 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
Recently I looked through a microscope at a small colony of the creatures that cause tuberculosis in humans. About a hundred of them had woven themselves into a long structure that — magnified 1000 times — looked like a badly fraying section of rope stained bright fuchsia. The creatures didn’t appear to be moving, and a county microbiologist assured me that right after being placed on the slide, they had been baked to death.
Amid all the dinosaur hoopla this summer, I thought a lot about those minuscule bugs. No one will ever make a horror film about Mycobacteria tuberculosis humanis. They’re too tiny, each individual less than a 6400th of an inch long. They have no personality. Yet they’ve killed more people than any sharp-toothed monsters. They’ve killed more than all of humanity’s wars — at least a billion victims in just the 19th and 20th centuries. A hundred years ago, one out of every five people in their 30s and 40s died from being eaten alive by them.
And their grisly work continues. Last year tubercle bacilli were discovered to be munching away on the lungs and other parts of 457 San Diego County residents. That means about 18 out of every 100,000 people who live here were struck by the disease, a rate that has more than doubled since 1984. Among those TB victims, some had strains of the bacillus that can’t be cured with standard drugs. “To be perfectly honest, I and most of the people who are familiar with TB are scared to death right now,” says UCSD’s Dr. Antonino Catanzaro, who just chaired a statewide Tuberculosis Elimination Task Force. “Since I’ve been a doctor, we’ve always felt relatively comfortable about TB. We had the tools we needed to handle it.” Now all of a sudden “we’ve been robbed of those tools. This multiple-drug-resistant TB has robbed us of them.... And that is what’s gotten people really scared! They think about what happened to the world 100 years ago, and they’re saying, ‘My God, is this in our future?’”
Catanzaro points out another of TB’s most frightening aspects: the fact that it can attack virtually anyone. It spreads when someone with TB-ravaged lungs coughs or sings or even talks in a voice loud enough to propel invisible drops of sputum into the air. Once these “droplet nuclei” dry out, the TB bugs act like dust particles; they can float on the air currents, fully potent, for days or even weeks. If you walk into the room where they’re floating and you happen to inhale a liter of air containing them, you can get infected. “You don’t have to be doing illicit things and you don’t have to be sick,” says Catanzaro. “You can be perfectly normal.”
Actual infection takes place when a bacillus settles onto the moist, dark surface of one of the lung’s air sacs. In this oxygen-rich environment, TB germs thrive. They grow slowly, dividing only about once per day, and they face immediate attack by the body’s immune system. But the tubercle bacilli are tough, protected by a waxy armor that withstands most of the body’s defenders. Even the macrophages (defensive cells that scout for, attack, and internalize foreign substances) rarely kill all the TB germs. They kill some and slow the growth of the remainder, but they usually wind up carrying the latter into the lymph nodes and throughout the bloodstream, seeding them in the brain, bones, and other organs. Only weeks after the infection begins do T-cells start to produce chemicals called lymphokines that help the macrophages destroy the invaders. At this point, 95 percent of those who’ve been infected with TB win at least a partial victory as their immune system kills or immobilizes the tubercle bacilli so well that the infected persons never appear sick. The only way they’re likely to know they were infected is by having a positive TB skin test or by developing active TB at some point later in life. This delayed onset of the disease happens to about five percent of all those infected; the TB germs can lie dormant for decades then begin to grow and attack anew when something weakens the body’s defenses.
For those ten percent of infected people who develop active disease (either immediately or later in life), the illness can run a course lasting from months to years, producing symptoms known all too well in the 18th and 19th centuries. Sufferers coughed, of course, and they typically ran fevers that peaked each afternoon, disappearing by the following morning. They grew thin and pale, at times feeling exhausted, at other times seized by flurries of activity marked by flushed cheeks and glittering eyes.
Such associations made their way into a broad literature that suggested that “consumption” (as TB was called then) somehow refined its victims, elevating them to a more spiritual plane. It was perceived to be “a gentle death,” according to literary critic and TB historian Mark Caldwell, who writes, “It was a badge of refinement, it was very nearly a polite accomplishment.” Among the writers, musicians, and artists afflicted by it were Modigliani, Paganini, Chopin, Emerson, Thoreau, Poe, Keats, Shelley, Trollope, Chekhov, and the entire Brontë family.
Many 18th- and 19th-century writers gave TB to their characters, particularly those in need of a vague and rapturous demise. But less than 30 years after the beatific deaths of Dora in David Copperfield and Eva in Uncle Tom's Cabin, pathologists began to look at what was really happening in the bodies of TB victims. Autopsies revealed gaping holes in the lungs, where the gluttonous bacilli — now numbering in the millions — as well as the body’s own defender cells literally dissolved the tissue, to be coughed up in the glutinous sputum. In some cases, blood vessels eroded — explaining the frightening instances in which sufferers also coughed up bright red blood. Fibrin, a product of coagulated blood, coated the lungs and pleura of some of the corpses. Purulent fluid filled the chest cavities.
As vivid as were these revelations, the news about TB that rocked European medical men was a 1882 announcement by the German bacteriologist Robert Koch. He had isolated a bacillus, then devised experiments with guinea pigs that proved the microorganism caused TB. Up to then, many people had no idea the disease could be transmitted. John Keats, for example, who had studied medicine in London before turning to poetry, spent months tending to his tubercular brother in tightly shuttered rooms. As the public ever so slowly became aware of TB’s infectiousness, people could begin to check its spread.
But a cure for TB proved far more elusive and was “not to be sought in drugs,” the San Diego Union informed its readers one day in May of 1883. “A long and fruitless search [for such a drug] has been in progress for hundreds of years and...none has been found and none ever will be found.” Hundreds of persons had been cured of the disease, the newspaper declared, but “pure air” was the key to improved health. “Many have been cured in an advanced stage of the disease by passing most of their time outdoors, engaged in some light employment. The consumptive must not allow a fear of the weather to keep him within doors. He must...keep out in nearly all kinds of weather.”
The notion that one’s surroundings could help one recover from TB was hardly news. In ancient Rome, sufferers sought warm, dry climates. By the 19th Century, the search for health was taking the tuberculous in a confusing number of directions. Washington Irving tried to mend his lungs in Canada and later Europe, while the poet Sydney Lanier headed for Florida. Robert Louis Stevenson journeyed from Scotland to New York to Tahiti, and Cecil Rhodes believed that the air of South Africa made him well again.
In the mid-1800s, the equation of cure with setting became more complicated as the first great TB sanatoria opened in what is now Poland and Western Germany. One therapeutic model required patients to exercise, take cold showers, and eat massive meals. Another demanded absolute bed rest. In the United States, the Adirondack Mountains enjoyed a reputation for restoring well-being, and in 1885 the first American sanatorium was opened there at Saranac Lake by Edward Livingston Trudeau (great-grandfather of the cartoonist Garry).
By 1935 some 471 full-fledged American sanatoria had come into being, with another 418 TB departments operating in connection with hospitals. The sanatoria tended to cluster in “healthful” locations, but theories about just what constituted healthfulness again varied wildly. The Adirondacks, and Saranac Lake in particular, remained a mecca, but Colorado attracted high-altitude partisans. (Today the most famous center for TB research is at the National Jewish Center for Immunology and Respiratory Medicine in Denver.) The entire Southwest lured those who thought a mild climate most beneficial, and San Diego was no exception.
As early as 1885, the same year Trudeau opened his Little Red Cottage, TB victims were making their way here, according to one oral history on file in the San Diego County Historical Society’s archives. In this document, a San Diego immigrant named Hattie Kaufman describes moving to Alpine where there was “a kind of sanitarium... with lots of tents with beds in them.... We never had less than 10 or 15 consumptive people there with tuberculosis.... There were no facilities to take care of them in San Diego. These people were sent out here from the East, and as there was so much fog in San Diego, the doctors would send them on up to Alpine, where there wasn’t any fog.”
The influx of hopeful “lungers” accelerated as San Diego entered the 20th Century. By the summer of 1920, when the county had a population of 74,000, the State Bureau of Tuberculosis dispatched a field worker named Ida M. Theile to assess conditions here. “The Indians thru the County are very susceptible,” she reported, adding that by one estimate, 75 to 80 percent of the entire Indian population was infected. “Their superstition and ignorance and unsanitary method of living make them especially good subjects.” But they were hardly alone. San Diego’s resident Mexicans “are infected to a great extent,” Theile wrote, and “La Mesa and East San Diego afford an excellent climate for the tuberculous and so are to a great extent resorts.” She noted that National City and Escondido lured their share of patients, and “the equable climate of San Diego attracts many.... Some have sufficient funds...and are no great problem, but many others come with little more money than is needed to bring them here, and in all stages of the disease, occasionally even dying on the train before it reaches the city. The rooming houses are full of them, but no precautions are taken when they die or leave. These people present a serious problem. They are not careful in their habits. The rooms are poorly renovated if at all after they leave.”
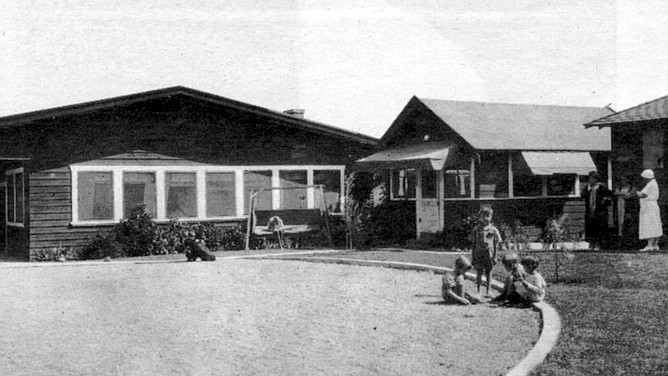
In addition to the boarding houses, two major institutions were accepting tubercular patients in 1920. The oldest was Rest Haven, established in 1913 by the San Diego Society for the Study and Prevention of Tuberculosis. Originally an open -air camp, it evolved by the late 1930s into an elaborate complex including a hospital building (still in use today as Villa View Community Hospital). During World War I, Rest Haven restricted its care to servicemen with TB, but by 1920 it had modified its mission to care for children aged 3 to 12 who were in an anemic condition or who had had contact with TB.
