 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
Some weeks in family practice have themes. This week's theme was colon cancer.
Monday morning I went up to the sixth floor of the hospital to check on Viola. Now 86 years old, Viola is one of many delightful old African-Americans who grew up in the South, moved to Berkeley, and now entertain me and my staff with their youthful smiles and never-failing spirits. Widowed 5 years ago after 60 years of marriage, she is also one of several octogenarians I’ve known who have outlived their husbands and could not see any reason to go on living. I had to get past her cheerful countenance to discover this. She was bent over, looking at her knees, as I entered her room. “I recognize those feet,” she greeted me without looking up.
Two abdominal surgeries and three major complications hadn’t silenced her humor.
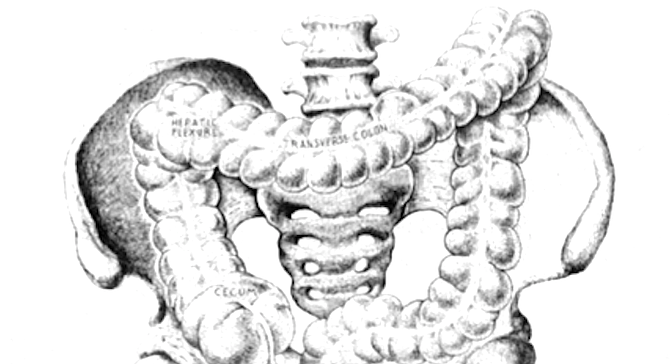
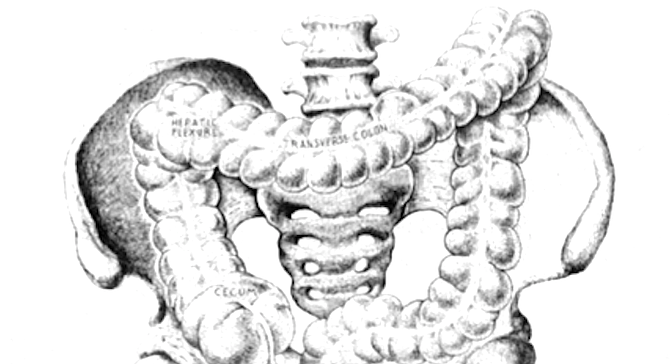
One month ago, Viola had come to my office for her routine blood pressure check and mentioned some increased fatigue. I sent her to the lab across the street for a blood count, which showed that she had iron deficiency anemia. Women after menopause get iron deficient when they are losing blood from an unknown source, usually the gastrointestinal tract. I therefore referred her to a gastroenterologist, who found a small cancer in her “hepatic flexure,” where the ascending colon turns 90 degrees in the right upper abdomen to become the transverse colon. On Saturday morning two days later, I assisted Charles, the general surgeon, as he performed a right hemicolectomy, the removal of the right colon. As with most of our organs, we have more colon than we need, so our guts function normally after a right hemicolectomy.
She had her first complication the next morning, when she bled so much from her rectum that we had to give her a four-unit blood transfusion. I had signed out the day before to take the weekend off, so Charles had someone else assist him when he went back into her abdomen to find that her colon was bleeding where he had reconnected the ends, a problem he had never seen in his 30 years as a surgeon. He took apart the ends, stopped the bleeding, sewed them back together, and closed her up again.
I didn’t find out any of this had happened until the following evening, when the surgeon called me about her second complication: her heart rate was suddenly 140. Blood loss and two surgeries had so stressed her heart that it had converted from its normal “sinus” rhythm to “atrial flutter,” a common rhythm in the elderly that can lead to heart failure, which results when the heart is not able to pump enough blood to the rest of the body. I went straight to the hospital and ordered an intravenous medication, diltiazem, that returned her to sinus rhythm.
A week later, she went home, where she met her third problem. Handling the intestines during surgery causes them to shut down for a while, so when the pyloric sphincter at the stomach’s exit release, a recently ingested meal into the small intestine, the food just sits there. After surgery, we wait until we can hear through our stethoscopes the distinctive gurgling of functioning bowels before we allow patients to start taking in clear liquids and gradually advance to a regular diet. Viola’s two surgeries, blood loss, and heart troubles denied her guts the oxygen and nutrition they needed to recover, so over the next several days, she lost her appetite. On Saturday, she vomited several times, so we had to bring her back into the hospital.
