall in the diastolic pressure while increasing the heart rate. At the close of the exercise, we opened the animal’s chest to get our first chance to do open cardiac massage. It seemed to me and many classmates that we easily could have just seen this on film rather than practicing this less than satisfying brand of medicine on our canine friends.
Back to the operating room. So now I’m looking at a human being with a wide-open chest cavity exposing a heart that is sitting like a lump of cold fat surrounded by ice, while the blood is being directed outside the body into this large box of a machine. And I’m thinking, “Isn’t this person dead? Is this a real-life demonstration of the mind-body problem? Assuming that all goes well when we restart his heart and warm him up, how do we know he’s really the same person when he comes back and not some other person who just has his memories? Why did I sign up for this?"
One reason I signed up was because coronary artery bypass surgery offers medical students extensive practice in stitching large wounds. The vein used for the bypass grafts, which allow blood traveling into a blocked coronary artery to bypass the blockage, much like a roadway detour redirects traffic, is the greater saphenous vein of the lower leg. After the surgeon removes the vein, he leaves a wound extending the length of the lower leg, which needs to be sewn together. Many a medical student learns to do an intracuticular closing stitch by sewing these wounds shut, and it provides that all-too-rare opportunity for a student in surgery to feel less like an undescended testicle and more like someone who has something to contribute.
Not that I really felt useful. One morning we were finishing replacing an elderly gentleman’s defective aortic valve when both surgeons became frantic. When they had reconnected the patient’s circulation, his aorta had revealed an unexpected fragility and had begun to disintegrate (“like tissue paper!”) under the pressure of his restored Wood flow. They hooked him back up to the pump, but because there is a limit to how long one can remain on the pump before serious physiologic consequences occur, this was a tough spot. They had about an hour to fix the aorta, which meant stitching an artificial graft to replace the areas that were falling apart. Given that there wasn’t certainty that any part of his aorta would be strong enough to hold the graft, everyone suspended the usual light banter that helped ease the tension of long surgeries. The surgeons’ orders and comments cut like knives into the still operating room air, and at times I felt as though I were forgetting to breathe. The graft held. We all welcomed the barbecue-like smell of smoke from the bovey, which cooks the open blood vessels below the skin and thereby stops them from bleeding, as this smell immediately precedes the closing of the skin, ending every operation.
So what happens to this cold, previously lifeless man once the surgery ends? We gradually warm him up, using blankets, intravenous fluids, and his own metabolism. The body responds to cold by constricting the arteries and veins close to the skin, preventing heat from escaping; this is why your feet and hands turn pale when they are cold. As the body warms up, the constricted vessels begin to dilate. Bypass patients demonstrate this dramatically. As the body warms to 95 or 96 degrees, the intravascular space suddenly becomes much larger, causing the blood pressure to fell, and we respond by rapidly infusing intravenous fluid to “fill the tank,” to maintain blood flow to the vital organs. Fluid management in these patients is tricky, because if you fill them up too fast, the amount of blood the heart has to pump exceeds the heart’s capacity, particularly in patients who have weakened hearts anyway. We call this situation heart failure. It results in fluid backing up into the lungs, which impairs the ability of the lungs to extract oxygen from the air. To prevent this, the patient has a Swan-Ganz catheter placed in the jugular vein and threaded through the right side of the heart to the pulmonary artery, where the volume of fluid in the body can be measured with the most precision. This is just one of many tubes used to manage these patients during and immediately after surgery, the others include an arterial catheter to measure the blood pressure precisely, a Foley catheter to measure urine output, a nasogastric tube to prevent aspiration of the stomach contents, and an endotracheal tube to which the ventilator attaches.
This setup was intimidating at first, but as with many situations encountered in learning this trade, you get used to it and more comfortable with it as you begin to understand and manage the equipment and the patient to whom it is attached. If the blood pressure is too high, you increase the infusion of sodium nitro-prusside, a medicine that dilates arteries and therefore decreases the blood pressure against which the heart has to pump, reducing the work of the heart. But this medicine is metabolized into a form of cyanide, so you have to monitor the total dosage carefully. If the pulmonary “wedge” pressure, measured from the Swan-Ganz catheter, is too low, you turn up the intravenous fluid infusion. For other situations, there are other adjustments. It feds much like driving a car, knowing when to use the gas, the brake, the air conditioner, etc. If all goes well, the patient gradually starts losing tubes and lines and begins to walk, talk, eat, and use the bathroom. Other than a scar, patients who haven’t had a major complication seem the same as before surgery. As a family doctor in training, I had always looked at people as a whole, rather than as a collection of organ systems, but my experience on cardiothoracic surgery gave me insight into why many specialists see people as an assembly of parts.
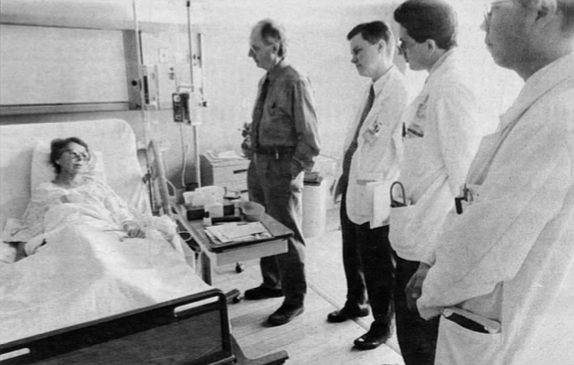
BILOXI BLUES
Humiliation was a way of life for third-year students, and my worst taste of it came during my clerkship in internal medicine. Our predecessors in the class ahead had informed those of us planning to do residencies in family practice or internal medicine that we had to have strong reviews from our attending physicians and medical residents during this rotation if we didn’t wish to spend our three years of residency in Harlem, Detroit, or other less desirable locales. Excellent performance required a thorough approach. Any patient assigned to a “stud” underwent the most thorough and detailed interview (history) and examination (physical) he or she had ever endured. Fortunately, we spent half our internal medicine clerkship at the VA Hospital; veterans as a rule were lonely people who were usually pleased with the one-on-one attention medical students provided. But some of our patients just wanted to be left alone.
One evening our team was on duty for the night (this occurred every fourth night) when Keith, my supervising resident, notified me that I would be admitting Mr. C., who was about 70 years old. He was coming in with respiratory insufficiency, meaning that his lungs were not providing his organs with enough oxygen. Because most veterans smoke, many of them run into this problem late in their lives, generally due to chronic obstructive pulmonary disease and/or heart failure.
When I arrived in Mr. C’s room, he had already been started on medications and oxygen to correct his problem, and he was comfortable. A diminutive, wiry fellow (decades of working to breathe sufficient quantities of air into smoke-ravaged lungs makes one very thin), he greeted me and initially seemed content to answer my stream of questions. I learned that he spent much of his time
in Biloxi, Mississippi, whence he had just driven to La Jolla, neglecting to bring his heart and lung medications. After about 30 minutes I sensed he was growing weary of my interrogation, so I began examining him. It didn’t take tong for him to lose his temper, and I eventually fled beneath his roaring “Get the HELL OUT OF HERE, YOU GODDAMN MEDICAL STUDENT WITH YOUR GODDAMN QUESTIONS....”
Nurses, patients, interns, and residents cast inquisitive and not ostensibly sympathetic glances in my direction as they identified the trigger of this outburst. I sought the shelter of a little room with bunk beds, where we spent our nights in the
hospital, to write up my findings, knowing that his reaction and the incompleteness of my work would be held against me.
During morning rounds, the team always visited patients at their bedsides, so the following morning Keith approached Mr. C., greeted him, and informed him that the rest of the team would be coming into the room. Mr. C. responded, “That’s fine. Everyone’s welcome...except that GODDAMN MEDICAL STUDENT WITH HIS GODDAMN questions. Get him the HELLOUTTA HERE!” I Stayed out.
After the team finished talking to Mr.C., Keith approached me and jocularly inquired, “What did you do to him?” I gave a puzzled shrug and explained that he had just suddenly exploded, at which point Keith took on a more serious tone and said, “Well, we rarely have to do this, but I’m going to have to take you off this case." One of the family practice interns and the other student working on our team offered me some support, but I felt abandoned, alone, and uncertain of my future in medicine that night.
A couple of weeks earlier a patient under my care had died. He was my first patient to die, but his death unnerved me for other reasons. A stocky, “tough-as-nails,” 59-year-old guy came in with pneumonia, and Keith assigned him to me.
Another smoker with significant lung damage, this muscular gentleman still led a vigorous life and looked as though he had another 20 good years left. However, his blood oxygen levels were dropping before my eyes, and it became clear to my inexperienced medical mind that he was likely to need more than just some oxygen blown into his face and intravenous antibiotics to get better; he looked as though he would be needing a ventilator. I talked to him about this, and he made himself perfectly clear: he didn’t want anything to do with endotracheal tubes or breathing machines. My explanation that he might need these to survive until the medicines started working did not change his mind. To him, mechanical ventilation meant a complete invasion of his personal space and loss of dignity. I’m not sure he ever understood that his need for mechanical ventilation would probably be temporary or that his stubbornness could be fatal to him and devastating to his wife. My shift was ending as I left his room, and I will never forget his wife asking me, “He’ll be all right, won’t he?” I responded honestly, with my throat in a knot, “I don’t know. He might not be.”
Somehow, when I went home that evening, I assumed he would be fine. The next morning’s news that he had been found dead in his room the night before was a rude awakening to the realities of practicing medicine. People, sane people, make “informed” decisions about their medical management that we who know and live with the consequences have to obey. There was more to it than that, though. That guy should not have died, and my team, particularly Keith and our attending physician, should have been more active in the care of a potentially critically ill patient. Knowing what I know now, I am sure I could have prevented his death by mobilizing his family and friends; his wife did not have the necessary influence to change his mind. Guilt overwhelmed me that morning; I felt that something could have been done to save him, and I was probably right. The VA Hospital conducted a quality-assurance investigation of the circumstances of his death. I do not know the outcome It was the only time during my medical school training that I observed negligence resulting in a tragic consequence. I learned then to trust my gut and to be willing to raise a fuss if I thought a superior wasn’t doing enough for my patient.
PSYCH
My next stop was a six-week stay on the locked psychiatric ward at UCSD’s University Hospital. The intimate confines, small number of patients, and close one-on-one working relationships with senior residents contrasted with the fast pace and often impersonal nature of the working relationships on my previous clerkship. At that time the ward had just 15 patients, split equally among three second-year residents. Each resident had a private office and one medical student who shared the office and patients. The patients were acutely ill, warranting hospitalization because they were dangerous to themselves and/or others. The hallways formed a U-shape, with locked exits at both ends. There were two padded isolation rooms, into which staff placed patients who, despite medication and close supervision, could not interact safely with the others. Patient rooms lined the arms of the U, and patients were allowed free access to hallways and activity rooms along the base of the U, across from the nursing station.
Once I got used to being enclosed in close quarters with some of the sickest psychiatric patients in San Diego County, I grew to like the place. One could never be certain what human drama would be played out on a given day, and I, unlike my classmates who did psychiatry clerkships at the VA, where they dealt almost exclusively with chronically ill patients, never got bored. The dramas were not restricted to patients; one of the residents broke down and cried on several occasions during the six weeks, although I never found out why. Barry and Doug, the two students with whom I spent this clerkship, were cool customers in every respect and provided levity and humor, which were otherwise scarce. Barry had played football at Stanford; Doug, a Japanese American, had come from UC Berkeley and had paired with another Japanese American member of the class to form “The Rapping Japs,” a duo whose one and only appearance brought down the house at the traditional performance of skits at the end of our first year.