Eventually, Rest Haven accepted youngsters with a wide range of medical problems, but TB always numbered among the criteria for admission. One person who recalls the Rest Haven regime in the early 1940s is Stella Larson, today a resident of Imperial Beach. Around 1940, when Larson was about ten, she was living in La Jolla at the Gillispie Welfare Cottage on Girard Street. (Her mother’s death had resulted in her family’s breaking up.) Larson says when she began fainting and “started spitting up a lot,” X-rays revealed spots on her lungs. “The doctors must have talked it over and decided I wasn’t sick enough to go to [the county’s TB facility].” So they dispatched her to Rest Haven.
Located not far from what is now 54th Street and El Cajon Boulevard, Rest Haven then felt like a country retreat, according to Larson. Her first three weeks were spent in an isolation room. “I didn’t like it there, I know that!” she says today. “I didn’t like it because it was new and strange and I missed my home.” Still Larson adjusted quickly. “I could control that cough, and I didn’t cough in anybody’s face,” she says today with some pride. After her three-week quarantine, she moved into a dormitory and donned the Rest Haven uniform for girls: shorts and a bolero-style sun top tied around the back and at the neck. “We had to wear that all the time. Even in winter! Though they let us put our sweaters on and we didn’t go out as much when it was cold.”
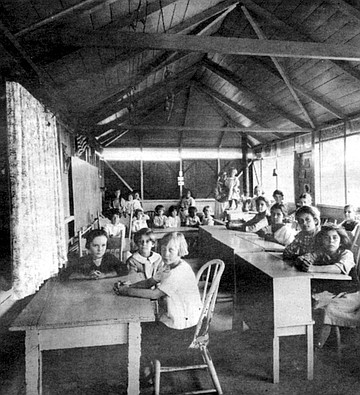
Education for Rest Haven’s inmates took place in a one-room schoolhouse that had opened in 1925. But outside of class, no special exercises were mandated. “We were just supposed to go outside and play like a normal kid does. They had a collie dog, and he used to follow us around, I remember that. Also they had a berry patch, and I enjoyed that.” Larson was eventually discharged in 1945, apparently healthy.
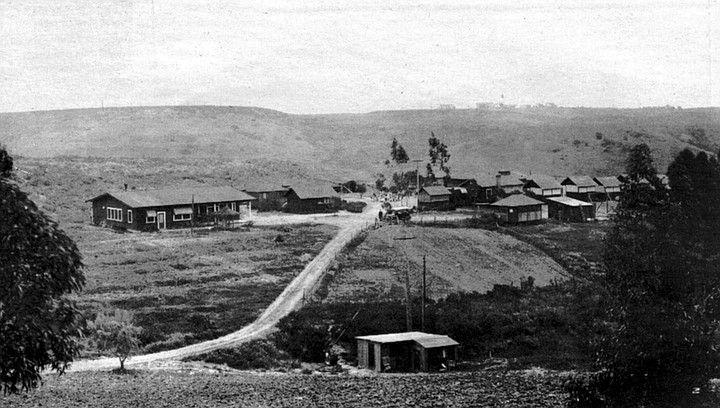
San Diego’s other major TB institution, Vauclain Home, was less bucolic. It took its name from John Vauclain, a Pennsylvanian who came to San Diego in 1887 in search of a climatic cure. No hotel or rooming house at that time would take him in because of his illness, so he bought a home on the northeast corner of Second Avenue and Cedar Street downtown; there he recovered his health and lived until 1909. In his will, he left a third of his estate to establish a TB colony, and his executors finally acquired some land in Normal Heights where they erected tent houses. That enterprise failed, and in 1918 the managers turned over the property and some cash to the county, which ordered a facility to be built on a 45-acre site overlooking Mission Valley that came to be known as Vauclain Point.
Located about a mile from the old county hospital (now UCSD Medical Center), across the canyon from it, Vauclain Home came into being in 1919, just as sanatoria were reaching their heyday. But in some regards, the San Diego facility differed from the archetype established in upstate New York and replicated throughout the country.
Mark Caldwell, whose book The Last Crusade is largely devoted to an analysis of sanatorium culture, describes the typical sanatorium as a totalitarian realm where adherence to certain notions was carried to cultish excess. By 1916 rest had “become the dominant factor in sanatorium routine, replacing exercise, which was allowed in increasing doses only as the patient edged toward normal life,” Caldwell writes. “But inactivity, crucial though it was in the sanatorium, implied passivity and helplessness. Resting outdoors, day and night, summer and winter, made rest into a challenge....”
Patients at many facilities thus were carted outside even when winter temperatures fell below freezing. “Detailed instructions were introduced about everything from the way patients were to inhale the outdoor air to the lounge equipment and bodily positions they used to ingest it,” Caldwell writes. Other daily routines were also spelled out in obsessive detail, a systematization that “was not so much a direct treatment as a giant living metaphor of order, erected in the face of the unpredictable, as a bulwark against it.”
Though the rigidity made aspects of sanatorium life nightmarish, surprisingly few patients denounced the system. Cheerful submission was demanded, and there was daily indoctrination in the salubrious effects of positive thinking. In The Plague and I, one mordantly funny exception to the typical sugar-coated memoir, writer Betty MacDonald (author, also, of The Egg and I) described how the staff of her Seattle-area sanatorium dished up daily “beautiful thoughts” along with each meal (“If you must be blue, be a BRIGHT blue!”) while at the same time prohibiting bedridden patients from reading or even talking with their roommates and forcing them to endure the cold wind and rain that streamed in their perennially open windows. In San Diego’s Vauclain Home, optimism was de rigueur. One 1939 newspaper article twinkled that “Visitors may search the children’s ward from corner to corner, and they will find neither hide nor hair of Old Man Gloom...for cheerfulness is the rule....” A published statement from Vauclain patients proclaimed that “the mental attitude of the patient is 50 percent of the cure in tuberculosis.” But Vauclain imposed no unreasonable demands on its patients, at least not according to William Weathers’s recollection.
Weathers has lived in San Diego for all but five of his 79 years. In 1940 he had just gone to work for the post office, carrying special delivery mail and earning an average of $22 per week. “I used to work my tail off. The more mail I delivered, the more money I made.” Then his back began to hurt. Weathers says at first he thought an old work-related injury was causing the pain, but it increased to the point where he remembers lying in bed at night and having to grab one side of his pajamas to turn himself over. When he also began having night sweats, he saw a doctor, who diagnosed tuberculosis of the spine. “I said, ‘How long’s it gonna take [to get well]?’ He said, ‘You’ll probably be off the job about a year.’ And I said, ‘Open a window and I’ll just jump out and get it all over with.’ ”
Things went better than Weathers anticipated. His wife, who hadn’t been working, got a job at the post office in his stead, and Vauclain Home accepted him for treatment at no charge. In the Hillcrest facility, Weathers says the doctors immediately placed him on a Bradford frame, a canvas bed stretched across a galvanized pipe framework. “It put a reverse arch in your back,” he explains. “I laid on that thing for I don’t know how long. The first week I thought I was gonna die because the curvature of my back was just the opposite of what it was originally.... It was so uncomfortable they finally rolled up a blanket and had me lay across that. I couldn’t turn or anything. If I had tried to move, I’d probably tip the thing over.”
Weathers recalls that at one point one of the X-ray technicians, who had worked in another sanatorium, told him he was lucky to be at Vauclain, that the San Diego sanatorium treated patients much better than did other TB establishments. Weathers could read (though it was difficult in his contorted position), and he could chat with other patients. “I remember I could look down the hall, just a little ways, and I used to talk to a girl in another ward there. We’d shout back and forth.” Weathers couldn’t play cards like other patients, but he listened to the radio, and at times the scene out his window entertained him. “The psychiatric hospital was right across the road from us, and about twice a week they’d take two or three people up to Patton (state mental hospital]. They didn’t have too much trouble with the men, but the girls used to fight ’em! They’d strap them in the back seat, and they were kickin’ and all. I always used to watch that.” He laughs.
“Practically every morning we’d hear about somebody passing away in the night,” Weathers recalls. But he never despaired about his own prognosis. “I just said to myself, if there’s any way to get out of here, the best way is to eat my way out. So everything they sat in front of me, I ate. When I went in there I weighed about 135 sopping wet.” One year later, weighing about 160 pounds and having undergone “spinal fusion” surgery, which he says immobilized the disintegrated vertebrae in his lower back, he was asked by one of the doctors if he’d like to go home. “I couldn’t believe it.” The memory makes his voice shaky. “I cried like a baby.”
By 1941, when Weathers was released, San Diego’s tuberculosis incidence had fallen to 70.5 cases per 100,000 residents (compared to 227.2 in 1920, the year of Nurse Theile’s report). Authorities still are debating why fewer people were catching TB then, both here and elsewhere. Was it the general rise in prosperity? Better health screening? Increased resistance bred through Darwinian-style pruning? Despite success stories like those of Stella Larson and William Weathers, the impact of the sanatorium movement remains unclear. According to historian Caldwell, “Consistently, from the beginning of the sanatorium movement through the 1940s, nearly 25 percent of all patients died while in the hospital, and 50 percent of all released patients succumbed within five years of discharge. Some institutions prided themselves on records better than this average, but these were often the ones that limited patients, as far as possible, to those with incipient tuberculosis and left the moribund to state and county hospitals.”