Now, two days later, her nausea had resolved, thanks to the nasogastric tube that was sucking out through her nose the bile and stomach secretions that for days had been stuck in her stomach and small bowel. That evening her bowels would awaken with a roar, keeping her glued to the commode for most of the night with diarrhea. But for now she was comfortable, sitting on the edge of the bed ready to chat with me.
“How’s your wife?” she demanded. “Are you getting ready, if you know what I mean?" I knew, she had been telling me to have children for more than two years. “Tell her the old lady hasn’t got much time left.” A mischievous grin spread across her chubby face, and we both knew she was on her way back.
That afternoon, Virginia came to see me in my office. A 75-year-old retired librarian with hypothyroidism and chronic mild depression, she maintains a proud countenance that offsets her melancholy air. Her white, wrinkled skin has paled from a ten-month course of chemotherapy, but she has kept the elegance in her stride and eloquence in her speech.
It had been almost a year since I had discovered occult blood in her stool during her annual physical examination. This is why I check the rectum of every patient in my practice over age 50 every year. During my second year of medical school at UC San Diego ten years ago, Bill, a fourth-year medical student, taught me and three colleagues how to finish the rectal examination. “Take your finger out of the rectum. There will be a lump of shit on it. Rub the shit onto the two squares of this Hemoccult card, turn it over, open the back, and put a couple of drops of developer on it. If the stool turns blue, there's blood in it.”
Blood in the stool can be benign. Internal hemorrhoids are common, particularly in Western cultures where our diets often cause constipation. Polyps, which are stalks of tissue that extend into the lumen (tube) of the colon, can ooze small amounts of blood. These can become cancers, and therefore if a gastroenterologist encounters polyps when examining the colon through a sigmoidoscope or colonoscope, he or she will remove them unless they are too large to do so safely.
Arteriovenous malformations (AVMs), another source of blood in the colon, are developmental errors. Normally the arteries supplying blood to an area divide into smaller vessels, called arterioles, which feed tiny capillaries that bring nutrients to cells. Tiny venules drain these capillaries into larger veins that take the blood back to the central circulation. An AVM occurs when an arteriole connects directly to a vein, dumping much more volume and pressure into the vein than nature intended, creating an engorged vessel susceptible to leaking or even breaking. By using a laser to burn them or by injecting ethyl alcohol to cause them to shrivel, a gastroenterologist can fix AVMs through the colonoscope.
Virginia had a three-centimeter cecal cancer. A bulb-shaped structure adjacent to the appendix, the cecum terminates the small intestine, after which the ascending colon begins. The small intestine completes the task of breaking down and digesting the fats, sugars, and proteins we eat, so when our meals reach the cecum, all that is left for the colon to do is absorb salt and water, changing the bowel contents from a greenish yellow slime into a solid brown lump.
Charles and I took out her cecum and right colon two weeks later. Unlike Viola, Virginia breezed through her postoperative course (what we call the recovery period from surgery) before starting one year of chemotherapy, which in recent clinical trials has decreased post-surgical metastases in patients with colon cancer.
Most chemotherapy drugs are poisons that kill the most rapidly dividing cells in the body. Cancer cells divide quickly, but so do many normal cells, such as hair and blood cells, which is why chemotherapy causes hair loss, anemia, and immune-system depression. The goal is to eliminate as many cancer cells as possible without destroying enough normal cells to kill the patient.
We had scheduled this afternoon’s visit to check her hypothyroidism, a common condition in which the thyroid gland, located in the front of the neck just above the collarbone, fails to produce enough thyroid hormone. “As long as I can tend to my garden, I'll make it,” she convinced me. For about one week out of every month, she has the usual nausea and fatigue from her chemotherapy, but she still has a full head of hair, and if she can avoid what is happening to Louise, it will be worth the trouble.
Louise is an 88-year-old African-American from Chicago, now two years removed from a left hemicolectomy for a cancer I found with one of those Hemoccult cards. looking 20 years younger than her age, she came to my office Tuesday morning. Carroll, her 84-year-old boyfriend who has also cheated time, escorted her in, as always.
“I’ve had this pain in my right side for three days,” she explained, pointing to her right lower rib cage, underneath which the liver resides. She otherwise felt fine except for a poor appetite, but she had not lost any weight.