There are those who claim that the mentally ill are the only people who truly know what is going on, and some of what I saw and heard on the locked ward supported this. We encouraged patients to draw or write as a means of expressing themselves, often with stunning results. I remember one paranoid schizophrenic’s vivid drawing of a deranged satanic figure, his face laced with bright yellows and purples forming a frightful, screaming expression as an arrow pierced the middle of his forehead, yielding a free flow of bright red blood draining his life from within. Another drew a large, distorted flower of soft, wide purple and yellow petals almost as beautiful as it was peculiar. A young black woman, also a paranoid schizophrenic, produced a stream-of-consciousness narrative in which she strung the following thoughts together: “Can that Coke! Fast food. We all must die together.” She could have given dietary counseling to the patients in the coronary care unit.
Then there was a former member of the Vietcong who had recently developed some peculiar habits and no longer spoke intelligibly, in English or Vietnamese. Sporting an inappropriate half-grimace, half smile on his reddened, weatherbeaten round face, he showed us one of the least appealing of his new behaviors, that of playing with his feces immediately after making a fresh deposit in the toilet. He would kneel like a child in front of the bowl and swirl the feces with his index finger. Once in a while he would point to his abdomen and yell, so we had an internist see him in consultation. He and Bob, his medical student, ended up cracking the case by sending a sample of the patient’s stool to the lab. In that specimen, the lab found Strongyloides, a parasite that affects the GI tract, the lung, and the brain. While playing with his feces, this “crazy” fellow, ironically, was showing us where to find the answer to his troubles. My six-week clerkship ended at that point, but I learned afterward that once they treated his parasite, he transformed into a much more personable fellow, and his peculiarities vanished.
My psychiatry rotation arrived at the onset of spring, and I had the good fortune of teaming with the star among the three residents. Patti was the best, and she knew it. Bright and confident, with thick shoulder-length dark brown hair and freckles that brought a childlike petulance to her Irish face, Patti dressed in fashionable, flattering short skirts and had a way of swinging her legs up under her onto her office chair that made one’s heart skip a beat. Yes, I had a crush on her, the only time that happened during my medical education. I'm quite sure she never knew it, but there was an undeniable intensity in our interactions that I cannot attribute solely to the intimacy of our surroundings. She talked often about the golf pro she began dating during my clerkship, and I dutifully feigned interest. Though I was unattached, I thought it far too risky to pursue her, as her evaluation could affect my career, and I had promised myself I would never date a doctor anyway.
Because she was the best, her patients recovered the fastest, which meant we had to take on more new patients than the other two teams. We worked harder, so I learned more. By the time we were halfway into the rotation, I was involved in the treatment of all five patients assigned to us. Therefore, I frequently presented patients at clinical rounds with the attending and the chief resident. That’s the sort of activity that chief residents and attendings notice. I never went out of my way to impress superiors on my rotations because I found that trait nauseating in peers, most of whom didn’t do it either. On this rotation, however, I wanted to impress Patti, so when she gave me work, I did it with zeal, and I got a lot of credit.
Bob, the student who helped bring our Vietcong patient back from fecal-soiled delirium, exemplified the brown-nosing extreme. One of the least-liked members of our class, he earned his lack of popularity with his nasal voice, impertinent wisecracks, and insincerity. During our obstetrics and gynecology clerkship, Dr. Ornstein scheduled individual teaching sessions with students. A nurse practitioner prepared us for this tutorial by telling us that Dr. Ornstein always asked the question, “What is a Pap smear?" and he expected the student to answer, “It’s a screening test for cervical cancer.” During his session, Bob gave the answer, and when the doctor remarked, “I see you were appropriately prompted,” Bob replied, “No, I just read a lot.” One of our sickest patients on the psych ward, EC., a stout, 50ish, strawberry blond woman with a disheveled appearance and histrionic demeanor, was battling severe depression that resisted many of our therapeutic interventions, including counseling in various settings and medications. She also had a significant medical problem: atrial fibrillation (A-fib).
Former President Bush had A-fib. It’s a condition where the right atrium of the heart, the chamber that houses the natural pacemaker, has been damaged such that the pacemaker no longer generates a timed electrical impuLse to cause a rhythmic heartbeat. Instead, the chamber randomly flutters, or “fibrillates,” in a chaos of disorganized electrical activity, generating a barrage of electrical impulses that are intermittently and irregularly conducted to the rest of the heart. If the rest of the heart is reasonably healthy, this activity will cause it to beat very rapidly, about 120 to 160 beats per minute, a rate that greatly taxes the heart muscle and that compromises the heart’s efficiency. Doctors usually attempt to restore the heart to its normal sinus rhythm, first with medications, then with electricity. If these treatments fail, then we use other medications to control the heart.
During the course of her stay with us, I noticed that E.G’s pulse rate had risen consistently above 100, which was not safe for her in the long run. Her medication, digoxin, was not adequately controlling her rate. Because I had just finished my internal medicine clerkship and was also brimming with testosterone-driven enthusiasm, I gave Patti a detailed explanation of the problem and suggested a medical consultation, which she then requested. The internist did his evaluation, we discussed it, and then started her on verapamil, which brought her rate nicely under control. Much to my chagrin, Patti did not share my joy at this result and instead her Irish temper flared. She reproached me, saying I had used my recently acquired medical knowledge to show her up. Stunned, I tried to save the situation by professing my genuine admiration for her skills and the obvious superiority of her knowledge to mine, but I failed to convince her and over the final two weeks she distanced herself from me. At the end, she gave me a lukewarm endorsement while informing me that the chief resident and attending had, to her surprise, decided to give me an honors grade. I never saw her again.
NEW LIFE
The last clerkship of my third year, my six-week obstetrics and gynecology rotation, was, despite some very long hours, one of my favorites. I returned to the Balboa Naval Hospital, this time to a brand-new facility, and everyone was in a better mood, including me. Armed with what I had learned during the previous ten months, I reduced the rest of our team’s work, and they liked that. So they occasionally rewarded me. One day in the operating room we were doing a cesarean section, with a second-year gynecology resident as the primary surgeon and a veteran attending physician, Dr. Torp, assisting him. I held the retractors. As surgeries go, C-sections are pretty easy to do, so after we delivered the baby. Dr. Torp said to the resident, “Pretty soon, you’re going to be assisting residents who have almost no experience, so let’s practice. Jim, move over. You’ll finish the case.”
And I did. We pulled the uterus outside the pelvis and laid it on the abdomen, which most surgeons do when closing the uterus because it’s easier to sew it in this position. They showed me where to put each stitch through the soft, smooth muscle of the womb and I obeyed, following the curve of the needle (the favorite instruction of everyone who teaches surgery) with each stitch, and tying the square surgical knots at the end of each layer. For once, I was not the one to cut the threads after someone else tied the knots. It is customary for the attending physician to say one of two things to the student who cuts the suture “That’s too short” or “That’s too long.” So occasionally a student arrives with enough gumption to ask before he or she cuts the threads, “So how would you like these cut, doctor too long or too short?”
I then stitched the bladder flap over the uterus, and then the peritoneum to close the abdominal cavity. These layers (surgeons always work in and talk about layers) feel somewhat like silk, except they are smooth and moist. Next came the fascial layer, the thick layer just under the skin containing mostly yellow and white fat and having a texture just softer than tender meat. Last, we closed the skin with staples. Staples, if properly placed, allow the skin to heal as well as sutures do, and they can be put in faster, which is why they have become popular. Skin is much tougher than the tissue beneath it; I bent and ruined many a needle while learning to sew skin.
Dr. Torp did wonders for my confidence that day, and I understand she has done the same for many other students. The best teachers pick their spots; they take advantage of situations where students can do meaningful work with minimal risk to patients. More commonly, as I mentioned before, students feel very small in the operating room. It was during this clerkship that I learned of a student who a few years earlier had tried to adjust the lights over the surgeons’ heads, but he banged them together so hard they shattered. The surgeons spent hours (10 to 16, depending on who was telling the story) pulling glass out of the patient’s abdomen. I don’t think I could have finished school after an event like that.
People often ask what it was like to deliver a baby the first time, and I always confess with some embarrassment that I barely remember it, which is odd since I consider obstetrics the most important aspect of my current practice. Like most students, I wanted to deliver as many babies as I could. The timing was favorable; the academic year was ending, and the interns had done enough deliveries to be willing to let the students do a few. My first came at 3:00 a.m., when a woman whose labor I had followed and documented in her chart every two hours summoned the last reserves of her energy and pushed her baby's black-haired crown through her entroitus and out into the gloved left hand of my supervising male intern.
Delivering the head requires the most skill, as the head’s large diameter causes more damage to the woman’s body during birth than any other body part. Students generally do not get to deliver the head. “Go ahead,” the intern instructed me after he used the blue bulb syringe to suck mucus out of the baby’s mouth and nose. I gratefully and clumsily accepted the invitation to finish the job, nearly tripping over the intern’s stool as I moved in to place my hands in position, one hand above the baby’s head and the other below, to perform the maneuvers I had rehearsed many times.
With my top hand I pushed the slippery head straight down toward the floor, noting the presence of a couple of other arms extended to help should I commit the ultimate crime and drop the baby. The baby’s left shoulder, partially obscured by its mother’s blood, slid out from under the top of her pelvis, prompting the intern to blurt out, “Up!” I moved the head straight up, allowing the right shoulder to emerge from the bottom of the vagina. The other hands helped me pull out the buttocks and legs.
I wish I could say that at this point I reveled in the joy of having brought a fresh new life into the world, but a new baby really is slippery, and I was scared she would fall to the floor, perhaps ending my career. I don’t remember what she looked like, who clamped and cut the cord, or what happened after that. One thing impressed me: the sturdy umbilical cord, with its rubbery, tough, gray-white braided ropelike appearance and the three life-sustaining umbilical blood vessels twisting their course toward the baby. Just another architectural wonder of nature, brilliantly suited to its purpose as the life support to the unborn fetus. I would deliver six more babies before the end of the clerkship, which finished my third year.
CLOSE SHAVE
I harmed a patient in my fourth year.
During the weekend that separates the third from the fourth year, medical students undergo a transformation from useless slave to valued member of whatever medical service they join. All fourth-year courses were elective when I was at UCSD, and it was therefore more fun than any other year of my training. Anesthesiology was one of the electives I chose, as 1 was told I would get many opportunities to intubate patients and start intravenous lines, both of which are useful skills in emergencies. It was during my anesthesiology elective that I accidentally shaved a patient’s tooth.
We intubate a patient to allow adequate oxygen exchange through the lungs when the patient is unable to do this himself, either because he’s under general anesthesia or because he’s critically ill. Sliding an endotracheal tube through the vocal cords into the trachea usually is not difficult, and most of the time students intubated patients who were under general anesthesia and who did not present anatomical challenges and were not ill.