Unclouded victory over the tubercle bacillus came only with the drug discoveries of the 1940s and early ’50s. These began with the realization that a certain mold found naturally in soil, streptomyces, powerfully inhibited the growth of so-called “Gram-negative” bacteria, including Mycobacterium tuberculosis. (The TB germ produces an enzyme that destroys penicillin, that other famous mold byproduct.) Human experiments with the new drug, streptomycin, were generating great excitement by 1946, as was a second anti-tubercular substance discovered in Sweden, PAS (para-aminosalicylic acid). By 1952 a still more powerful antibiotic called isoniazid, or INH, appeared. Used in combination with the first drugs, it seemed at long last to give humanity truly lethal weapons against the ancient scourge.
From 51 cases per 100,000 population in 1953, San Diego’s TB incidence over the next five years plummeted: 43.7 in 1954, followed by 35.9, then 29.8, 25.2, 18.6. In 1964, with the rate at 14.3, Vauclain Home shut down; remaining TB patients moved into the county hospital. Although the incidence of tuberculosis fluctuated somewhat in the ’60s and ’70s, the basic trend continued downward through 1985, when only seven out of every 100,000 San Diegans were reported having the disease. Medical scientists envisioned TB germs being obliterated from the planet by the year 2010.
Then came the turn-around. From that low of 149 cases in 1985, the numbers jumped to 244 in 1987. Since 1988 they have climbed without interruption: 294 cases in 1989,346 in 1990,391 in 1991,458 last year. Dr. Kathleen Moser, San Diego County’s TB Control chief, calculates that San Diego has the seventh highest number of cases in the country. “An epidemic is when you see cases in excess of what you have expected, in a continuous manner. And in that sense, I believe we are in an epidemic,” Moser says.
What has happened in San Diego has been occurring all over the country — with some interesting variations. Here, 65 percent of the TB victims come from other countries (according to 1991 figures), whereas nationally the percentage of foreign-born TB cases is just 27 percent. Nearly half of all people with TB here (47 percent in 1991) are Hispanic, compared with just 20 percent nationwide. But many San Diego Hispanics have regular contact with Mexico, where the active TB rate has been estimated to run as high as 400 cases per 100,000 (compared to San Diego County’s current 18 per 100,000). Fifteen percent of San Diego’s TB cases in 1991 were either born in or descended from those born in the Philippine Islands — where the active TB rate may run as high as 1500 cases per 100,000.
The frightening situation in some foreign countries is matched by that in certain American subgroups. The rate among young black men in New York City, for instance, exceeds 300 per 100,000. Blacks in North Carolina’s migrant labor camps suffer a staggering 3600 cases per 100,000, Newsweek reported, more than ten times the case rate in sub-Saharan Africa. (When a health worker last year tested 393 migrant workers in San Diego’s migrant labor camps, he came up with the happy, if baffling, finding that not a single one had the active disease, though many had positive skin tests.)
In most ways, New York City leads the nation’s TB horror File. The highest number of AIDS patients with TB live there; New York City officials say that more than half of the 3811 TB cases diagnosed in 1992 also were infected with HIV. In contrast, San Diego had about 40 such cases last year. “That’s still a small number,” says Catanzaro, the UCSD-based TB specialist. “But when you figure we didn’t have any just five years ago, that’s something to worry about.” In 1992, 19 percent of New York’s TB patients were resistant to the two best drugs for treating the disease, next to which San Diego’s number of comparable cases — eight in 1992, or less than two percent of the total — seems inconsequential. But any amount of some kinds of multiple-drug-resistant TB is frightening.
To better understand this, I spoke with Dr. Ted Heffernan, an infectious-disease specialist at UCSD. He pointed out that many people have the wrong idea about drug-resistant TB; they think it’s tuberculosis that has become drug-resistant in response to the antibiotics used against it. In fact, drug-resistant forms of Mycobacterium tuberculosis exist in nature. They are mutants, but they develop at random. “It’s just Darwin,” says Heffernan. “Evolution is too smart to have all these bugs be identical.” Get a non-drug-resistant TB germ in your lungs — one that’s susceptible to everything — and it will start reproducing other drug-susceptible TB germs. But out of every million or so bugs reproduced, a non-susceptible (drug-resistant) one will come into being, even if you never go anywhere near a medicine bottle. “Bugs aren’t stupid, despite the fact that they don’t have brains,” Heffernan says. “There’s always genetic diversity in a population.”
The mutants aren’t necessarily superior; for example, they may not synthesize certain proteins as well as do standard TB bacilli. Evolution, after all, has refined the standard bugs for millions of years, Heffernan says. But when humans add an antibiotic to the picture, everything changes. The relatively weaker mutants suddenly have a big advantage (their drug resistance) and “they become the survivors.”
Medical researchers became aware of TB’s capacity for outflanking drugs almost immediately after the discovery of streptomycin. One early study found that patients treated with it improved for about four weeks (as the drug-susceptible bugs faltered), then began to languish again (as the streptomycin-resistant subpopulation continued to grow and thrive). Scientists quickly delivered a counter-punch: giving the TB sufferers two different kinds of drugs, such as INH (invented in 1952) plus PAS or streptomycin. Heffernan elaborates, “If it takes 10 to the 6th (one million) bugs to get one that’s INH-resistant, and it takes 10 to the 6th to get one that’s streptomycin-resistant, you’re going to need 10 to the 12th bugs — or a trillion — before you find one that’s resistant to both drugs.” Since most TB victims don’t have that many TB germs inside them, the multiple drug therapy has worked very well. Modified over the years (as additional drugs came along), the standard therapy today involves giving up to four drugs that must be taken for about six months.
The catch is that if a patient fails to take all the drugs for the period of time necessary to kill all the bugs, he may actually set up conditions for one of the mutant strains to predominate, for instance, the strain that’s impervious to INH. If this patient coughs out those INH-resistant germs, and somebody else breathes them in, they’ll come down with INH-resistant TB. When that happens often enough “you begin to have areas of the world, or subpopulations in the U.S., where you have a reservoir of people who have resistant TB,” says Heffernan, adding that this is now the case in both the Philippines and New York City.
Only one more step is necessary for a multi-drug-resistant strain of TB to emerge: not getting the right medicines or not taking them for long enough. If someone has TB that’s resistant to the two best anti-tubercular drugs, INH and rifampin, he has a 50 percent or lower chance of cure, even aided by all the remaining drugs, states Heffernan. His colleague Catanzaro echoes, “We have had about 12 to 15 drugs that we’ve been able to use against tuberculosis, and we’ve known for some time that 2 or 3 are enough. So we figured we had lots of cushion. But when we start finding cases that are resistant to INH, resistant to rifampin, all of a sudden we’re realizing, yeah, we’ve got another 13 or so, but they’re very weak! I mean, they’re so weak it’s pathetic! When you lose INH and rifampin, you are in deep yogurt!”
San Diego isn’t yet in that plight. Though the number of INH- and rifampin-resistant cases has been climbing, last year’s eight cases are hardly cause for panic. Heffernan offers the further reassurance that drug-resistant TB is somewhat harder to catch than regular TB — which in itself is not extraordinarily infectious. “It’s not like chicken pox or measles or pneumonic plague,” the doctor comments. Despite its history of carnage, Mycobacterium tuberculosis humanis has to overcome some formidable hurdles before it can take up residence in someone’s alveolus. It has to get past the person’s defense system against airborne invaders — all the hairs and mucus and cilia lining the nose, trachea, and bronchi. It’s almost always harmless if swallowed. Although it can float in the air for weeks, if it floats into direct sunshine, it will die within seconds (destroyed by the ultraviolet rays). Outdoors there’s so much air relative to the size of the bugs that they’re almost impossible to catch. But even indoors it takes an average of 400 hours of exposure before household members of TB victims get infected, studies have shown.
That doesn’t mean it isn’t important to try to limit TB’s spread, particularly in light of its increasing incidence, which most observers attribute to the rise of social problems such as homelessness, AIDS, and uncontrolled immigration. For the past year, Heffernan has been focusing on the UCSP Medical Center, where 50 TB patients were hospitalized in 1992. Hospitals, of course, are particularly vulnerable places — they harbor people who are actively infectious (some diagnosed, others not). Medical workers do procedures that bring them into much closer contact with the germs than the average household member. Catanzaro, for example, tells of a case at UCSD where the medical staff threaded a lighted tube into the lungs of a pneumonia patient to try to identify what type of pneumonia the person had (this procedure is known as a bronchoscopy). Only later did it become clear that the patient had TB, and testing revealed that 16 people had become infected during the exam, among them “the intern, the resident, the attending [physician], the fellow, several nurses, the respiratory tech, even the poor secretary sitting by the door!” says Catanzaro. “From that one bronchoscopy!”
UCSD’s hospital doesn’t have the additional problem that many facilities acquired in the energy-crisis days of the ’70s, namely, closed ventilation systems that recirculate their air. At the UCSD Medical Center, air flows from each patient room directly to the roof, with fresh air drawn in constantly. But the UCSD facility was unable to build any rooms specially designed to have negative air pressure, which keeps the microorganisms from flowing out into the corridor. For a long time, “when no one was worried anymore about TB,” in Heffernan’s words, state regulators wouldn't allow such rooms in hospitals because of their impact on Fire safety. The rules changed recently, but now it would cost USCD hundreds of thousands of dollars to tear out and replace the duct work necessary to create the invisible germ barriers.