As a physician, I’m supposed to care for all of my patients equally, but I have biases like everyone else. Since 99-year-old Rudy and his 88-year-old wife Fern both died this past year, Louise and Carroll are now my favorite old couple. So while her symptoms were telling me that her cancer had spread to her liver, I didn’t want to hear that, so my initial reaction was the same as any close friend’s would have been: denial. After examining her and not finding anything significant, I told her she might have strained the intercostal muscles in her lower rib cage, which was not likely since she was not tender there and deep breaths did not worsen the pain. I did say we had to make sure it was not cancer, so I ordered some blood tests. It was not until after she left the office that I recognized that those test results were probably not going to come back normal.
They did not. Her dying liver cells were releasing enzymes into her blood, so her liver enzyme levels were elevated. I called her gastroenterologist. “She has mets [metastatic cancer]” was his subdued reply. “What a shame.” Because we did not know the benefits two years ago, she had not undergone preventative chemotherapy, and we'll never know if this might have helped.
ACT scan of Louise's abdomen four days later showed that the cancer had invaded most of the right lobe of the liver, the left lobe had been spared, at least for now. The cancer had not yet obstructed her bile ducts, through which the liver sends bile to the first part of the small intestine, the duodenum, to digest the fat we eat. Obstruction of the ducts causes severe pain, nausea, and jaundice.
Louise and Carroll came lack two days later to discuss what lay ahead. “I guess I’m going to join Herb Caen,” she said with her usual graceful smile, referring to the San Francisco columnist whose lung cancer had taken his life the previous week. We do not have any treatment options for her other than doing our best to keep her comfortable.
Wednesday, the day after Louise’s visit for her rib cage pain, Fannie came in to see me. Originally from Texas, Fannie and her sister Ella Mae are 78 and 80 years old, respectively, and two of the sweetest souls in my practice. Ella Mae has severe chronic lung disease and never complains. Her “little sister” has high blood pressure, but this is under good control, and she is otherwise in excellent health. She sees me every three months and always has a number of minor concerns. Her visit on this day was for a routine blood pressure check, but she mentioned that she had been tired lately. Several of her close friends had died recently, and she had stopped making her Sunday trips to church, which she used to enjoy. I made the usual inquiries about other symptoms, sleeping habits, diet, and stress and then examined her without finding anything significant.
I told her that the fatigue was likely secondary to depression, a common cause, and we talked about what she could do to help that. She agreed to resume her weekly trips to church to improve her social life. Because anemia and hypothyroidism are common and cause fatigue, I ordered a complete blood count (CBC) and a thyroid function test.
The next day her CBC came back and showed moderate iron deficiency anemia. I had checked her stool for occult blood during her annual physical exam three months earlier, and she had done three more Hemoccults at home, all of which were negative. The Hemoccult is not, unfortunately, a sensitive test for blood loss in the GI tract, which is why we have to look there with a scope in patients with unexplained iron deficiency.
Fannie escaped the diagnosis of the week. She has a colon full of A VMS, which we can manage by giving her iron supplements. We’re both feeling better now.

Some weeks in family practice have themes. This week's theme was colon cancer.
Monday morning I went up to the sixth floor of the hospital to check on Viola. Now 86 years old, Viola is one of many delightful old African-Americans who grew up in the South, moved to Berkeley, and now entertain me and my staff with their youthful smiles and never-failing spirits. Widowed 5 years ago after 60 years of marriage, she is also one of several octogenarians I’ve known who have outlived their husbands and could not see any reason to go on living. I had to get past her cheerful countenance to discover this. She was bent over, looking at her knees, as I entered her room. “I recognize those feet,” she greeted me without looking up.
Two abdominal surgeries and three major complications hadn’t silenced her humor.
One month ago, Viola had come to my office for her routine blood pressure check and mentioned some increased fatigue. I sent her to the lab across the street for a blood count, which showed that she had iron deficiency anemia. Women after menopause get iron deficient when they are losing blood from an unknown source, usually the gastrointestinal tract. I therefore referred her to a gastroenterologist, who found a small cancer in her “hepatic flexure,” where the ascending colon turns 90 degrees in the right upper abdomen to become the transverse colon. On Saturday morning two days later, I assisted Charles, the general surgeon, as he performed a right hemicolectomy, the removal of the right colon. As with most of our organs, we have more colon than we need, so our guts function normally after a right hemicolectomy.