One morning the anesthesiology resident and I were running through the usual routine, giving general anesthesia to an elderly man who was about to undergo a minor surgery. I used the bag and oxygen mask to blow a few extra breaths of oxygen into his lungs, as we always do just before we intubate. I then took the laryngoscope into my hand. This instrument has a cylindrical metal handle with a hard plastic blade, which can be curved or straight, that you put in the patient’s mouth and then use to push the tongue out of the way. The light on the blade allows you to see the back of the throat, the posterior pharyngeal wall. Down a bit farther is the epiglottis, the pink structure that flops back and forth to allow food to go down the esophagus and air to go down the trachea. As I slid the laryngoscope into position, I noticed that this fellow had two very large upper front teeth and that these were the only teeth in his mouth. He also had a short neck. People with short necks and chins are more difficult to intubate because the trachea is farther upward (when they lie on their backs). To see the straight white vocal cords, you lift the epiglottis upward by pushing the jaw forward with the laryngoscope; if you rock backward, the blade comes into contact with the teeth. I had to pull pretty hard to see the vocal cords, and I must have inadvertently rocked back. After I pushed the inflatable cuff of the endotracheal tube to its destination just past the vocal cords and looked down at the blade, my eyes met the two front teeth sticking out like shiny gold and white targets. The blade rested against the right tooth, and a quarter-inch-long white shaving, looking much like one would file off a hard white metal, dangled from the edge of the tooth. The attending anesthesiologist noted the look on my face, came over, surveyed the damage, angrily snatched the blade out, and blurted at me, “What are you doing?” He looked at the tooth again and said to the resident, “It looks okay, but we had better get a dental consult just to be sure.” He then turned to me in disgust and muttered, “Be careful, would you?”
My fear that I would do harm to someone had finally been realized. The damage was minor, but I felt terrible for days. We do have to be careful, with everyone, all the time. It is probably too much to ask of human beings so we have to learn to forgive ourselves, even when patients do not, although they usually do. No one at UCSD discussed the idea of forgiving oneself for mistakes; I did not learn to do it until my residency.
WHY CHARLIE?
To what extremes could our often reckless approach to education take us? Hard to say, but what our classmate Charlie did made me think about this for a long time.
I met Charlie in late 1985, when we both took an elective in clinical hypnosis. To dramatize the difference between using hypnosis constructively and using it for entertainment, many of us went out one evening with our professor to take in Dr. Dean’s show, in which he used hypnosis on members of the audience to entice them to perform various outrageous stunts. Charlie came with Bet, his 27-year-old wife of four years, whom I vaguely remember as a serious but pleasant individual; he seemed content and easygoing. She worked two jobs to support him through medical schooL For the next three years, my infrequent encounters with Charlie involved only the occasional exchange of routine pleasantries. In early December of 1988, Charlie spotted Tracy, a classmate and lifelong North County resident who now practices family medicine, in the medical school parking lot and shouted out a friendly greeting. Tracy said this struck her as somewhat odd, since they had rarely spoken to each other. Charlie rushed over, informed her that he had become a daddy, and proudly showed her pictures of the new family member. Tracy felt genuinely happy for him, as he seemed thrilled with his lot in life. Stories in the San Diego Union later described him and Bet as “the ideal couple,” going on outings together and attending neighborhood barbecues and other family-style events.
I left for a ten-week working vacation in Nairobi, Kenya, in late December 1988 to do my required research project. When I returned, a classmate informed me that on December 20 Charlie had allegedly strangled Bet with a telephone cord in the laboratory where she worked. He had taken out a $100,000 life insurance policy on her just four months earlier. He became the primary suspect during questioning about his wife’s death when he showed little emotion. Investigators also noticed a scratch on his chest that looked like a fingernail injury and something on his right little finger that suggested struggle with a cord.
Turbulence in relationships between my classmates and their spouses/significant others was not news. Several marriages ended during our four years, and many more long-term relationships broke off, as the constant duress of long study hours and sleep deprivation drove apart all but the most stable partnerships. I would not have suspected that anyone in our class would be capable of killing his or her spouse, and Charlie would not have topped my list of possible candidates.
Because this happened in the middle of our last year of school, during which time we did not get together as a class until graduation day, it’s difficult to say what effect this had on the class. Everyone I asked seemed as surprised and unsure of the tragedy’s meaning for us as I was. We graduated long before the trial, and from my recent conversations with members of our class it seems that most of us never found out what fate finally befell Charlie. He maintained his innocence at the beginning of the trial and even remained close to his deceased wife’s family until about halfway through the trial, when he changed his plea to guilty. He plea-bargained his charge to manslaughter,' resulting in a 12-year prison sentence. He was only six months away from earning his M.D. and practicing medicine.
Medical school, and residency after it, attacked us where we were most vulnerable. We confronted death, nudity, blood, and disease while our schedule and teachers denied us the sleep and self-esteem that are so important in keeping oneself grounded while surrounded by emotional chaos. Traditionally, medical teaching institutions have neglected the emotional growth and education of their students, claiming that extreme conditions of sleep deprivation and hard work build better doctors. Most of the faculty and almost all my supervising interns and residents at UCSD knew the absurdity of this philosophy and tried to help the medical students survive the clinical years without mental breakdowns. Some of our most accomplished faculty had left the intense academic atmosphere of other medical schools, particularly those on the East Coast, for the more relaxed atmosphere of UCSD. A few of them confessed to enjoying students and granted us the same courtesy and empathy they showed patients. But I hope that Bet didn’t die completely in vain and that changes in policy to improve the treatment of students ensued.
I left UCSD much the same as I had entered, except that I had less tolerance for shallow banter and small talk, making my personality seem more serious and intense. I think this happens to most of us in medical school. After completing a three-year family practice residency in Maine, I now have a four-year-old private practice in Berkeley, where I do the full range of family medicine, including obstetrics. Fifteen to 20 patients walk into my office, a converted red brick house just outside of downtown, every day with earaches, depression, acute heart attacks, sprains, memory loss, and just about anything else that can happen to a human being. Most speak English or Spanish, but many come from places like the Far East, the Philippines, and Africa. Once in a while I get to use the French I learned while working in Belgium for two months the year before I started at UCSD.
In an attempt to distance myself from the hierarchical structure of medical school, I have left my white coat at home since the day my residency started; this fall, I sent it to the Goodwill. I teach physician’s assistant and nurse practitioner students in my office twice a week and try to make them feel comfortable and competent, because I remember.

During the first year of my residency in family practice in Maine, I came home to Los Angeles for Christmas. The climate switch in the seven-hour cross-country journey, from minus 10 to 86 degrees, didn’t trouble me as much as the prospect of getting together that evening with friends I had not seen since high school As my brother John and I drove south toward the floor of the San Fernando Valley, I posed the unsettling question.
“Since before I went to medical school, do I seem different to you?”
He reflected a few moments. “You have joined a kind of fraternity. You have been places the rest of us haven’t. There’s a part of you that the rest of us don’t know and may not understand. That puts some distance between you and us. But you still seem pretty much the same to me.”
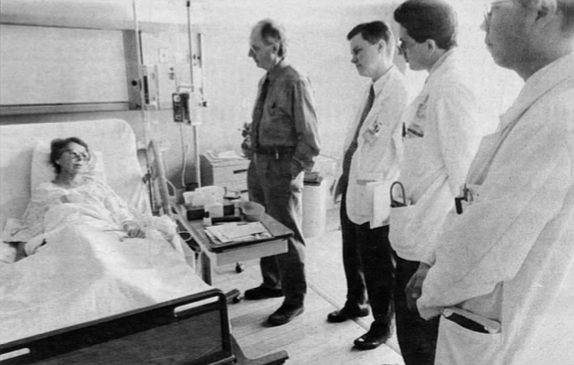
More than 3700 college graduates had applied to enter UC San Diego’s School of Medicine class of 1989. UCSD invited 230 to spend the next four years at one of the finest schools in the country; 122 of us accepted the offer and arrived in La Jolla in September 1985.
Why were we chosen?
I had wanted to be a doctor since graduating from elementary school; I never seriously considered anything else. I did not have any doctor role models in my immediate family, but my chain-smoking, wisecracking, New York-bred pediatrician impressed me, as my mother trusted her more than anyone. For example, my inability to consume an entire cookie at age eight concerned my mother, as I was quite skinny then, even more so than I was upon entering med school, but Dr. Mont’s advice reassured my mother. So, in the manner of a great many premedical students before and after me, I had applied myself in a focused fashion to earning the Greek and Latin distinctions (Phi Beta Kappa, magna cum laude) and high numbers (3.8 GPA from Pomona College and a 10, two 11s, and three 12s on my Medical College Admissions Test) that would allow me a chance to obtain my M.D. To eight schools I had presented my credentials, my slender six-foot, four-inch frame (befitting my Dutch heritage), my similarly lengthy convex nose (Jewish ancestors contributed this), and my sincerest pledges to benefit mankind. UCSD extended the invitation and now, at age 22, my time had arrived.
Accompanying me was a diverse collection of individuals, including carpenters, philosophers, athletes. Mormons, Muslims, Catholics, Vietnamese, and Iranians, from places like Stanford, Harvard, Yale, and UCLA. We shared a common trait, which had written our admission ticket to UCSD: our proficiency as test takers. We had mastered the “art" of absorbing huge quantities of information in a short time and regurgitating it onto an examination paper. One might hope that, since we would become some of the most trusted members of society, whose daily decisions would profoundly affect people’s lives, we would also have distinguished ourselves with our honesty, reliability, and sound judgment.

Well, we had not and did not. Once during the first two years, our faculty announced they knew some of us were cheating on exams. They had us fill out an anonymous survey that asked if we had ever witnessed our classmates cheating. I never had, but after one exam my roommate, a test-taking star among stars who seemed out of sorts that day, confided that someone had looked at his answers. The faculty tried from the beginning to downplay competition, emphasizing that they considered each of us an “honors” student, and therefore all courses were graded pass/fail. (From this, we students derived “The Golden Rule of Medical School”: P = MD.) They shot themselves in the foot, however, by including “honors” and “low pass” distinctions in each course, which ensured that the incurably competitive would compete. Many of us competed just within ourselves. Others argued heatedly with professors during post-exam reviews about the fairness of questions answered incorrectly. Some, apparently, resorted to other means to improve their chances. I don’t think the faculty ever caught or disciplined anyone for cheating.
In many ways, we first-year students acted no differently than our undergraduate counterparts at UCSD. In fact, their professors provided almost all our first-quarter lectures in biochemistry and molecular biology. Our corner of the campus, its expansive, lush green lawns surrounding the gray-and-white concrete walls that enclosed our lecture halls, labs, and library, stood apart from the rest of the campus but did not particularly distinguish itself.
Our approaches to learning differed. Some of us attended every lecture, which during the first quarter meant eight hours of class three days a week and four hours the other three days (Saturday included), while others never attended unless it was mandatory. Many who showed up every day bored whoever would listen with complaints of long study hours; others would go to great lengths to hide the number of hours they spent over the books. The quantity of material we had to memorize required that we all work hard, but most of us found time to enjoy life in San Diego. I took a sailing course at Mission Bay in the spring, and many classmates pursued similar outdoor interests. We played intramural football, soccer, basketball, and softball and always finished at or near the top of the standings. Those of us just out of college threw parties, where we drank heavily and danced to “modern rock” (e.g.. Clash, Talking Heads, New Order).