Heffernan says he and the hospital’s environmental safety officer finally got the idea of testing the private rooms to sec if any of them accidentally had negative pressure. They found eight that are persistently negative, “So that’s where we’ve been putting our TB or suspect-TB patients. It’s an ad hoc solution.” And Heffernan has been investigating other cheap and easy ways to lessen the chances of the disease spreading, such as installing portable air filters in both the hospital’s in-patient rooms and its AIDS clinic. But Heffernan offers the opinion that “the heart of TB control is not all the stuff the regulatory agencies are talking about, all the reengineering...in the hospital.” He says, “The way to control this epidemic is to put our increasingly finite resources at the front end: having outreach programs, supporting public health....”
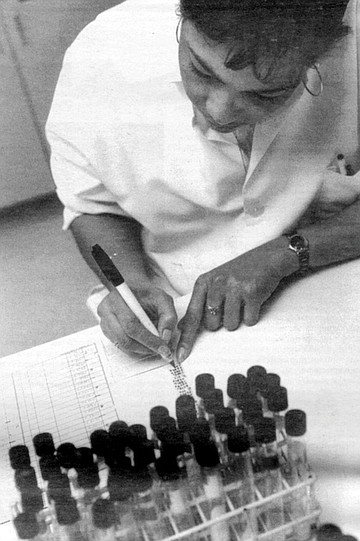
Cheryl Dalton toils in those trenches. Whenever any doctor anywhere in San Diego County diagnoses or even suspects a case of TB, he or she must report it to the county health department. The health department then uses its corps of public health nurses to try to insure that everyone who has TB gets cured of it, so they won’t make more people sick. The county’s 50 public health nurses thus play a role that’s part cop, part nagging mother, part UN diplomat, part guardian angel. In the South Bay Health Center, Dalton and six other full- and part-time public health nurses fill those roles, and as the “TB specialist,” it is Dalton who makes the first visit to the home of every single person diagnosed with TB in the South Bay, from Southeast San Diego to the Mexican border.
On the afternoon I met with her, she said she had wanted to take me to the home of a newly diagnosed patient so I could observe the teaching necessary on the first visit. “But there’s such a privacy about this disease that I couldn’t find [one] who would allow a reporter in,” she said. “In fact, many of the patients that I’ve worked with for a long time wouldn’t [open up to an outsider] because of the stigma.” Three had agreed, and we would be visiting them.
According to Dalton, the Chula Vista clinic normally follows about 140 TB patients. Many are poor and non-white, though they can come from anywhere on the socioeconomic spectrum. Dalton recently attended to one upper-middle-class high school teacher from Bonita, for example. At the other extreme, the public health nurses sometimes visit people living in their cars. “We’ve had nurses who’ve had active cases in crack houses. You drive around the house a couple of times to make sure there’s not a drug deal going down at that moment. You go to the door, and the hand comes out to get the medicine!”
At 38, Dalton has been a nurse for 15 years, with the last 5 spent in public health. “And I love this work,” she says. “I have a passion for it. Because we’re dealing with the whole family. We’re not just treating a disease.... Maybe there’s no food in the house. We know how to get food. We know how to get diapers for the baby. Satisfy some of those basic needs, and then you can do health care.”
The public health nurses visit each TB patient at least three times. After the initial diagnosis is made, Dalton goes out and administers skin tests to everyone else living in the household, and sometimes to co-workers or schoolmates of the sick person. If those tests show that others have been infected, they also may have to take medicine to protect them from getting active TB. About a month later, a public health nurse returns to assess whether the TB patient is “compliant” — that is, taking his or her medicine. If nothing looks suspicious, the nurse will return only once every three or four months until the treatment ends.
But many people need closer supervision. Dalton tells the story of one alcoholic with advanced tuberculosis. Dalton suspected he might have trouble taking his pills on his own and decided to monitor him weekly. She took him a seven-compartment pill case with each day clearly marked. “I filled it up for him every week, and I said to myself, 'I’m doing such a good job!’ ” And then one day, “one of the other little old drunks in the house took me aside one time when [the patient] wasn’t there and told me he wasn’t taking his pills.” The informant advised Dalton to check inside the household’s oatmeal box. “So I go in the big, roach-infested kitchen. I open the cupboards and I peek into the oatmeal box, and there’s, like, 200 pills! Every week he would dump them all in!” At the memory, Dalton laughs uproariously.
Dalton placed that patient on “directly observed therapy” or DOT, in the jargon of the TB healers. The nurse actually watches such patients put the pills in their mouths; she watches them swallow. “Some patients will try to tongue the pills.” Patients are supposed to be on their honor over the weekends — but the nurses don’t count toward the completion of the therapy any pills that they haven’t actually witnessed being consumed. Dalton says that at any time the Chula Vista office usually has from 23 to 26 DOT patients. On the afternoon that I accompanied her, we visited one named Willie Lee Smith.
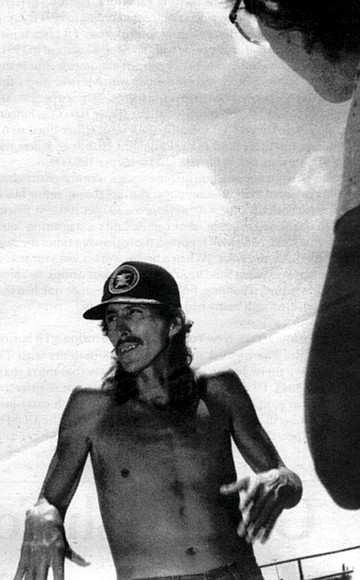
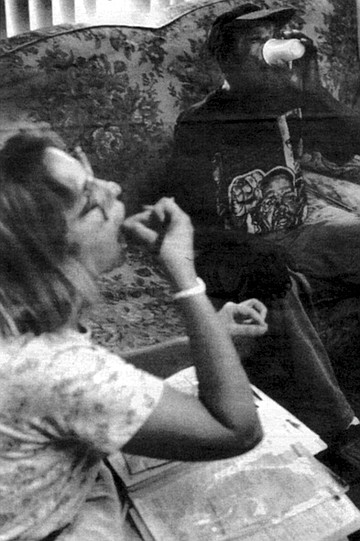
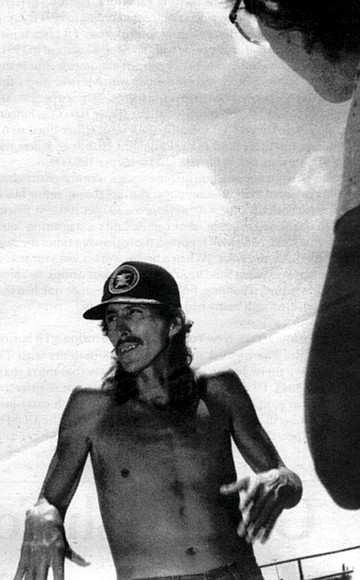
Smith lives in a surprisingly rural patch of Southeast San Diego; you reach his home by driving down an unpaved lane next to an open field. That day, heavy fruit hung from robust tomato plants in his front yard. Dalton greeted a few of Smith’s housemates as if they were old friends, then proceeded into the bungalow. Out of the dim interior emerged the figure of her patient, an emaciated black man wearing a baseball cap and a Malcolm X T-shirt. He looked 60, but when I asked his age he replied, “I’m 42.”
“Willie was real sick with TB,” Dalton said, sympathetically. “He had to go to the hospital.”
“I was feelin’ real tired and, well, I couldn’t eat nothin’. I was just feelin’ bad and losing weight all at the same time. I thought it might be comin’ from smokin’, and so I slacked off from smoking.”
“Which is very common,” Dalton interjected. “They’ll treat themselves. They’ll take cough medicine. They’ll stop smoking. They’ll do all these measures before they go to a doctor.”
When Smith began coughing up blood, he finally sought medical help. He was astonished to hear he had TB. He says he has no idea where he might have contracted the disease. “You can’t really tell who gave who because, see, germs, they spread.”
After about a month in the UCSD Medical Center, during which his weight fell to a skeletal 112, Smith finally improved enough to be discharged, but the pills caused several side effects, and “I forgot to take the medicine,” he told me. Under Dalton’s watchful eye since May, Smith would be completing his treatment in a month or two. He gulped his nine large pills in one swallow.
“I’ve got some people on 20 pills a day,” Dalton commented as we sped south again on I-5. Side effects are common. “They make you feel nauseated. A lot of people vomit. They make you feel tired. They make you feel headachy. They make you itch like crazy.” Dalton says the second- and third-line drugs taken by victims of drug-resistant TB are even worse. “Patients can lose their hearing. Or I have one guy who’s on this medication that turns your skin black/purple. He looks like the night!” Other patients “just look at their medicine and they vomit. And they’ve got to take them for so long!” (about two years, compared to the six-month regime for non-drug-resistant TB). “Can you imagine vomiting every day for two years?” Dalton asked.
Such side effects explain why some people don’t finish taking the medicine. Other people wrestle with denial. Dalton says, “TB has such a cultural stigma to it! We have Filipinos, Somalians, many Indochinese. There’s Laotian, Cambodian — you name it, we see it. And in their culture, if they get TB, they’re removed from the home.” Dalton recalls one case involving a young Mexican woman who was diagnosed in Mexico as having TB of the kidneys. “Her family from Mexico was so freaked by the TB diagnosis that they came up and took her child away from her! They told her to sterilize all her dishes and everything.” When Dalton visited her in a tiny trailer in San Ysidro, she had sprayed every surface with Lysol. “I could hardly breathe! She said her family told her to do this. I said, ‘Well, you know, if you took your urine and spritzed it all over the house, it might spread the disease. But it’s not infectious.’ ” In fact, tests here never did grow disease from the girl’s urine samples. “But her family took her baby away for four months!” Dalton says.