She had her first complication the next morning, when she bled so much from her rectum that we had to give her a four-unit blood transfusion. I had signed out the day before to take the weekend off, so Charles had someone else assist him when he went back into her abdomen to find that her colon was bleeding where he had reconnected the ends, a problem he had never seen in his 30 years as a surgeon. He took apart the ends, stopped the bleeding, sewed them back together, and closed her up again.
I didn’t find out any of this had happened until the following evening, when the surgeon called me about her second complication: her heart rate was suddenly 140. Blood loss and two surgeries had so stressed her heart that it had converted from its normal “sinus” rhythm to “atrial flutter,” a common rhythm in the elderly that can lead to heart failure, which results when the heart is not able to pump enough blood to the rest of the body. I went straight to the hospital and ordered an intravenous medication, diltiazem, that returned her to sinus rhythm.
A week later, she went home, where she met her third problem. Handling the intestines during surgery causes them to shut down for a while, so when the pyloric sphincter at the stomach’s exit release, a recently ingested meal into the small intestine, the food just sits there. After surgery, we wait until we can hear through our stethoscopes the distinctive gurgling of functioning bowels before we allow patients to start taking in clear liquids and gradually advance to a regular diet. Viola’s two surgeries, blood loss, and heart troubles denied her guts the oxygen and nutrition they needed to recover, so over the next several days, she lost her appetite. On Saturday, she vomited several times, so we had to bring her back into the hospital.
Now, two days later, her nausea had resolved, thanks to the nasogastric tube that was sucking out through her nose the bile and stomach secretions that for days had been stuck in her stomach and small bowel. That evening her bowels would awaken with a roar, keeping her glued to the commode for most of the night with diarrhea. But for now she was comfortable, sitting on the edge of the bed ready to chat with me.
“How’s your wife?” she demanded. “Are you getting ready, if you know what I mean?" I knew, she had been telling me to have children for more than two years. “Tell her the old lady hasn’t got much time left.” A mischievous grin spread across her chubby face, and we both knew she was on her way back.
That afternoon, Virginia came to see me in my office. A 75-year-old retired librarian with hypothyroidism and chronic mild depression, she maintains a proud countenance that offsets her melancholy air. Her white, wrinkled skin has paled from a ten-month course of chemotherapy, but she has kept the elegance in her stride and eloquence in her speech.
It had been almost a year since I had discovered occult blood in her stool during her annual physical examination. This is why I check the rectum of every patient in my practice over age 50 every year. During my second year of medical school at UC San Diego ten years ago, Bill, a fourth-year medical student, taught me and three colleagues how to finish the rectal examination. “Take your finger out of the rectum. There will be a lump of shit on it. Rub the shit onto the two squares of this Hemoccult card, turn it over, open the back, and put a couple of drops of developer on it. If the stool turns blue, there's blood in it.”
Blood in the stool can be benign. Internal hemorrhoids are common, particularly in Western cultures where our diets often cause constipation. Polyps, which are stalks of tissue that extend into the lumen (tube) of the colon, can ooze small amounts of blood. These can become cancers, and therefore if a gastroenterologist encounters polyps when examining the colon through a sigmoidoscope or colonoscope, he or she will remove them unless they are too large to do so safely.
Arteriovenous malformations (AVMs), another source of blood in the colon, are developmental errors. Normally the arteries supplying blood to an area divide into smaller vessels, called arterioles, which feed tiny capillaries that bring nutrients to cells. Tiny venules drain these capillaries into larger veins that take the blood back to the central circulation. An AVM occurs when an arteriole connects directly to a vein, dumping much more volume and pressure into the vein than nature intended, creating an engorged vessel susceptible to leaking or even breaking. By using a laser to burn them or by injecting ethyl alcohol to cause them to shrivel, a gastroenterologist can fix AVMs through the colonoscope.
Virginia had a three-centimeter cecal cancer. A bulb-shaped structure adjacent to the appendix, the cecum terminates the small intestine, after which the ascending colon begins. The small intestine completes the task of breaking down and digesting the fats, sugars, and proteins we eat, so when our meals reach the cecum, all that is left for the colon to do is absorb salt and water, changing the bowel contents from a greenish yellow slime into a solid brown lump.
Charles and I took out her cecum and right colon two weeks later. Unlike Viola, Virginia breezed through her postoperative course (what we call the recovery period from surgery) before starting one year of chemotherapy, which in recent clinical trials has decreased post-surgical metastases in patients with colon cancer.