I spent much of my spare time with a few single men in my class doing what they enjoyed doing: going to bars (the Elephant Bar, Carlos Murphy’s, the Belly Up Tavern, and others) to drink, dance, and pick up women. The latter, for me, was always a vicarious experience, because I never succeeded in picking up anyone at a bar (I stopped trying in 1986); several of my friends almost never went home alone. This was pretty frustrating; I remained a virgin until December 1987, narrowly averting a celebration of a quarter century of celibacy at my birthday party three months later. But my experiences in the bars of San Diego helped when I began my hospital clerkships at the start of my third year, because as frightening as a cross-examination by an attending physician could be, it never intimidated me as much as the women in the bars.
Other students led more responsible lives with spouses and children. We were 85 men and 37 women: two were married to each other, two were engaged but later broke up. We averaged 26 years of age. Most of us lived in the graduate student housing (“the ghetto" of La Jolla) east of campus; the apartments had modern kitchens and large rooms for about $150 per student per month. I couldn’t get in there the first year and a half, so I found a room in a Pacific Beach apartment with a 33-year-old divorced dental hygienist just recovering from leaving her alcoholic husband. We had grown up in the same San Fernando Valley town but had never previously met. Her closely cropped brown hair and pleasant personality did not prepare me for her quirks related to tidiness, one of which required that all utensils used to prepare meals be cleaned before I sat down to eat. This didn’t cause problems until I severed three ligaments in my left ankle during a basketball game and subsequently underwent surgery, after which I wore a cast on my ankle for six weeks. One evening, after a draining day at school, I limped around the kitchen to prepare my dinner and then dared to sit down before cleaning out the pans on the stove. She threw a fit, unimpressed by my crutches, sad dark eyes, and imprisoned lower leg. Other than that, I liked her. But when a classmate called with news that a college friend of his had just moved to San Diego and needed a roommate, I did not hesitate.
Perhaps the most important perk to many of us was the low cost of a UC education. When I started medical school, the annual tuition at Georgetown University in Washington, D.C., had reached $25,000. Georgetown represented the high end of the price range, but most private schools checked in at well over $15,000 annually. The University of California’s cost, about $500 per quarter, saved those who lived in California when they enrolled nearly six figures of debt over the four years. Almost all of us entered med school with an undergraduate debt load; mine totaled about $7000. To minimize my debt, I worked part-time as a typesetter for the Guardian, UCSD’s school paper, during my first two years. Four years later, I graduated $30,000 in debt; many of my present colleagues who went to private schools had debts ten times mine. Doctors who are just starting out, often after buying a practice, are commonly faced with a debt load approaching half a million dollars before they see their first private patient.
Some among us had a head start: born in Beverly Hills, educated in Ivy league schools on their parents’ accounts... one drove a Porsche. He was the youngest of our class (20 years old in 1985) and had a charming exuberance that endeared him to most of us. His entire immediate family died in a plane crash during our third year. Enough catastrophes confront third-year students to test their sanity limits anyway, so I admired Derek for the way he handled the most tragic event to happen to a class member in our four years, never losing his kind, gentle manner. The last I heard he had finished his pediatrics residency.
We had your typical dwarfish, rotund Yale grad with round, rimmed glasses covering owlish eyes, who would commemorate the end of many a lecture with an indecipherable question about some obscure detail that neither the professor nor any of the rest of us cared about. Another otherwise likable fellow had the same annoying habit, although his questions generally maintained a relevant thread. Many of us left the auditorium between lectures while those two finished their business.
Truthfully, most of what happened during the first two years bored us at the time and isn’t exciting to recollect here. Gross anatomy broke the routine. Taught during the first year at most medical schools, anatomy opened the second year at UCSD, immediately preceding the pathology (study of disease) courses.
Anatomy carried an aura of intrigue. Legends, the truth of which purveyors of the oral “history” were never quite sure, were part of course orientation. One tells of a student who borrowed part of his male cadaver to take to the local movie theater. After entering the restroom of the movie house, he strode up to a stall and hurriedly took care of his business. Upon finishing, he frantically yanked up his zipper, paused, and then let out a long howl and ran from the bathroom doubled over in mock pain, leaving “his” penis on the floor, to the horror of the old fellow using the adjoining stall. Another tale claims that a medical student startled an East Coast toll collector by handing him a pair of testicles in lieu of the usual fee and sped off. There were countless others.
The atmosphere added to the aura. A distinctive formaldehyde stench greeted the nose of everyone who wandered into the basement lab, where the 30 or so preserved bodies rested on dissecting tables under drop cloths. The cool, windowless laboratory featured blocklike workstations with sinks and drawers of typical lab design. It also featured laminated specimens of preserved human structures, including cross sections of the abdomen (about an inch thick) and a human skeleton. With classmates present and in the context of learning, most of us enjoyed the class, but the few times I went down there to a study session at night, the air was heavy with death’s stale, penetrating odor, and upon exiting into the still, black night, my body couldn’t suppress a shudder or two.
Dr. Halasz, a Greek general surgeon with a bushy gray mustache, ran the course. While students dissected cadavers, five or six professors roamed among us. Dr. Laurenson, a poetic Canadian, complete with beret and wry wit, always kept things in the proper perspective (when asked for advice before the first exam, he counseled us, “Always drive the Mercedes”). Dr. Wilson, a soft-spoken, gentle, matronly sort, periodically suffered attacks of Meniere’s disease, a poorly understood inner-ear condition causing intermittent attacks of severe dizziness and nausea, but she rarely complained while detailing the development of bodily structures from their embryologic origins. Dr. Breisch, a young New Jersey stud who dazzled us with knowledge and tall hunting tales, didn’t publish enough research, so despite his unusual gift for teaching, the university served him his walking papers after he finished with us.
Dr. Halasz began the introduction to our cadavers with a philosophical discussion of the difference between human bodies and human “remains”; drawing such a distinction made our work easier on the conscience, although once we started, the task at hand often made us forget that we were cutting up dead people. We divided into teams of four. My team’s “remains” had belonged to a woman who was about 90 when she died. All teams named their cadavers; we could not come up with anything we felt appropriate, so we respectfully called her "Ma’am.”
I do not remember much about the dissection, except that dead tissue almost always had a very tough and leathery feel to it, which I later discovered contrasted with the soft, elastic, and sensual fullness of living tissue. My only prior exposure to a dead human was six years earlier after my girlfriend’s father had dropped dead of a heart attack at the dinner table. I recall peering into his open casket and noting how peaceful he looked. What I really saw was the absence of color and expression that life gives a face.
While we worked on the bodies, the cadavers’ heads hid under wraps. Before their unveiling. Dr. Halasz called us together to prepare us. He explained that life brings a tremendous amount to a face, and that fact never is more evident than when one looks at the faces of the deceased, for they all look remarkably alike. Much of our unique appearance dies with us. I had trembled when I thought of slicing into Ma’am’s face, but death had stolen her human qualities. The warm, gentle, grandmotherly countenance I had expected wasn’t there; the vacancy of death had replaced it. Within a few minutes of making the first incision into her cheek, I once again immersed myself in learning.
Each of our examinations in anatomy had a written component and a lab practicum component. For the latter, the faculty would label parts of our cadavers with numbers and ask us to name the parts. During our first exam, I noticed that many students were taking longer than usual to look at one item, and when I arrived, I understood. Before me rested an amorphous body part, separated from the cadaver, lying sprawled out, limp, and composed mostly of soft, oily, yellow globs of stuff (fat). After 45 to 60 seconds, I walked around the specimen and found the skin over the front, at which time it dawned on me that I was looking at a female breast. Why anyone felt the need to detach it completely to label one of Cooper’s ligaments, which support the breast. I’ll never know, as I have never since had to identify one without a woman attached. I later noticed a bumper sticker in the lab that read “Parts is parts.”
Stuff like that took much of the human empathy out of the first two years of medical school and made it challenging for me and others in my class to maintain the focus of what this was supposed to be about: taking care of living human beings. Amongst the memorization of often trivial facts and the obsession over examination scores, glimpses of patients were rare until our Introduction to Clinical Medicine courses, which began in the winter quarter of the second year. This was our first chance to put on white coats and use stethoscopes and other tools of the trade on a semi-regular basis.
A fourth-year medical student, Bill, taught the physical examination we would perform on patients our third year. He showed us everything except the gynecologic exam; nurse practitioners taught that, using themselves as models and subjects for our first exams. For everything else, we practiced what we learned by examining fellow students. Each of us chose a partner. The couples in class had an advantage, as one learns more by practicing with a member of the opposite sex. I don’t remember much about these sessions, except the part when Bill told us that the exam involved inserting the index finger into the patient’s rectum, feeling the anatomy within, and extracting a lump of shit to wipe on a card, onto which we then dropped a clear liquid that turned blue if the “sample” contained occult blood. They spared us the indignity of doing this to one another.
Soon we began to practice our newly acquired skills on hospital patients. I found myself trying to behave as I believed a doctor would, thinking that would reassure the patient that I knew what I was doing. Perhaps this is why some doctors never stop presenting themselves to patients in a way that implies the doctor knows more than he or she really does.
My first patient, an attractive and pleasant 51- year-old blond woman with a fair complexion and crippling arthritis, treated me with an almost motherly kindness and respect. Sporting white coat, button-down shirt, and tie, I made my best effort to present myself professionally, and I managed quite nicely through the lengthy interview and the examination of her head and neck. This despite the inconveniently low height of the hospital bed she sat on, which was causing my back to ache in a way I could barely conceal. I then proceeded to examine her breasts, and at first this went well; neither of us seemed ill at ease as she sat bare from the waist up and 1 hunched over trying not to create any impression that I could think of her as a sex object. But women still made me nervous, and suddenly my antiperspirant and every other antisweat mechanism in my body gave way. I had to sheepishly excuse myself to dry my soaking-wet face and neck with a handful of paper towels from the dispenser above the sink. My recollection is that she thoughtfully offered some comment about the heat in the room (or maybe I did), as though we had suddenly transported ourselves from the San Diego winter to summer in Death Valley. I felt very much the naked emperor in front of my half-naked patient. Her grace, not mine, allowed me to finish, and my thoughtful write-up earned high praise from my preceptor. We doctors all have patients we owe for what they teach us about our profession and about ourselves; I’m eternally grateful to that woman.
I overcame most of my anxiety about examining women quickly, thanks to the nurse practitioners who so calmly allowed us to perform pelvic exams on them and taught us how to do so thoroughly and gently. Women wonder what goes through our minds when we touch their genitals, insert instruments in their vaginas, and probe their insides with our fingers. When we’re just starting out, I think most men feel as I did. I feared that my women patients would think I was having fun at their expense, and this made me nervous enough to sweat and far too nervous to have any sexual fantasies. On a few occasions, when my fingers would slide into a vagina that had unusually profuse lubrication, my stomach would gnaw at the thought that the patient was having more fun than I was comfortable sharing.
Later, as I grew more confident and understood better what I was doing, I found that the concentration required to do the job generally precluded any nasty thoughts. I examine women of all shapes, sizes, and ages, but what determines how I feel about the exam is their maturity and self-esteem. Good hygiene helps, but I can work through even the most nauseating of odors. Examining women who are comfortable with themselves is easy, no matter how they look. I would be lying, however, if I claimed that looks do not matter. It is easier and more pleasant to do a thorough exam on an attractive person, just as it is easier to look at one. If a woman looks and smells terrible, a careful exam is more difficult to do, although many of us, myself included, are aware of this and make a special effort to take enough time with such patients. Women who are suspicious, nervous, or unable to suppress giggles present a challenge, but my nine years of experience have given me enough composure that I cannot remember the last time I or a patient had emotional difficulties during a pelvic exam. Many women have an easier time with female providers, but some prefer a male physician; I’m not sure why that is and I would like to find out. In any event, for me and most of us, once we overcome our fears when we are rookies, we’re just doing our jobs when we examine women. Our patients do enter our fantasies once in a while (and we enter theirs), but it’s rare and, for most women, not worth worrying about (in my male opinion).