Faced with such reprisals, “People say, ‘I don’t have TB. Not me! I have pneumonia.’ Or they won’t take their medicine because they don’t believe they have TB. Or they’ll kind of take it and they kind of won’t.”
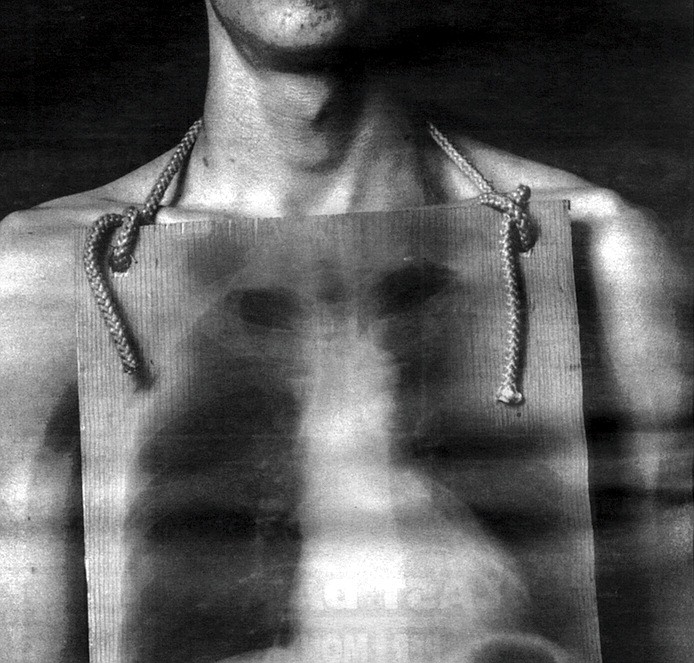
Dalton’s second appointment that afternoon took her to Sandi’s Rental Stables on Hollister Road, not far from the border. Her patient here was Jose, a 27-year-old Mexican who shoes horses for a living. He had a strain of TB resistant to both INH and ethambutol, another first-line drug. To combat the disease, he was taking seven pills a day and getting a daily injection of streptomycin, administered by Dalton. At her arrival, lose materialized, looking shy but cordial. He wore jeans but no shirt, showing off a lean but muscled torso that hardly looked ravaged by disease. “I was coughing up a lot of green stuff,” he recalled. When he visited his family in Mexico City, Jose’s mother heard him coughing at night. “My mom know. My mom told me first about tuberculosis. But I never believe it,” he said. When he returned to San Diego, he sought a skin test at the health department, which confirmed his mother’s diagnosis.
Dalton called José into the privacy of the stables office, where she injected an ampule of thick yellow streptomycin into his buttocks. “It hurts a lot. It really burns,” she said later. But the painful treatment appeared to be working. Although Jose had been prohibited by the county from working for two or three months, tests of his sputum had finally shown him to be non-infectious, so he was able to make a living again. “A week ago, he was wearing a mask when I went to see him,” Dalton explained. Not that a mask does much good. “The droplet nuclei go right through a mask,” Dalton said wryly. So what do the nurses do to protect themselves from infection? “You look at your case,” Dalton answered. “If I have a four-plus, smear-positive, real infectious case, I’ll go in and if it’s a really dosed-in place. I’ll stay near the door.” Sometimes she asks patients to open windows, and she reminds them to cough into a tissue. All the nurses get regular skin tests, and finally, “You know, you just kind of say a little prayer when you go in.” She laughed again.
Health officials say most patients welcome the nurses, but every so often someone reacts differently. Says UCSD’s Catanzaro, “I’ll never forget a woman I diagnosed a few years ago as having TB. I sat down and explained what that meant, and she said, ‘You mean I can make somebody sick just by breathing on them?’ And I said yeah, and she said, ‘Cooool!’ She was a working prostitute, and when she left the hospital, even though we made the liaison with the health department, she made an effort not to be found.”
In such cases, county officials can issue an “order of isolation and quarantine,” and if the patient ignores the order he can be sent to jail. Moser of the health department says three or four people per year have been incarcerated (at the Vista Jail, which has respiratory isolation rooms) for that reason, though in many cases judges have ordered them released before their treatment was over. “And every time except once, out of about eight or nine cases, it has failed,” says Moser. “The people just disappear; we never see them again.”
If open hostility to the public health nurses is rare, Dalton says cultural differences create daily pitfalls. “When I go into Indochinese homes, I take off my shoes. I use an interpreter. I understand not to look at the women but to look at the men. You have to learn how to avoid offending them.” She says among the most difficult groups to work with are the Somalian refugees, who have a very high TB rate. “They almost all have to be on supervised therapy, because they don’t take their medicine. They’re a very male-dominant culture,” she says. “This is what happens. I go into the house. The man is very arrogant. ‘You come here. I show you how to cure arthritis.’ And there’s a young woman sitting at his feet, rubbing his leg with Wesson oil. She takes a razor— this is no lie! — and she cuts his leg and puts a cow’s horn on top of the cut to pull out the blood, which relieves the poison in the body to relieve the arthritis. It’s this kind of health practice that we’re dealing with. If they have a headache, they cut their head to bleed it.”
Subtler factors complicated the case of 15-year-old Paola, Dalton’s third and final patient of this afternoon. Paola lives with her family in a tidy, new-looking neighborhood just west of San Ysidro. “I’m sorry the house is such a mess,” she apologized as we arrived. It looked spotless, and it was hard to believe Paola’s lungs were any less immaculate. A sturdy girl with pretty eyes, she wore her thick, glossy hair pulled back with a hair ornament that looked as if it should be decorating a birthday present.
She explained that a routine TB skin test last fall had revealed that she and several family members were infected. The family’s doctor ordered a course of preventive medicine, which Paola took for a while, then abandoned. And why? “Because [the doctor] told me to take it in the morning when I had eaten breakfast, and I don’t eat breakfast, so I kept forgetting to take it,” the teenager explained. “Also I had it in my cabinet in the bathroom, so it wasn’t visible.”
A few months later, her mother saw a television news report about TB and was worried enough by it to take Paola back for a recheck. “I had no symptoms or nothing,” Paola recalls — but this time an X-ray showed the TB germs to be eating away at one of her lungs. Paola then had to begin taking three different types of medication a day, with the public health nurses stopping by every two to four weeks to do “pill counts” to check on her compliance.
“And she’s perfect on her count this time!” Dalton announced, beaming. She thus wouldn’t schedule another visit to Paola’s home for a full month. But she gently ordered the girl to let her know when she had rescheduled a doctor’s visit the girl had skipped because it conflicted with her school exams.
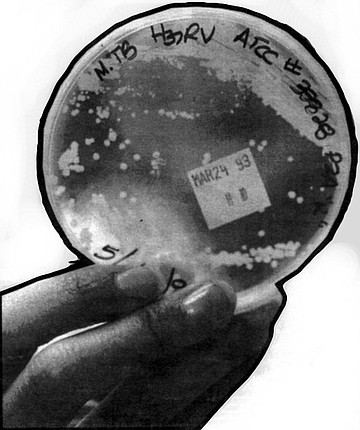
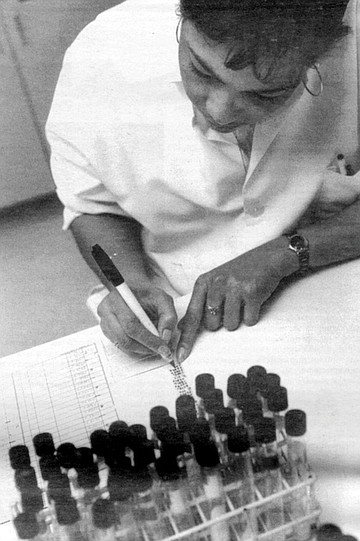
Driving back to the Chula Vista clinic, Dalton mentioned that she had recently toured the county’s TB lab, where much of the identification and testing of the germs takes place. An enthusiastic person, Dalton grew even more animated describing the facility. She urged me to visit it, and so one recent Wednesday I entered the large complex just east of the Midway/Rosecrans intersection.
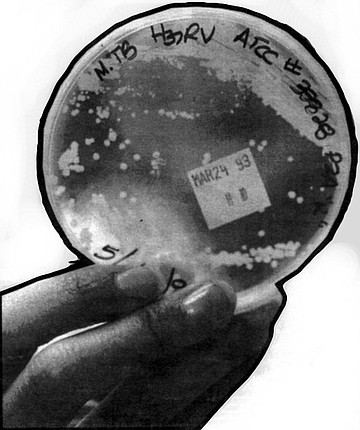
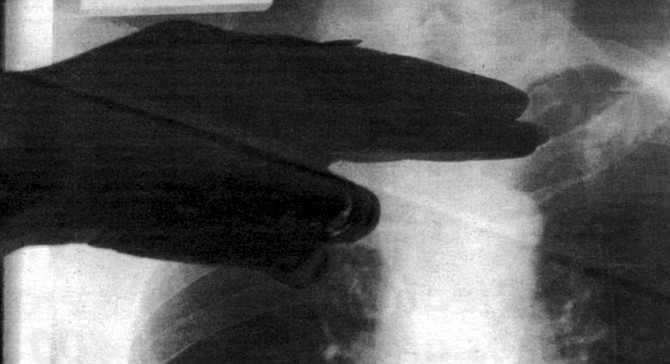
This building used to be Fedmart’s corporate headquarters; today the TB lab is located down a maze of corridors deep within it. It’s not a huge space, and it’s cluttered with instruments and work benches and cabinets and test tubes and papers. Tightly stoppered vials of sputum arrive three times a week; some of them are teaming with TB bacteria. Every time the microbiologists and lab assistants open a vial or one of the Petri dishes in which they culture the bacteria, they don gloves and lab coats and withdraw into one of two isolation chambers in the innermost recesses of the lab. These chambers are flooded with ultraviolet light when empty. When workers enter, they switch the lights off, but as much as possible, they keep their hands and the TB containers inside a long “biological safety cabinet.” Air inside the cabinet is drawn up into a smaller metal chamber containing a filter that traps particles down to less than a micron, then exhausts the purified air to the outside. If ever any container cracks or breaks, the lab personnel follow a rigid set of decontamination procedures.