Most chemotherapy drugs are poisons that kill the most rapidly dividing cells in the body. Cancer cells divide quickly, but so do many normal cells, such as hair and blood cells, which is why chemotherapy causes hair loss, anemia, and immune-system depression. The goal is to eliminate as many cancer cells as possible without destroying enough normal cells to kill the patient.
We had scheduled this afternoon’s visit to check her hypothyroidism, a common condition in which the thyroid gland, located in the front of the neck just above the collarbone, fails to produce enough thyroid hormone. “As long as I can tend to my garden, I'll make it,” she convinced me. For about one week out of every month, she has the usual nausea and fatigue from her chemotherapy, but she still has a full head of hair, and if she can avoid what is happening to Louise, it will be worth the trouble.
Louise is an 88-year-old African-American from Chicago, now two years removed from a left hemicolectomy for a cancer I found with one of those Hemoccult cards. looking 20 years younger than her age, she came to my office Tuesday morning. Carroll, her 84-year-old boyfriend who has also cheated time, escorted her in, as always.
“I’ve had this pain in my right side for three days,” she explained, pointing to her right lower rib cage, underneath which the liver resides. She otherwise felt fine except for a poor appetite, but she had not lost any weight.
As a physician, I’m supposed to care for all of my patients equally, but I have biases like everyone else. Since 99-year-old Rudy and his 88-year-old wife Fern both died this past year, Louise and Carroll are now my favorite old couple. So while her symptoms were telling me that her cancer had spread to her liver, I didn’t want to hear that, so my initial reaction was the same as any close friend’s would have been: denial. After examining her and not finding anything significant, I told her she might have strained the intercostal muscles in her lower rib cage, which was not likely since she was not tender there and deep breaths did not worsen the pain. I did say we had to make sure it was not cancer, so I ordered some blood tests. It was not until after she left the office that I recognized that those test results were probably not going to come back normal.
They did not. Her dying liver cells were releasing enzymes into her blood, so her liver enzyme levels were elevated. I called her gastroenterologist. “She has mets [metastatic cancer]” was his subdued reply. “What a shame.” Because we did not know the benefits two years ago, she had not undergone preventative chemotherapy, and we'll never know if this might have helped.
ACT scan of Louise's abdomen four days later showed that the cancer had invaded most of the right lobe of the liver, the left lobe had been spared, at least for now. The cancer had not yet obstructed her bile ducts, through which the liver sends bile to the first part of the small intestine, the duodenum, to digest the fat we eat. Obstruction of the ducts causes severe pain, nausea, and jaundice.
Louise and Carroll came lack two days later to discuss what lay ahead. “I guess I’m going to join Herb Caen,” she said with her usual graceful smile, referring to the San Francisco columnist whose lung cancer had taken his life the previous week. We do not have any treatment options for her other than doing our best to keep her comfortable.
Wednesday, the day after Louise’s visit for her rib cage pain, Fannie came in to see me. Originally from Texas, Fannie and her sister Ella Mae are 78 and 80 years old, respectively, and two of the sweetest souls in my practice. Ella Mae has severe chronic lung disease and never complains. Her “little sister” has high blood pressure, but this is under good control, and she is otherwise in excellent health. She sees me every three months and always has a number of minor concerns. Her visit on this day was for a routine blood pressure check, but she mentioned that she had been tired lately. Several of her close friends had died recently, and she had stopped making her Sunday trips to church, which she used to enjoy. I made the usual inquiries about other symptoms, sleeping habits, diet, and stress and then examined her without finding anything significant.
I told her that the fatigue was likely secondary to depression, a common cause, and we talked about what she could do to help that. She agreed to resume her weekly trips to church to improve her social life. Because anemia and hypothyroidism are common and cause fatigue, I ordered a complete blood count (CBC) and a thyroid function test.
The next day her CBC came back and showed moderate iron deficiency anemia. I had checked her stool for occult blood during her annual physical exam three months earlier, and she had done three more Hemoccults at home, all of which were negative. The Hemoccult is not, unfortunately, a sensitive test for blood loss in the GI tract, which is why we have to look there with a scope in patients with unexplained iron deficiency.
Fannie escaped the diagnosis of the week. She has a colon full of A VMS, which we can manage by giving her iron supplements. We’re both feeling better now.
Comments