Perhaps this is the time to mention that pornographic movies were a part of our core curriculum during the first year. The idea was to confront us with different sexual orientations and experiences so we could deal with our reactions before patients challenged us with their “lifestyle-related” problems. Despite much anticipation and preparation (many of us came to class that morning with popcorn and Milk Duds), the event disappointed me. The films showing male and female masturbation, gay males, and lesbians didn’t have any plot or character development, and consequently didn’t offer much to those of us who had lived in urban areas. By far the most stimulating of the offerings involved a heterosexual couple in their 60s, which, as my oldest (33) classmate pointed out, gave us hope for our future. The advertised video of a young heterosexual couple was not available; too bad for those who came to class hoping to learn something new.
After two years in the lecture hall and laboratory, we spent two days answering the 999 multiple-choice questions on the National Board of Medical Examiners’ Examination: Part I. This is the first and toughest of the three National Board examinations one must pass to qualify for a medical license in the United States. We take Part II during the fourth year of medical school and Part III at the close of our internships. The completion of Part I marks the end of daily treks to the lecture hall and the beginning of hospital clerkships, where we finally begin to take care of patients. Unlike the first two years, when we all share pretty much the same experiences, the class separates during the clinical years, never meeting as a whole again, and each of us has a highly individual experience. The following vignettes give some details of mine.
MR. CLEAN
The month of August 1987 brought me to my first hospital clerkship: neurology at the VA Hospital. My only previous exposure to medical neurology came during the spring quarter of our first year in a basic neurology course, the most interesting course of the least stressful quarter of the first two years. No organ surpasses the brain for complexity and intrigue; learning how the brain works and how each area exerts its influence fascinated me. Of course, one cannot deny the macabre nature of cutting up and studying brains, as we did in neuroanatomy lab. Our favorite neuropathologist, a cheerful and engaging British chap, Dr. Powell, led us through the ceremonious “Brain Cutting” sessions, in which he unlocked the mysteries kept within the brains of persons recently deceased from or with neuro-logic diseases. Boyish in appearance due to his short stature, despite his middle age and white coat, his enthusiasm captivated his audience of 10 or 15 students, interns, and residents. We were seated above him on several rows of wooden bleacher seats in the tiny theater downstairs. Carefully he sliced the brains into thin sections in the manner of one preparing a fine salmon loaf. Thusly he demonstrated the atrophied cortex and mammilary bodies (the “breasts” of the brain) in the alcoholic, the compromised substantia nigra (an area of “black substance”) of Parkinson’s disease, and other abnormalities of such regions as the “pale globe” (globus pallidus), the “tail” (caudate), and the “almond” (amygdala), all of which resemble their namesakes.
We spent more time with live patients. People with neurologic problems, particularly those localized to specific areas of the brain, can be interesting and sometimes cruelly entertaining to study and observe. Oliver Sacks describes extraordinary cases in his books, but I had not yet read these, so I was unprepared for what I encountered.
Adam and Paul, two witty transplanted Ivy Leaguers, were my partners for our four-week neurology rotation at the “Va spa,” the euphemistic nickname we physicians in training gave the Veterans Administration Hospital in La Jolla. Although it is one of the newest and nicest of the VA hospitals, one would never willingly stay inside long. It features cheerless, faded gray-white hospital corridors, interrupted by outpatient waiting areas crowded with the day's patients. Interns, medical students, and other hospital personnel, some responding to operators’ messages resonating from the intercom, passed quickly by patients strolling the halls in hospital gowns, pushing IV poles with bags of yellow urine from the Foley catheters wrapped around their legs. Paul dressed up as a veteran at our Halloween party that year, complete with gown, Foley, and cigarette. His and Adam’s senses of humor, laced with cynicism, helped get me through what was otherwise a dreary month.
Among other things, most veterans learned to smoke and drink in the military, and the “spa” was where they were treated for the consequences.
We frequently revisited the subject of alcoholism during our month on the neurology ward because of the academically interesting and humanly tragic effects it has on the brain. One patient, J.M., suffered from Korsakoff s psychosis, a condition in which the ability to form new memories is destroyed. To compensate, affected individuals confabulate, which renders them interesting interview subjects. When asked, “Do helicopters eat their young?” a patient with Korsakoff s might answer, “Only when they’re hungry.” Paul thoughtfully asked J.M., who was sitting with several other demented patients one afternoon during lunch, “Would you like some grapes, Mr. M.?” The pale, wheelchair-bound gentleman reflected for a moment before replying, “No thanks. I just had a bar of soap."
More sobering were the stroke victims. Veterans, because of their smoking habits, frequently acquired during the years our government provided servicemen with free or cheap cigarettes, often succumb to complications of atherosclerotic disease, which clogs the arteries. Heart attacks and strokes are common examples of these complications.
One tragic case was an elderly gentleman who had already lost the function of his left arm and leg from a previous stroke. He came to us because he had suddenly lost his ability to make new memories; he forgot within a minute anything that happened to him. He did not show any other new deficits in his sensation abilities or in his movements or reflexes. An alarming scenario for him and his more youthful brunette wife, this was a particularly curious one for us, because sudden isolated memory loss is rarely seen; most memory loss, such as that of Alzheimer’s disease or Parkinson’s disease, occurs gradually. It is puzzles such as this that attract neurologists into their specialty, because for most neurological syndromes there is a logical answer awaiting the clever doctor/detective. In this case, we tracked down the head CT scan from his previous stroke, which showed an impressive dark discoloration of much of his right hemisphere typical of a stroke affecting the right middle cerebral artery. The attending neurologist looked it over thoughtfully and came up with the solution. The first stroke had affected the hippocampus, one of the key memory centers, but only on the right side. Stroking out the hippocampus on one side often fails to produce any measurable memory deficits, but if you knock out both sides, you get profound deficits. A CT scan several days later confirmed the diagnosis: a new stroke affecting almost exclusively the left hippocampus. Why didn’t it show up on the CT done the day of the stroke? Because nonhemorrhagic strokes do not immediately show up on the scan; it takes about 48 hours for the dead brain tissue to lose enough density to be visible on an x-ray.
As is often the case with neurologic disease, once we solved the puzzle, we could not do much for the patient. He now not only could not use half his body, but he could not remember that fact or almost anything else, which led to frequent, dangerous attempts to get up and walk that always ended with him on the floor. He was one of the cases that convinced me that 1 would not become a neurologist. I value recovery from illness much more than the thrill of the diagnostic chase.
FRESH AIR
Changing venues from the VA neurology ward to Children’s Hospital was like moving from Detroit to San Diego. Optimism, a rare commodity at the VA, overflowed at Children’s. The pace and energy of the place picked up the spirits of many disgruntled students who wandered in after four weeks of slow-moving patients at the VA.
Our workload also picked up a bit, including overnight call every fourth night. Early one evening on call, I admitted to the medical ward an asthmatic dark-haired, chubby-cheeked Mexican boy, about 14 months old. At that age, one has a well-developed sense of fear and a need to protect oneself from the unknown, so imagine being dragged in that frame of mind into a large, unfamiliar building full of strangers, many of whom are trying to probe you with needles to fill your veins with antibiotics and theophylline (a caffeine-like medicine that opens bronchial tubes) or blow cold mist (containing oxygen and bronchodilators) into your face. All of this is happening while you feel as though you are drowning: you can’t get enough air. So this little boy made no effort to hide his feelings about me or my attempt to examine him. He screamed. He punched. He kicked. He bit. We prevailed. I left him to his mother, his nurse, his medication, and his breathing treatments and continued my evening’s work with other patients.
Several hours later, after his mother had left for the night, I dared to venture back into his room to check on him. I intended to listen to his lungs and hoped that if I approached slowly his protests would be mild enough to allow me to do so without bringing in Marines to help. As I approached, he stood up in his crib and gripped the vertical metal bars in a pose that was becoming familiar to me on the pediatric ward: that of children doing their time until they were fit to be released into society. He began to cry as I raised the upper bars to reach him, but I was able to press my stethoscope against his back to listen, noting that the wheezes and other adventitious musical sounds were louder than previously, which meant he was moving more air into his lungs. Then, the unexpected happened: as he cried more loudly, he stretched his arms out toward me with an expression of terror on his little face. I let out a big “Aw.. picked him up, rocked him in my arms, and told him he really was going to be okay. This was one of the few moments of pure human sweetness I would be allowed during my third year of school, and I enjoyed it fully. After a few minutes, I had to leave and replaced the crying child into his little cell-like crib.
In retrospect, I wonder which of us benefited more from that encounter. For me, it was one of the defining moments of my career, it helped convince me that my choice to'become a primary care physician, a family practitioner, was the right one. The little boy recovered and went home two days later.
BOOMER AND THE BROOMSTICK
We all dreaded our 12-week surgical clerkships. Workdays of 14 to 20 hours were routine, and the stories of student abuse made many of us hit the antacids before we started. Later we discovered that some surgery residents drank Mylanta or Maalox during morning rounds.
One brilliant attending surgeon, who enjoyed a worldwide reputation for many reasons, earned most of his notoriety on campus with his blatant disrespect for students, particularly women. “Medical students are like undescended testicles,” he used to say, only partially in jest. “They are always late, and when they arrive, they are useless.”
“You are doing the work of two people,” he informed one exhausted student during a lengthy operation. “An idiot and an asshole. Pretend like you are trying to help me.”
To him, any female student was named Veronica, that is, when he wasn’t calling her his favorite nickname: sexpot. “You are only good for one thing,” he would frequently remind his current Veronica during surgery. And if Veronica happened to be holding the suction when he needed it, he would demand of her, “Suck me.”
Hospital rounds were no picnic either. He did not trust students to say anything to his patients. If a patient asked Veronica, “What time is it?” she was expected to answer, “I don’t know. I’ll have to ask Dr......
Knowing his reputation, I knew I wanted to do my six weeks of general surgery where he would never find me: the Balboa Naval Hospital. I got my wish. I could never stomach a long-term relationship with a military institution, but I’m grateful for the six weeks of grueling work, relentless questioning, ridiculous hours, and minimal sleep I spent there. The residents and attendings (attending physicians) valued my presence and my work and made sure I learned something.
As I had expected, the patriarchal structure of the military resulted in a male-dominant atmosphere the testosterone-laden dialogue often seemed more appropriate for a locker room than a hospital, and I occasionally felt more like a member of a high-school basketball team than of a surgical team. Boomer, the chief resident of our team, had the boyish face and pouting lips to match his nickname and a coach’s penchant for lectures about teamwork and motivation. Of the three chief residents. Boomer headed the class, with an extensive fund of medical knowledge, excellent clinical judgment, and supreme self-confidence. I had none of that and assumed the role of “raw young pup,” as Boomer later remembered me.