Here, in the laboratory, tuberculosis seems most real. It’s alive, growing under the microscope, mushrooming into colonies you can see unaided. It also seems least fearsome; I could understand why Dalton so liked the place. Amidst all the devices for studying them and containing them, the teeny germs (which killed more than three million human beings around the world last year) seem like they shouldn’t have a chance against us.

Recently I looked through a microscope at a small colony of the creatures that cause tuberculosis in humans. About a hundred of them had woven themselves into a long structure that — magnified 1000 times — looked like a badly fraying section of rope stained bright fuchsia. The creatures didn’t appear to be moving, and a county microbiologist assured me that right after being placed on the slide, they had been baked to death.
Amid all the dinosaur hoopla this summer, I thought a lot about those minuscule bugs. No one will ever make a horror film about Mycobacteria tuberculosis humanis. They’re too tiny, each individual less than a 6400th of an inch long. They have no personality. Yet they’ve killed more people than any sharp-toothed monsters. They’ve killed more than all of humanity’s wars — at least a billion victims in just the 19th and 20th centuries. A hundred years ago, one out of every five people in their 30s and 40s died from being eaten alive by them.
And their grisly work continues. Last year tubercle bacilli were discovered to be munching away on the lungs and other parts of 457 San Diego County residents. That means about 18 out of every 100,000 people who live here were struck by the disease, a rate that has more than doubled since 1984. Among those TB victims, some had strains of the bacillus that can’t be cured with standard drugs. “To be perfectly honest, I and most of the people who are familiar with TB are scared to death right now,” says UCSD’s Dr. Antonino Catanzaro, who just chaired a statewide Tuberculosis Elimination Task Force. “Since I’ve been a doctor, we’ve always felt relatively comfortable about TB. We had the tools we needed to handle it.” Now all of a sudden “we’ve been robbed of those tools. This multiple-drug-resistant TB has robbed us of them.... And that is what’s gotten people really scared! They think about what happened to the world 100 years ago, and they’re saying, ‘My God, is this in our future?’”
Catanzaro points out another of TB’s most frightening aspects: the fact that it can attack virtually anyone. It spreads when someone with TB-ravaged lungs coughs or sings or even talks in a voice loud enough to propel invisible drops of sputum into the air. Once these “droplet nuclei” dry out, the TB bugs act like dust particles; they can float on the air currents, fully potent, for days or even weeks. If you walk into the room where they’re floating and you happen to inhale a liter of air containing them, you can get infected. “You don’t have to be doing illicit things and you don’t have to be sick,” says Catanzaro. “You can be perfectly normal.”
Actual infection takes place when a bacillus settles onto the moist, dark surface of one of the lung’s air sacs. In this oxygen-rich environment, TB germs thrive. They grow slowly, dividing only about once per day, and they face immediate attack by the body’s immune system. But the tubercle bacilli are tough, protected by a waxy armor that withstands most of the body’s defenders. Even the macrophages (defensive cells that scout for, attack, and internalize foreign substances) rarely kill all the TB germs. They kill some and slow the growth of the remainder, but they usually wind up carrying the latter into the lymph nodes and throughout the bloodstream, seeding them in the brain, bones, and other organs. Only weeks after the infection begins do T-cells start to produce chemicals called lymphokines that help the macrophages destroy the invaders. At this point, 95 percent of those who’ve been infected with TB win at least a partial victory as their immune system kills or immobilizes the tubercle bacilli so well that the infected persons never appear sick. The only way they’re likely to know they were infected is by having a positive TB skin test or by developing active TB at some point later in life. This delayed onset of the disease happens to about five percent of all those infected; the TB germs can lie dormant for decades then begin to grow and attack anew when something weakens the body’s defenses.
For those ten percent of infected people who develop active disease (either immediately or later in life), the illness can run a course lasting from months to years, producing symptoms known all too well in the 18th and 19th centuries. Sufferers coughed, of course, and they typically ran fevers that peaked each afternoon, disappearing by the following morning. They grew thin and pale, at times feeling exhausted, at other times seized by flurries of activity marked by flushed cheeks and glittering eyes.
Such associations made their way into a broad literature that suggested that “consumption” (as TB was called then) somehow refined its victims, elevating them to a more spiritual plane. It was perceived to be “a gentle death,” according to literary critic and TB historian Mark Caldwell, who writes, “It was a badge of refinement, it was very nearly a polite accomplishment.” Among the writers, musicians, and artists afflicted by it were Modigliani, Paganini, Chopin, Emerson, Thoreau, Poe, Keats, Shelley, Trollope, Chekhov, and the entire Brontë family.
Many 18th- and 19th-century writers gave TB to their characters, particularly those in need of a vague and rapturous demise. But less than 30 years after the beatific deaths of Dora in David Copperfield and Eva in Uncle Tom's Cabin, pathologists began to look at what was really happening in the bodies of TB victims. Autopsies revealed gaping holes in the lungs, where the gluttonous bacilli — now numbering in the millions — as well as the body’s own defender cells literally dissolved the tissue, to be coughed up in the glutinous sputum. In some cases, blood vessels eroded — explaining the frightening instances in which sufferers also coughed up bright red blood. Fibrin, a product of coagulated blood, coated the lungs and pleura of some of the corpses. Purulent fluid filled the chest cavities.
As vivid as were these revelations, the news about TB that rocked European medical men was a 1882 announcement by the German bacteriologist Robert Koch. He had isolated a bacillus, then devised experiments with guinea pigs that proved the microorganism caused TB. Up to then, many people had no idea the disease could be transmitted. John Keats, for example, who had studied medicine in London before turning to poetry, spent months tending to his tubercular brother in tightly shuttered rooms. As the public ever so slowly became aware of TB’s infectiousness, people could begin to check its spread.
But a cure for TB proved far more elusive and was “not to be sought in drugs,” the San Diego Union informed its readers one day in May of 1883. “A long and fruitless search [for such a drug] has been in progress for hundreds of years and...none has been found and none ever will be found.” Hundreds of persons had been cured of the disease, the newspaper declared, but “pure air” was the key to improved health. “Many have been cured in an advanced stage of the disease by passing most of their time outdoors, engaged in some light employment. The consumptive must not allow a fear of the weather to keep him within doors. He must...keep out in nearly all kinds of weather.”
The notion that one’s surroundings could help one recover from TB was hardly news. In ancient Rome, sufferers sought warm, dry climates. By the 19th Century, the search for health was taking the tuberculous in a confusing number of directions. Washington Irving tried to mend his lungs in Canada and later Europe, while the poet Sydney Lanier headed for Florida. Robert Louis Stevenson journeyed from Scotland to New York to Tahiti, and Cecil Rhodes believed that the air of South Africa made him well again.
In the mid-1800s, the equation of cure with setting became more complicated as the first great TB sanatoria opened in what is now Poland and Western Germany. One therapeutic model required patients to exercise, take cold showers, and eat massive meals. Another demanded absolute bed rest. In the United States, the Adirondack Mountains enjoyed a reputation for restoring well-being, and in 1885 the first American sanatorium was opened there at Saranac Lake by Edward Livingston Trudeau (great-grandfather of the cartoonist Garry).
By 1935 some 471 full-fledged American sanatoria had come into being, with another 418 TB departments operating in connection with hospitals. The sanatoria tended to cluster in “healthful” locations, but theories about just what constituted healthfulness again varied wildly. The Adirondacks, and Saranac Lake in particular, remained a mecca, but Colorado attracted high-altitude partisans. (Today the most famous center for TB research is at the National Jewish Center for Immunology and Respiratory Medicine in Denver.) The entire Southwest lured those who thought a mild climate most beneficial, and San Diego was no exception.
As early as 1885, the same year Trudeau opened his Little Red Cottage, TB victims were making their way here, according to one oral history on file in the San Diego County Historical Society’s archives. In this document, a San Diego immigrant named Hattie Kaufman describes moving to Alpine where there was “a kind of sanitarium... with lots of tents with beds in them.... We never had less than 10 or 15 consumptive people there with tuberculosis.... There were no facilities to take care of them in San Diego. These people were sent out here from the East, and as there was so much fog in San Diego, the doctors would send them on up to Alpine, where there wasn’t any fog.”
The influx of hopeful “lungers” accelerated as San Diego entered the 20th Century. By the summer of 1920, when the county had a population of 74,000, the State Bureau of Tuberculosis dispatched a field worker named Ida M. Theile to assess conditions here. “The Indians thru the County are very susceptible,” she reported, adding that by one estimate, 75 to 80 percent of the entire Indian population was infected. “Their superstition and ignorance and unsanitary method of living make them especially good subjects.” But they were hardly alone. San Diego’s resident Mexicans “are infected to a great extent,” Theile wrote, and “La Mesa and East San Diego afford an excellent climate for the tuberculous and so are to a great extent resorts.” She noted that National City and Escondido lured their share of patients, and “the equable climate of San Diego attracts many.... Some have sufficient funds...and are no great problem, but many others come with little more money than is needed to bring them here, and in all stages of the disease, occasionally even dying on the train before it reaches the city. The rooming houses are full of them, but no precautions are taken when they die or leave. These people present a serious problem. They are not careful in their habits. The rooms are poorly renovated if at all after they leave.”