Our schedule ran in three-day cycles: one day admitting surgical patients to the hospital (pre-op day), one day in the operating room and one day in outpatient surgery clinic. Every day began at 5:30 a.m. with work rounds, when we would see patients who were recovering from surgery, determine their condition, formulate that day’s treatment plan, and then, in my case, have the plan shot down by the chief resident. On pre-op days, we would then get our assigned patients, perform their histories and physical examinations, write them up, and get ready for pre-op conference in the afternoon. At these conferences, medical students and interns presented the patients admitted that morning for surgery, and then answered a three-hour barrage of questions about them and their medical conditions. Our attending physician, Captain Carlisle, chaired the afternoon sessions.
One afternoon I presented a patient who would be undergoing a vein-stripping operation to treat painful varicose veins caused by abnormalities in her venous circulation. This led to a discussion of venous anatomy and circulation. After the usual review of the anatomy of deep veins, perforating veins, and venous valves, Captain Carlisle took a more personal approach. He turned his bald head and dark gray mustache to launch his deep, booming, staccato voice
“Just exactly where is the greater saphenous vein, James?” he demanded. An easy question to answer.
“It runs over the medial malleolus...”
“Show me YOUR saphenous vein, James!”
I felt a pounding at my temples, heralding the onset of one of my frequent migraines, as I quickly, though reluctantly, pulled up my left pants leg to demonstrate my easily visible vein.
"Not everyone's as large and obvious as yours, but remember, it is ALWAYS there. When you need venous access [to give intravenous fluids in emergencies] immediately, it is ALWAYS there.”
Point taken. Although I had unpleasant visions of future conferences (e.g., “Show me YOUR genitals, James!”), Captain Carlisle never repeated this tactic.
On operating days, we would go from rounds to the operating room. Two residents and the attending physician usually performed the operation; my job was to pull consistently and firmly on retractors so they could see, while I could not, and to field questions about the anatomy that seemed always just out of view. Later in the day, the number of surgeons would diminish, and one assistant for a lone surgeon, usually Boomer. These were the real learning opportunities.
One night we got a call from the emergency room. A young midshipman had come in complaining that he had sat on a broomstick and, much to his chagrin, it had broken, and he couldn’t get the stick out of his rectum. This being a military hospital, it became apparent to me that the retained broomstick probably represented far less a problem than the disciplinary measures he would almost certainly face because of this closet-betraying incident. After Boomer and I rummaged through the operating room supply areas to find tools to retrieve the mislaid stick, we entered the OR where the cowering, terrified 'patient lay on his back with his legs elevated (in stirrups, I think). I can’t remember his face, just the feeling in his expression. A couple of pushes on his abdomen resulted in a colonic spasm that delivered the stick within easy reach of the anus, so Boomer just pulled it out. Elated at the ease of the procedure, and with his glove covered with shit, Boomer couldn’t resist offering his suffocatingly malodorous hand to the OR nurse, saying with an impish grin, “Damn glad to meet ya.” He then went up to the young victim and sternly warned him, “This time, you were lucky, but don’t let anyone find you doing that anymore.”
The next morning, I got a good look at the downside of staying up most of the night in the name of education: I slammed into the rear of a four-door sedan that had suddenly stopped in the fast lane on I-5. My car fared worse than either driver, and my insurance company paid for the damage. To this day, that remains my only accident.
THE PUMP ROOM
Sleep deprivation didn’t become a way of life until my three-week introduction to cardio-thoracic (CT) surgery. The workday began at 4:30 a.m. and ended at 10:30 p.m., and if you happened to be on call that night, you didn’t even get those other six hours off. But believe me, when you get inside a living person’s chest cavity, staying awake is not a problem.
Nothing one experiences, neither in the first two years of medical school nor in ordinary life, prepares one to enter the realm of such things as cardioplegia and extracorporeal oxygenation. I had never witnessed the beating of a human heart, the inflation and deflation of human lungs, or the bony cage of human chest wall within which this life-defining activity ceaselessly continues. On my first day I was led into the operating room to the area just above the patient’s head, where the anesthesiologist resides. A second-year surgical resident was cracking open the patient’s chest, buzzing through the sternum with something similar to a Black & Decker circular saw. The vital structures quickly came into view.
Then the fun really began. The surgeons inserted a large cannula (tube) in the aorta and another in the vena cava, thus bypassing the heart and lungs and directing almost all the patient’s blood to “the pump,” within which the blood exchanged carbon dioxide for oxygen, a task normally handled in the lungs. This is extracorporeal oxygenation.
No one had briefed me on the details of cardioplegia. I did my best to maintain an ostensibly curious, calm, and interested demeanor, while my surgical mask hid my gaping jaw, as the surgeons stopped the heart and cooled the body to four degrees centigrade (39 degrees Fahrenheit). This “cooling down" diminishes the body’s requirements for oxygen and nutrients, giving the surgeons time to accomplish a heart operation, such as bypassing dogged arteries to the heart or replacing a defective heart valve.
The warm, wet odor of the open chest took me back to the dog labs of the winter quarter of our first year. These labs demonstrated some of the principles of cardiovascular physiology and pharmacology that our professors had described during lectures. The dogs we worked on had come from the animal shelter, where they had escaped immediate execution by volunteering to be our helpful subjects. Senior pharmacology students and others who administered the laboratory course anesthetized the dogs deeply, intubated them (placed a breathing tube down the trachea), hooked them up to a respirator (breathing machine), stuck pressure transducers into one of the large arteries to give us accurate graphs of each dog’s blood pressure, and inserted an intravenous line through which the lab assistants could give medications. I vividly remember our dog volunteer, a young German shepherd, whose little heart beat like a machine gun when we injected it with norepinephrine, epinephrine, or isoproterenol, all of which are powerful stimulants of the sympathetic nervous system. The point of the exercise was to demonstrate that norepinephrine acted on sympathetic nerve receptors in such a way that the heart rate, systolic blood pressure (the pressure during the heartbeat), and diastolic blood pressure (the pressure between heartbeats) would all rise; epinephrine stimulated a slightly different subset of receptors that caused only the heart rate and the systolic blood pressure to rise, while the diastolic pressure actually fell slightly, and isoproterenol acted only on one class of receptors and caused minimal change in the systolic pressure and a fall in the diastolic pressure while increasing the heart rate. At the close of the exercise, we opened the animal’s chest to get our first chance to do open cardiac massage. It seemed to me and many classmates that we easily could have just seen this on film rather than practicing this less than satisfying brand of medicine on our canine friends.
Back to the operating room. So now I’m looking at a human being with a wide-open chest cavity exposing a heart that is sitting like a lump of cold fat surrounded by ice, while the blood is being directed outside the body into this large box of a machine. And I’m thinking, “Isn’t this person dead? Is this a real-life demonstration of the mind-body problem? Assuming that all goes well when we restart his heart and warm him up, how do we know he’s really the same person when he comes back and not some other person who just has his memories? Why did I sign up for this?"
One reason I signed up was because coronary artery bypass surgery offers medical students extensive practice in stitching large wounds. The vein used for the bypass grafts, which allow blood traveling into a blocked coronary artery to bypass the blockage, much like a roadway detour redirects traffic, is the greater saphenous vein of the lower leg. After the surgeon removes the vein, he leaves a wound extending the length of the lower leg, which needs to be sewn together. Many a medical student learns to do an intracuticular closing stitch by sewing these wounds shut, and it provides that all-too-rare opportunity for a student in surgery to feel less like an undescended testicle and more like someone who has something to contribute.
Not that I really felt useful. One morning we were finishing replacing an elderly gentleman’s defective aortic valve when both surgeons became frantic. When they had reconnected the patient’s circulation, his aorta had revealed an unexpected fragility and had begun to disintegrate (“like tissue paper!”) under the pressure of his restored Wood flow. They hooked him back up to the pump, but because there is a limit to how long one can remain on the pump before serious physiologic consequences occur, this was a tough spot. They had about an hour to fix the aorta, which meant stitching an artificial graft to replace the areas that were falling apart. Given that there wasn’t certainty that any part of his aorta would be strong enough to hold the graft, everyone suspended the usual light banter that helped ease the tension of long surgeries. The surgeons’ orders and comments cut like knives into the still operating room air, and at times I felt as though I were forgetting to breathe. The graft held. We all welcomed the barbecue-like smell of smoke from the bovey, which cooks the open blood vessels below the skin and thereby stops them from bleeding, as this smell immediately precedes the closing of the skin, ending every operation.
So what happens to this cold, previously lifeless man once the surgery ends? We gradually warm him up, using blankets, intravenous fluids, and his own metabolism. The body responds to cold by constricting the arteries and veins close to the skin, preventing heat from escaping; this is why your feet and hands turn pale when they are cold. As the body warms up, the constricted vessels begin to dilate. Bypass patients demonstrate this dramatically. As the body warms to 95 or 96 degrees, the intravascular space suddenly becomes much larger, causing the blood pressure to fell, and we respond by rapidly infusing intravenous fluid to “fill the tank,” to maintain blood flow to the vital organs. Fluid management in these patients is tricky, because if you fill them up too fast, the amount of blood the heart has to pump exceeds the heart’s capacity, particularly in patients who have weakened hearts anyway. We call this situation heart failure. It results in fluid backing up into the lungs, which impairs the ability of the lungs to extract oxygen from the air. To prevent this, the patient has a Swan-Ganz catheter placed in the jugular vein and threaded through the right side of the heart to the pulmonary artery, where the volume of fluid in the body can be measured with the most precision. This is just one of many tubes used to manage these patients during and immediately after surgery, the others include an arterial catheter to measure the blood pressure precisely, a Foley catheter to measure urine output, a nasogastric tube to prevent aspiration of the stomach contents, and an endotracheal tube to which the ventilator attaches.
This setup was intimidating at first, but as with many situations encountered in learning this trade, you get used to it and more comfortable with it as you begin to understand and manage the equipment and the patient to whom it is attached. If the blood pressure is too high, you increase the infusion of sodium nitro-prusside, a medicine that dilates arteries and therefore decreases the blood pressure against which the heart has to pump, reducing the work of the heart. But this medicine is metabolized into a form of cyanide, so you have to monitor the total dosage carefully. If the pulmonary “wedge” pressure, measured from the Swan-Ganz catheter, is too low, you turn up the intravenous fluid infusion. For other situations, there are other adjustments. It feds much like driving a car, knowing when to use the gas, the brake, the air conditioner, etc. If all goes well, the patient gradually starts losing tubes and lines and begins to walk, talk, eat, and use the bathroom. Other than a scar, patients who haven’t had a major complication seem the same as before surgery. As a family doctor in training, I had always looked at people as a whole, rather than as a collection of organ systems, but my experience on cardiothoracic surgery gave me insight into why many specialists see people as an assembly of parts.
BILOXI BLUES
Humiliation was a way of life for third-year students, and my worst taste of it came during my clerkship in internal medicine. Our predecessors in the class ahead had informed those of us planning to do residencies in family practice or internal medicine that we had to have strong reviews from our attending physicians and medical residents during this rotation if we didn’t wish to spend our three years of residency in Harlem, Detroit, or other less desirable locales. Excellent performance required a thorough approach. Any patient assigned to a “stud” underwent the most thorough and detailed interview (history) and examination (physical) he or she had ever endured. Fortunately, we spent half our internal medicine clerkship at the VA Hospital; veterans as a rule were lonely people who were usually pleased with the one-on-one attention medical students provided. But some of our patients just wanted to be left alone.
One evening our team was on duty for the night (this occurred every fourth night) when Keith, my supervising resident, notified me that I would be admitting Mr. C., who was about 70 years old. He was coming in with respiratory insufficiency, meaning that his lungs were not providing his organs with enough oxygen. Because most veterans smoke, many of them run into this problem late in their lives, generally due to chronic obstructive pulmonary disease and/or heart failure.
When I arrived in Mr. C’s room, he had already been started on medications and oxygen to correct his problem, and he was comfortable. A diminutive, wiry fellow (decades of working to breathe sufficient quantities of air into smoke-ravaged lungs makes one very thin), he greeted me and initially seemed content to answer my stream of questions. I learned that he spent much of his time
in Biloxi, Mississippi, whence he had just driven to La Jolla, neglecting to bring his heart and lung medications. After about 30 minutes I sensed he was growing weary of my interrogation, so I began examining him. It didn’t take tong for him to lose his temper, and I eventually fled beneath his roaring “Get the HELL OUT OF HERE, YOU GODDAMN MEDICAL STUDENT WITH YOUR GODDAMN QUESTIONS....”
Nurses, patients, interns, and residents cast inquisitive and not ostensibly sympathetic glances in my direction as they identified the trigger of this outburst. I sought the shelter of a little room with bunk beds, where we spent our nights in the
hospital, to write up my findings, knowing that his reaction and the incompleteness of my work would be held against me.
During morning rounds, the team always visited patients at their bedsides, so the following morning Keith approached Mr. C., greeted him, and informed him that the rest of the team would be coming into the room. Mr. C. responded, “That’s fine. Everyone’s welcome...except that GODDAMN MEDICAL STUDENT WITH HIS GODDAMN questions. Get him the HELLOUTTA HERE!” I Stayed out.
After the team finished talking to Mr.C., Keith approached me and jocularly inquired, “What did you do to him?” I gave a puzzled shrug and explained that he had just suddenly exploded, at which point Keith took on a more serious tone and said, “Well, we rarely have to do this, but I’m going to have to take you off this case." One of the family practice interns and the other student working on our team offered me some support, but I felt abandoned, alone, and uncertain of my future in medicine that night.
A couple of weeks earlier a patient under my care had died. He was my first patient to die, but his death unnerved me for other reasons. A stocky, “tough-as-nails,” 59-year-old guy came in with pneumonia, and Keith assigned him to me.
Another smoker with significant lung damage, this muscular gentleman still led a vigorous life and looked as though he had another 20 good years left. However, his blood oxygen levels were dropping before my eyes, and it became clear to my inexperienced medical mind that he was likely to need more than just some oxygen blown into his face and intravenous antibiotics to get better; he looked as though he would be needing a ventilator. I talked to him about this, and he made himself perfectly clear: he didn’t want anything to do with endotracheal tubes or breathing machines. My explanation that he might need these to survive until the medicines started working did not change his mind. To him, mechanical ventilation meant a complete invasion of his personal space and loss of dignity. I’m not sure he ever understood that his need for mechanical ventilation would probably be temporary or that his stubbornness could be fatal to him and devastating to his wife. My shift was ending as I left his room, and I will never forget his wife asking me, “He’ll be all right, won’t he?” I responded honestly, with my throat in a knot, “I don’t know. He might not be.”
Somehow, when I went home that evening, I assumed he would be fine. The next morning’s news that he had been found dead in his room the night before was a rude awakening to the realities of practicing medicine. People, sane people, make “informed” decisions about their medical management that we who know and live with the consequences have to obey. There was more to it than that, though. That guy should not have died, and my team, particularly Keith and our attending physician, should have been more active in the care of a potentially critically ill patient. Knowing what I know now, I am sure I could have prevented his death by mobilizing his family and friends; his wife did not have the necessary influence to change his mind. Guilt overwhelmed me that morning; I felt that something could have been done to save him, and I was probably right. The VA Hospital conducted a quality-assurance investigation of the circumstances of his death. I do not know the outcome It was the only time during my medical school training that I observed negligence resulting in a tragic consequence. I learned then to trust my gut and to be willing to raise a fuss if I thought a superior wasn’t doing enough for my patient.
PSYCH
My next stop was a six-week stay on the locked psychiatric ward at UCSD’s University Hospital. The intimate confines, small number of patients, and close one-on-one working relationships with senior residents contrasted with the fast pace and often impersonal nature of the working relationships on my previous clerkship. At that time the ward had just 15 patients, split equally among three second-year residents. Each resident had a private office and one medical student who shared the office and patients. The patients were acutely ill, warranting hospitalization because they were dangerous to themselves and/or others. The hallways formed a U-shape, with locked exits at both ends. There were two padded isolation rooms, into which staff placed patients who, despite medication and close supervision, could not interact safely with the others. Patient rooms lined the arms of the U, and patients were allowed free access to hallways and activity rooms along the base of the U, across from the nursing station.
Once I got used to being enclosed in close quarters with some of the sickest psychiatric patients in San Diego County, I grew to like the place. One could never be certain what human drama would be played out on a given day, and I, unlike my classmates who did psychiatry clerkships at the VA, where they dealt almost exclusively with chronically ill patients, never got bored. The dramas were not restricted to patients; one of the residents broke down and cried on several occasions during the six weeks, although I never found out why. Barry and Doug, the two students with whom I spent this clerkship, were cool customers in every respect and provided levity and humor, which were otherwise scarce. Barry had played football at Stanford; Doug, a Japanese American, had come from UC Berkeley and had paired with another Japanese American member of the class to form “The Rapping Japs,” a duo whose one and only appearance brought down the house at the traditional performance of skits at the end of our first year.
There are those who claim that the mentally ill are the only people who truly know what is going on, and some of what I saw and heard on the locked ward supported this. We encouraged patients to draw or write as a means of expressing themselves, often with stunning results. I remember one paranoid schizophrenic’s vivid drawing of a deranged satanic figure, his face laced with bright yellows and purples forming a frightful, screaming expression as an arrow pierced the middle of his forehead, yielding a free flow of bright red blood draining his life from within. Another drew a large, distorted flower of soft, wide purple and yellow petals almost as beautiful as it was peculiar. A young black woman, also a paranoid schizophrenic, produced a stream-of-consciousness narrative in which she strung the following thoughts together: “Can that Coke! Fast food. We all must die together.” She could have given dietary counseling to the patients in the coronary care unit.
Then there was a former member of the Vietcong who had recently developed some peculiar habits and no longer spoke intelligibly, in English or Vietnamese. Sporting an inappropriate half-grimace, half smile on his reddened, weatherbeaten round face, he showed us one of the least appealing of his new behaviors, that of playing with his feces immediately after making a fresh deposit in the toilet. He would kneel like a child in front of the bowl and swirl the feces with his index finger. Once in a while he would point to his abdomen and yell, so we had an internist see him in consultation. He and Bob, his medical student, ended up cracking the case by sending a sample of the patient’s stool to the lab. In that specimen, the lab found Strongyloides, a parasite that affects the GI tract, the lung, and the brain. While playing with his feces, this “crazy” fellow, ironically, was showing us where to find the answer to his troubles. My six-week clerkship ended at that point, but I learned afterward that once they treated his parasite, he transformed into a much more personable fellow, and his peculiarities vanished.
My psychiatry rotation arrived at the onset of spring, and I had the good fortune of teaming with the star among the three residents. Patti was the best, and she knew it. Bright and confident, with thick shoulder-length dark brown hair and freckles that brought a childlike petulance to her Irish face, Patti dressed in fashionable, flattering short skirts and had a way of swinging her legs up under her onto her office chair that made one’s heart skip a beat. Yes, I had a crush on her, the only time that happened during my medical education. I'm quite sure she never knew it, but there was an undeniable intensity in our interactions that I cannot attribute solely to the intimacy of our surroundings. She talked often about the golf pro she began dating during my clerkship, and I dutifully feigned interest. Though I was unattached, I thought it far too risky to pursue her, as her evaluation could affect my career, and I had promised myself I would never date a doctor anyway.
Because she was the best, her patients recovered the fastest, which meant we had to take on more new patients than the other two teams. We worked harder, so I learned more. By the time we were halfway into the rotation, I was involved in the treatment of all five patients assigned to us. Therefore, I frequently presented patients at clinical rounds with the attending and the chief resident. That’s the sort of activity that chief residents and attendings notice. I never went out of my way to impress superiors on my rotations because I found that trait nauseating in peers, most of whom didn’t do it either. On this rotation, however, I wanted to impress Patti, so when she gave me work, I did it with zeal, and I got a lot of credit.
Bob, the student who helped bring our Vietcong patient back from fecal-soiled delirium, exemplified the brown-nosing extreme. One of the least-liked members of our class, he earned his lack of popularity with his nasal voice, impertinent wisecracks, and insincerity. During our obstetrics and gynecology clerkship, Dr. Ornstein scheduled individual teaching sessions with students. A nurse practitioner prepared us for this tutorial by telling us that Dr. Ornstein always asked the question, “What is a Pap smear?" and he expected the student to answer, “It’s a screening test for cervical cancer.” During his session, Bob gave the answer, and when the doctor remarked, “I see you were appropriately prompted,” Bob replied, “No, I just read a lot.” One of our sickest patients on the psych ward, EC., a stout, 50ish, strawberry blond woman with a disheveled appearance and histrionic demeanor, was battling severe depression that resisted many of our therapeutic interventions, including counseling in various settings and medications. She also had a significant medical problem: atrial fibrillation (A-fib).
Former President Bush had A-fib. It’s a condition where the right atrium of the heart, the chamber that houses the natural pacemaker, has been damaged such that the pacemaker no longer generates a timed electrical impuLse to cause a rhythmic heartbeat. Instead, the chamber randomly flutters, or “fibrillates,” in a chaos of disorganized electrical activity, generating a barrage of electrical impulses that are intermittently and irregularly conducted to the rest of the heart. If the rest of the heart is reasonably healthy, this activity will cause it to beat very rapidly, about 120 to 160 beats per minute, a rate that greatly taxes the heart muscle and that compromises the heart’s efficiency. Doctors usually attempt to restore the heart to its normal sinus rhythm, first with medications, then with electricity. If these treatments fail, then we use other medications to control the heart.
During the course of her stay with us, I noticed that E.G’s pulse rate had risen consistently above 100, which was not safe for her in the long run. Her medication, digoxin, was not adequately controlling her rate. Because I had just finished my internal medicine clerkship and was also brimming with testosterone-driven enthusiasm, I gave Patti a detailed explanation of the problem and suggested a medical consultation, which she then requested. The internist did his evaluation, we discussed it, and then started her on verapamil, which brought her rate nicely under control. Much to my chagrin, Patti did not share my joy at this result and instead her Irish temper flared. She reproached me, saying I had used my recently acquired medical knowledge to show her up. Stunned, I tried to save the situation by professing my genuine admiration for her skills and the obvious superiority of her knowledge to mine, but I failed to convince her and over the final two weeks she distanced herself from me. At the end, she gave me a lukewarm endorsement while informing me that the chief resident and attending had, to her surprise, decided to give me an honors grade. I never saw her again.