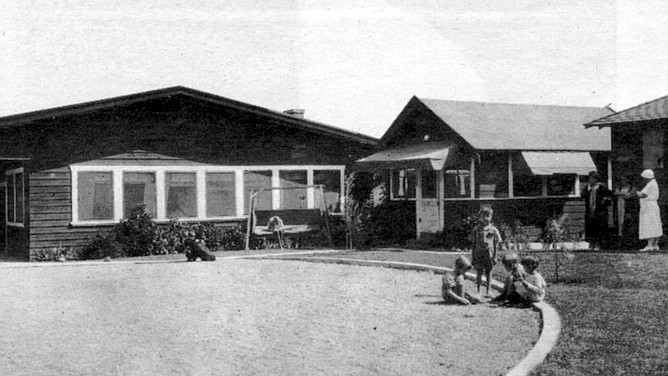
In addition to the boarding houses, two major institutions were accepting tubercular patients in 1920. The oldest was Rest Haven, established in 1913 by the San Diego Society for the Study and Prevention of Tuberculosis. Originally an open -air camp, it evolved by the late 1930s into an elaborate complex including a hospital building (still in use today as Villa View Community Hospital). During World War I, Rest Haven restricted its care to servicemen with TB, but by 1920 it had modified its mission to care for children aged 3 to 12 who were in an anemic condition or who had had contact with TB.
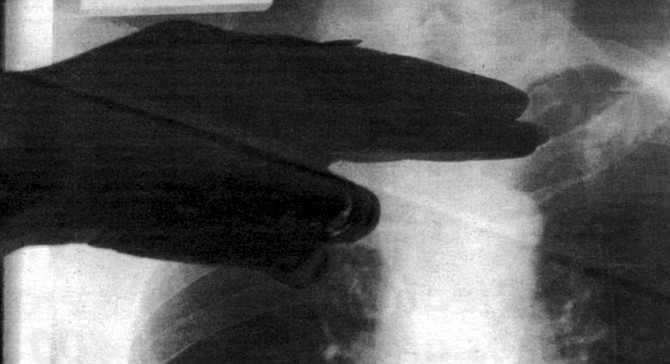
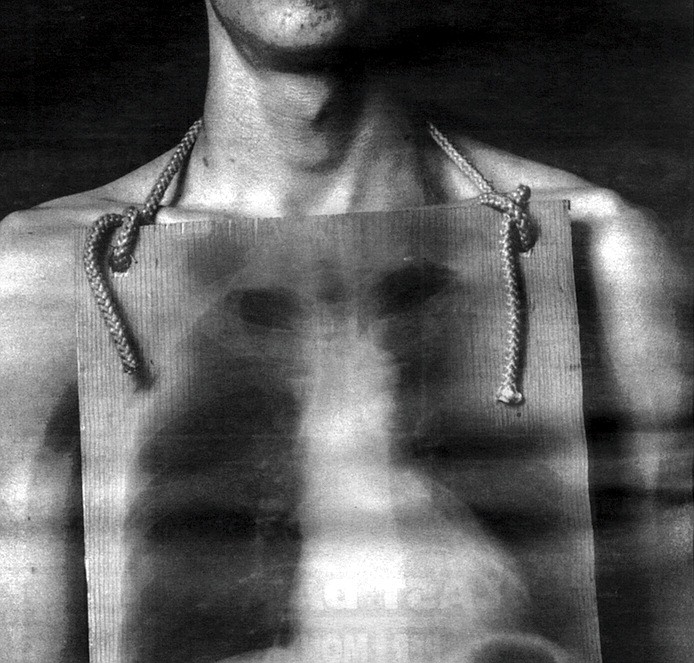
Eventually, Rest Haven accepted youngsters with a wide range of medical problems, but TB always numbered among the criteria for admission. One person who recalls the Rest Haven regime in the early 1940s is Stella Larson, today a resident of Imperial Beach. Around 1940, when Larson was about ten, she was living in La Jolla at the Gillispie Welfare Cottage on Girard Street. (Her mother’s death had resulted in her family’s breaking up.) Larson says when she began fainting and “started spitting up a lot,” X-rays revealed spots on her lungs. “The doctors must have talked it over and decided I wasn’t sick enough to go to [the county’s TB facility].” So they dispatched her to Rest Haven.
Located not far from what is now 54th Street and El Cajon Boulevard, Rest Haven then felt like a country retreat, according to Larson. Her first three weeks were spent in an isolation room. “I didn’t like it there, I know that!” she says today. “I didn’t like it because it was new and strange and I missed my home.” Still Larson adjusted quickly. “I could control that cough, and I didn’t cough in anybody’s face,” she says today with some pride. After her three-week quarantine, she moved into a dormitory and donned the Rest Haven uniform for girls: shorts and a bolero-style sun top tied around the back and at the neck. “We had to wear that all the time. Even in winter! Though they let us put our sweaters on and we didn’t go out as much when it was cold.”
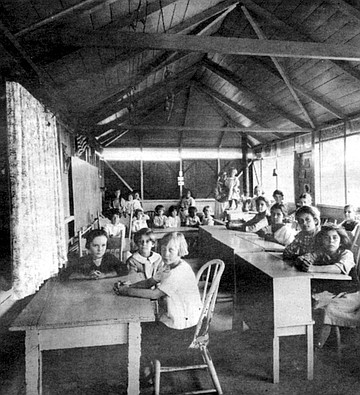
Education for Rest Haven’s inmates took place in a one-room schoolhouse that had opened in 1925. But outside of class, no special exercises were mandated. “We were just supposed to go outside and play like a normal kid does. They had a collie dog, and he used to follow us around, I remember that. Also they had a berry patch, and I enjoyed that.” Larson was eventually discharged in 1945, apparently healthy.
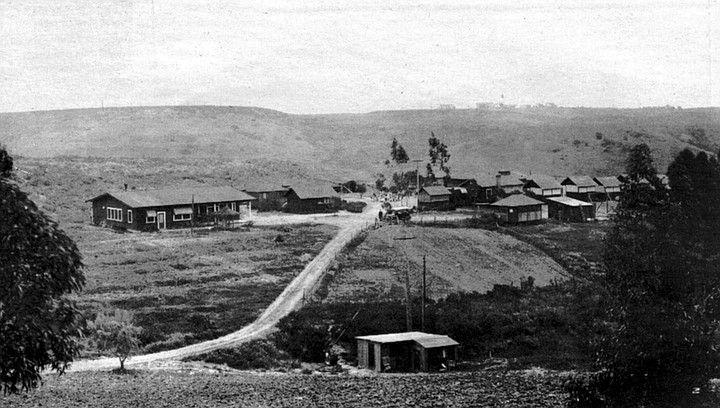
San Diego’s other major TB institution, Vauclain Home, was less bucolic. It took its name from John Vauclain, a Pennsylvanian who came to San Diego in 1887 in search of a climatic cure. No hotel or rooming house at that time would take him in because of his illness, so he bought a home on the northeast corner of Second Avenue and Cedar Street downtown; there he recovered his health and lived until 1909. In his will, he left a third of his estate to establish a TB colony, and his executors finally acquired some land in Normal Heights where they erected tent houses. That enterprise failed, and in 1918 the managers turned over the property and some cash to the county, which ordered a facility to be built on a 45-acre site overlooking Mission Valley that came to be known as Vauclain Point.
Located about a mile from the old county hospital (now UCSD Medical Center), across the canyon from it, Vauclain Home came into being in 1919, just as sanatoria were reaching their heyday. But in some regards, the San Diego facility differed from the archetype established in upstate New York and replicated throughout the country.
Mark Caldwell, whose book The Last Crusade is largely devoted to an analysis of sanatorium culture, describes the typical sanatorium as a totalitarian realm where adherence to certain notions was carried to cultish excess. By 1916 rest had “become the dominant factor in sanatorium routine, replacing exercise, which was allowed in increasing doses only as the patient edged toward normal life,” Caldwell writes. “But inactivity, crucial though it was in the sanatorium, implied passivity and helplessness. Resting outdoors, day and night, summer and winter, made rest into a challenge....”
Patients at many facilities thus were carted outside even when winter temperatures fell below freezing. “Detailed instructions were introduced about everything from the way patients were to inhale the outdoor air to the lounge equipment and bodily positions they used to ingest it,” Caldwell writes. Other daily routines were also spelled out in obsessive detail, a systematization that “was not so much a direct treatment as a giant living metaphor of order, erected in the face of the unpredictable, as a bulwark against it.”
Though the rigidity made aspects of sanatorium life nightmarish, surprisingly few patients denounced the system. Cheerful submission was demanded, and there was daily indoctrination in the salubrious effects of positive thinking. In The Plague and I, one mordantly funny exception to the typical sugar-coated memoir, writer Betty MacDonald (author, also, of The Egg and I) described how the staff of her Seattle-area sanatorium dished up daily “beautiful thoughts” along with each meal (“If you must be blue, be a BRIGHT blue!”) while at the same time prohibiting bedridden patients from reading or even talking with their roommates and forcing them to endure the cold wind and rain that streamed in their perennially open windows. In San Diego’s Vauclain Home, optimism was de rigueur. One 1939 newspaper article twinkled that “Visitors may search the children’s ward from corner to corner, and they will find neither hide nor hair of Old Man Gloom...for cheerfulness is the rule....” A published statement from Vauclain patients proclaimed that “the mental attitude of the patient is 50 percent of the cure in tuberculosis.” But Vauclain imposed no unreasonable demands on its patients, at least not according to William Weathers’s recollection.