NEW LIFE
The last clerkship of my third year, my six-week obstetrics and gynecology rotation, was, despite some very long hours, one of my favorites. I returned to the Balboa Naval Hospital, this time to a brand-new facility, and everyone was in a better mood, including me. Armed with what I had learned during the previous ten months, I reduced the rest of our team’s work, and they liked that. So they occasionally rewarded me. One day in the operating room we were doing a cesarean section, with a second-year gynecology resident as the primary surgeon and a veteran attending physician, Dr. Torp, assisting him. I held the retractors. As surgeries go, C-sections are pretty easy to do, so after we delivered the baby. Dr. Torp said to the resident, “Pretty soon, you’re going to be assisting residents who have almost no experience, so let’s practice. Jim, move over. You’ll finish the case.”
And I did. We pulled the uterus outside the pelvis and laid it on the abdomen, which most surgeons do when closing the uterus because it’s easier to sew it in this position. They showed me where to put each stitch through the soft, smooth muscle of the womb and I obeyed, following the curve of the needle (the favorite instruction of everyone who teaches surgery) with each stitch, and tying the square surgical knots at the end of each layer. For once, I was not the one to cut the threads after someone else tied the knots. It is customary for the attending physician to say one of two things to the student who cuts the suture “That’s too short” or “That’s too long.” So occasionally a student arrives with enough gumption to ask before he or she cuts the threads, “So how would you like these cut, doctor too long or too short?”
I then stitched the bladder flap over the uterus, and then the peritoneum to close the abdominal cavity. These layers (surgeons always work in and talk about layers) feel somewhat like silk, except they are smooth and moist. Next came the fascial layer, the thick layer just under the skin containing mostly yellow and white fat and having a texture just softer than tender meat. Last, we closed the skin with staples. Staples, if properly placed, allow the skin to heal as well as sutures do, and they can be put in faster, which is why they have become popular. Skin is much tougher than the tissue beneath it; I bent and ruined many a needle while learning to sew skin.
Dr. Torp did wonders for my confidence that day, and I understand she has done the same for many other students. The best teachers pick their spots; they take advantage of situations where students can do meaningful work with minimal risk to patients. More commonly, as I mentioned before, students feel very small in the operating room. It was during this clerkship that I learned of a student who a few years earlier had tried to adjust the lights over the surgeons’ heads, but he banged them together so hard they shattered. The surgeons spent hours (10 to 16, depending on who was telling the story) pulling glass out of the patient’s abdomen. I don’t think I could have finished school after an event like that.
People often ask what it was like to deliver a baby the first time, and I always confess with some embarrassment that I barely remember it, which is odd since I consider obstetrics the most important aspect of my current practice. Like most students, I wanted to deliver as many babies as I could. The timing was favorable; the academic year was ending, and the interns had done enough deliveries to be willing to let the students do a few. My first came at 3:00 a.m., when a woman whose labor I had followed and documented in her chart every two hours summoned the last reserves of her energy and pushed her baby's black-haired crown through her entroitus and out into the gloved left hand of my supervising male intern.
Delivering the head requires the most skill, as the head’s large diameter causes more damage to the woman’s body during birth than any other body part. Students generally do not get to deliver the head. “Go ahead,” the intern instructed me after he used the blue bulb syringe to suck mucus out of the baby’s mouth and nose. I gratefully and clumsily accepted the invitation to finish the job, nearly tripping over the intern’s stool as I moved in to place my hands in position, one hand above the baby’s head and the other below, to perform the maneuvers I had rehearsed many times.
With my top hand I pushed the slippery head straight down toward the floor, noting the presence of a couple of other arms extended to help should I commit the ultimate crime and drop the baby. The baby’s left shoulder, partially obscured by its mother’s blood, slid out from under the top of her pelvis, prompting the intern to blurt out, “Up!” I moved the head straight up, allowing the right shoulder to emerge from the bottom of the vagina. The other hands helped me pull out the buttocks and legs.
I wish I could say that at this point I reveled in the joy of having brought a fresh new life into the world, but a new baby really is slippery, and I was scared she would fall to the floor, perhaps ending my career. I don’t remember what she looked like, who clamped and cut the cord, or what happened after that. One thing impressed me: the sturdy umbilical cord, with its rubbery, tough, gray-white braided ropelike appearance and the three life-sustaining umbilical blood vessels twisting their course toward the baby. Just another architectural wonder of nature, brilliantly suited to its purpose as the life support to the unborn fetus. I would deliver six more babies before the end of the clerkship, which finished my third year.
CLOSE SHAVE
I harmed a patient in my fourth year.
During the weekend that separates the third from the fourth year, medical students undergo a transformation from useless slave to valued member of whatever medical service they join. All fourth-year courses were elective when I was at UCSD, and it was therefore more fun than any other year of my training. Anesthesiology was one of the electives I chose, as 1 was told I would get many opportunities to intubate patients and start intravenous lines, both of which are useful skills in emergencies. It was during my anesthesiology elective that I accidentally shaved a patient’s tooth.
We intubate a patient to allow adequate oxygen exchange through the lungs when the patient is unable to do this himself, either because he’s under general anesthesia or because he’s critically ill. Sliding an endotracheal tube through the vocal cords into the trachea usually is not difficult, and most of the time students intubated patients who were under general anesthesia and who did not present anatomical challenges and were not ill.
One morning the anesthesiology resident and I were running through the usual routine, giving general anesthesia to an elderly man who was about to undergo a minor surgery. I used the bag and oxygen mask to blow a few extra breaths of oxygen into his lungs, as we always do just before we intubate. I then took the laryngoscope into my hand. This instrument has a cylindrical metal handle with a hard plastic blade, which can be curved or straight, that you put in the patient’s mouth and then use to push the tongue out of the way. The light on the blade allows you to see the back of the throat, the posterior pharyngeal wall. Down a bit farther is the epiglottis, the pink structure that flops back and forth to allow food to go down the esophagus and air to go down the trachea. As I slid the laryngoscope into position, I noticed that this fellow had two very large upper front teeth and that these were the only teeth in his mouth. He also had a short neck. People with short necks and chins are more difficult to intubate because the trachea is farther upward (when they lie on their backs). To see the straight white vocal cords, you lift the epiglottis upward by pushing the jaw forward with the laryngoscope; if you rock backward, the blade comes into contact with the teeth. I had to pull pretty hard to see the vocal cords, and I must have inadvertently rocked back. After I pushed the inflatable cuff of the endotracheal tube to its destination just past the vocal cords and looked down at the blade, my eyes met the two front teeth sticking out like shiny gold and white targets. The blade rested against the right tooth, and a quarter-inch-long white shaving, looking much like one would file off a hard white metal, dangled from the edge of the tooth. The attending anesthesiologist noted the look on my face, came over, surveyed the damage, angrily snatched the blade out, and blurted at me, “What are you doing?” He looked at the tooth again and said to the resident, “It looks okay, but we had better get a dental consult just to be sure.” He then turned to me in disgust and muttered, “Be careful, would you?”
My fear that I would do harm to someone had finally been realized. The damage was minor, but I felt terrible for days. We do have to be careful, with everyone, all the time. It is probably too much to ask of human beings so we have to learn to forgive ourselves, even when patients do not, although they usually do. No one at UCSD discussed the idea of forgiving oneself for mistakes; I did not learn to do it until my residency.
WHY CHARLIE?
To what extremes could our often reckless approach to education take us? Hard to say, but what our classmate Charlie did made me think about this for a long time.
I met Charlie in late 1985, when we both took an elective in clinical hypnosis. To dramatize the difference between using hypnosis constructively and using it for entertainment, many of us went out one evening with our professor to take in Dr. Dean’s show, in which he used hypnosis on members of the audience to entice them to perform various outrageous stunts. Charlie came with Bet, his 27-year-old wife of four years, whom I vaguely remember as a serious but pleasant individual; he seemed content and easygoing. She worked two jobs to support him through medical schooL For the next three years, my infrequent encounters with Charlie involved only the occasional exchange of routine pleasantries. In early December of 1988, Charlie spotted Tracy, a classmate and lifelong North County resident who now practices family medicine, in the medical school parking lot and shouted out a friendly greeting. Tracy said this struck her as somewhat odd, since they had rarely spoken to each other. Charlie rushed over, informed her that he had become a daddy, and proudly showed her pictures of the new family member. Tracy felt genuinely happy for him, as he seemed thrilled with his lot in life. Stories in the San Diego Union later described him and Bet as “the ideal couple,” going on outings together and attending neighborhood barbecues and other family-style events.
I left for a ten-week working vacation in Nairobi, Kenya, in late December 1988 to do my required research project. When I returned, a classmate informed me that on December 20 Charlie had allegedly strangled Bet with a telephone cord in the laboratory where she worked. He had taken out a $100,000 life insurance policy on her just four months earlier. He became the primary suspect during questioning about his wife’s death when he showed little emotion. Investigators also noticed a scratch on his chest that looked like a fingernail injury and something on his right little finger that suggested struggle with a cord.
Turbulence in relationships between my classmates and their spouses/significant others was not news. Several marriages ended during our four years, and many more long-term relationships broke off, as the constant duress of long study hours and sleep deprivation drove apart all but the most stable partnerships. I would not have suspected that anyone in our class would be capable of killing his or her spouse, and Charlie would not have topped my list of possible candidates.
Because this happened in the middle of our last year of school, during which time we did not get together as a class until graduation day, it’s difficult to say what effect this had on the class. Everyone I asked seemed as surprised and unsure of the tragedy’s meaning for us as I was. We graduated long before the trial, and from my recent conversations with members of our class it seems that most of us never found out what fate finally befell Charlie. He maintained his innocence at the beginning of the trial and even remained close to his deceased wife’s family until about halfway through the trial, when he changed his plea to guilty. He plea-bargained his charge to manslaughter,' resulting in a 12-year prison sentence. He was only six months away from earning his M.D. and practicing medicine.
Medical school, and residency after it, attacked us where we were most vulnerable. We confronted death, nudity, blood, and disease while our schedule and teachers denied us the sleep and self-esteem that are so important in keeping oneself grounded while surrounded by emotional chaos. Traditionally, medical teaching institutions have neglected the emotional growth and education of their students, claiming that extreme conditions of sleep deprivation and hard work build better doctors. Most of the faculty and almost all my supervising interns and residents at UCSD knew the absurdity of this philosophy and tried to help the medical students survive the clinical years without mental breakdowns. Some of our most accomplished faculty had left the intense academic atmosphere of other medical schools, particularly those on the East Coast, for the more relaxed atmosphere of UCSD. A few of them confessed to enjoying students and granted us the same courtesy and empathy they showed patients. But I hope that Bet didn’t die completely in vain and that changes in policy to improve the treatment of students ensued.
I left UCSD much the same as I had entered, except that I had less tolerance for shallow banter and small talk, making my personality seem more serious and intense. I think this happens to most of us in medical school. After completing a three-year family practice residency in Maine, I now have a four-year-old private practice in Berkeley, where I do the full range of family medicine, including obstetrics. Fifteen to 20 patients walk into my office, a converted red brick house just outside of downtown, every day with earaches, depression, acute heart attacks, sprains, memory loss, and just about anything else that can happen to a human being. Most speak English or Spanish, but many come from places like the Far East, the Philippines, and Africa. Once in a while I get to use the French I learned while working in Belgium for two months the year before I started at UCSD.
In an attempt to distance myself from the hierarchical structure of medical school, I have left my white coat at home since the day my residency started; this fall, I sent it to the Goodwill. I teach physician’s assistant and nurse practitioner students in my office twice a week and try to make them feel comfortable and competent, because I remember.
Comments