Weathers has lived in San Diego for all but five of his 79 years. In 1940 he had just gone to work for the post office, carrying special delivery mail and earning an average of $22 per week. “I used to work my tail off. The more mail I delivered, the more money I made.” Then his back began to hurt. Weathers says at first he thought an old work-related injury was causing the pain, but it increased to the point where he remembers lying in bed at night and having to grab one side of his pajamas to turn himself over. When he also began having night sweats, he saw a doctor, who diagnosed tuberculosis of the spine. “I said, ‘How long’s it gonna take [to get well]?’ He said, ‘You’ll probably be off the job about a year.’ And I said, ‘Open a window and I’ll just jump out and get it all over with.’ ”
Things went better than Weathers anticipated. His wife, who hadn’t been working, got a job at the post office in his stead, and Vauclain Home accepted him for treatment at no charge. In the Hillcrest facility, Weathers says the doctors immediately placed him on a Bradford frame, a canvas bed stretched across a galvanized pipe framework. “It put a reverse arch in your back,” he explains. “I laid on that thing for I don’t know how long. The first week I thought I was gonna die because the curvature of my back was just the opposite of what it was originally.... It was so uncomfortable they finally rolled up a blanket and had me lay across that. I couldn’t turn or anything. If I had tried to move, I’d probably tip the thing over.”
Weathers recalls that at one point one of the X-ray technicians, who had worked in another sanatorium, told him he was lucky to be at Vauclain, that the San Diego sanatorium treated patients much better than did other TB establishments. Weathers could read (though it was difficult in his contorted position), and he could chat with other patients. “I remember I could look down the hall, just a little ways, and I used to talk to a girl in another ward there. We’d shout back and forth.” Weathers couldn’t play cards like other patients, but he listened to the radio, and at times the scene out his window entertained him. “The psychiatric hospital was right across the road from us, and about twice a week they’d take two or three people up to Patton (state mental hospital]. They didn’t have too much trouble with the men, but the girls used to fight ’em! They’d strap them in the back seat, and they were kickin’ and all. I always used to watch that.” He laughs.
“Practically every morning we’d hear about somebody passing away in the night,” Weathers recalls. But he never despaired about his own prognosis. “I just said to myself, if there’s any way to get out of here, the best way is to eat my way out. So everything they sat in front of me, I ate. When I went in there I weighed about 135 sopping wet.” One year later, weighing about 160 pounds and having undergone “spinal fusion” surgery, which he says immobilized the disintegrated vertebrae in his lower back, he was asked by one of the doctors if he’d like to go home. “I couldn’t believe it.” The memory makes his voice shaky. “I cried like a baby.”
By 1941, when Weathers was released, San Diego’s tuberculosis incidence had fallen to 70.5 cases per 100,000 residents (compared to 227.2 in 1920, the year of Nurse Theile’s report). Authorities still are debating why fewer people were catching TB then, both here and elsewhere. Was it the general rise in prosperity? Better health screening? Increased resistance bred through Darwinian-style pruning? Despite success stories like those of Stella Larson and William Weathers, the impact of the sanatorium movement remains unclear. According to historian Caldwell, “Consistently, from the beginning of the sanatorium movement through the 1940s, nearly 25 percent of all patients died while in the hospital, and 50 percent of all released patients succumbed within five years of discharge. Some institutions prided themselves on records better than this average, but these were often the ones that limited patients, as far as possible, to those with incipient tuberculosis and left the moribund to state and county hospitals.”
Unclouded victory over the tubercle bacillus came only with the drug discoveries of the 1940s and early ’50s. These began with the realization that a certain mold found naturally in soil, streptomyces, powerfully inhibited the growth of so-called “Gram-negative” bacteria, including Mycobacterium tuberculosis. (The TB germ produces an enzyme that destroys penicillin, that other famous mold byproduct.) Human experiments with the new drug, streptomycin, were generating great excitement by 1946, as was a second anti-tubercular substance discovered in Sweden, PAS (para-aminosalicylic acid). By 1952 a still more powerful antibiotic called isoniazid, or INH, appeared. Used in combination with the first drugs, it seemed at long last to give humanity truly lethal weapons against the ancient scourge.
From 51 cases per 100,000 population in 1953, San Diego’s TB incidence over the next five years plummeted: 43.7 in 1954, followed by 35.9, then 29.8, 25.2, 18.6. In 1964, with the rate at 14.3, Vauclain Home shut down; remaining TB patients moved into the county hospital. Although the incidence of tuberculosis fluctuated somewhat in the ’60s and ’70s, the basic trend continued downward through 1985, when only seven out of every 100,000 San Diegans were reported having the disease. Medical scientists envisioned TB germs being obliterated from the planet by the year 2010.
Then came the turn-around. From that low of 149 cases in 1985, the numbers jumped to 244 in 1987. Since 1988 they have climbed without interruption: 294 cases in 1989,346 in 1990,391 in 1991,458 last year. Dr. Kathleen Moser, San Diego County’s TB Control chief, calculates that San Diego has the seventh highest number of cases in the country. “An epidemic is when you see cases in excess of what you have expected, in a continuous manner. And in that sense, I believe we are in an epidemic,” Moser says.
What has happened in San Diego has been occurring all over the country — with some interesting variations. Here, 65 percent of the TB victims come from other countries (according to 1991 figures), whereas nationally the percentage of foreign-born TB cases is just 27 percent. Nearly half of all people with TB here (47 percent in 1991) are Hispanic, compared with just 20 percent nationwide. But many San Diego Hispanics have regular contact with Mexico, where the active TB rate has been estimated to run as high as 400 cases per 100,000 (compared to San Diego County’s current 18 per 100,000). Fifteen percent of San Diego’s TB cases in 1991 were either born in or descended from those born in the Philippine Islands — where the active TB rate may run as high as 1500 cases per 100,000.
The frightening situation in some foreign countries is matched by that in certain American subgroups. The rate among young black men in New York City, for instance, exceeds 300 per 100,000. Blacks in North Carolina’s migrant labor camps suffer a staggering 3600 cases per 100,000, Newsweek reported, more than ten times the case rate in sub-Saharan Africa. (When a health worker last year tested 393 migrant workers in San Diego’s migrant labor camps, he came up with the happy, if baffling, finding that not a single one had the active disease, though many had positive skin tests.)
In most ways, New York City leads the nation’s TB horror File. The highest number of AIDS patients with TB live there; New York City officials say that more than half of the 3811 TB cases diagnosed in 1992 also were infected with HIV. In contrast, San Diego had about 40 such cases last year. “That’s still a small number,” says Catanzaro, the UCSD-based TB specialist. “But when you figure we didn’t have any just five years ago, that’s something to worry about.” In 1992, 19 percent of New York’s TB patients were resistant to the two best drugs for treating the disease, next to which San Diego’s number of comparable cases — eight in 1992, or less than two percent of the total — seems inconsequential. But any amount of some kinds of multiple-drug-resistant TB is frightening.
To better understand this, I spoke with Dr. Ted Heffernan, an infectious-disease specialist at UCSD. He pointed out that many people have the wrong idea about drug-resistant TB; they think it’s tuberculosis that has become drug-resistant in response to the antibiotics used against it. In fact, drug-resistant forms of Mycobacterium tuberculosis exist in nature. They are mutants, but they develop at random. “It’s just Darwin,” says Heffernan. “Evolution is too smart to have all these bugs be identical.” Get a non-drug-resistant TB germ in your lungs — one that’s susceptible to everything — and it will start reproducing other drug-susceptible TB germs. But out of every million or so bugs reproduced, a non-susceptible (drug-resistant) one will come into being, even if you never go anywhere near a medicine bottle. “Bugs aren’t stupid, despite the fact that they don’t have brains,” Heffernan says. “There’s always genetic diversity in a population.”
The mutants aren’t necessarily superior; for example, they may not synthesize certain proteins as well as do standard TB bacilli. Evolution, after all, has refined the standard bugs for millions of years, Heffernan says. But when humans add an antibiotic to the picture, everything changes. The relatively weaker mutants suddenly have a big advantage (their drug resistance) and “they become the survivors.”
Medical researchers became aware of TB’s capacity for outflanking drugs almost immediately after the discovery of streptomycin. One early study found that patients treated with it improved for about four weeks (as the drug-susceptible bugs faltered), then began to languish again (as the streptomycin-resistant subpopulation continued to grow and thrive). Scientists quickly delivered a counter-punch: giving the TB sufferers two different kinds of drugs, such as INH (invented in 1952) plus PAS or streptomycin. Heffernan elaborates, “If it takes 10 to the 6th (one million) bugs to get one that’s INH-resistant, and it takes 10 to the 6th to get one that’s streptomycin-resistant, you’re going to need 10 to the 12th bugs — or a trillion — before you find one that’s resistant to both drugs.” Since most TB victims don’t have that many TB germs inside them, the multiple drug therapy has worked very well. Modified over the years (as additional drugs came along), the standard therapy today involves giving up to four drugs that must be taken for about six months.
The catch is that if a patient fails to take all the drugs for the period of time necessary to kill all the bugs, he may actually set up conditions for one of the mutant strains to predominate, for instance, the strain that’s impervious to INH. If this patient coughs out those INH-resistant germs, and somebody else breathes them in, they’ll come down with INH-resistant TB. When that happens often enough “you begin to have areas of the world, or subpopulations in the U.S., where you have a reservoir of people who have resistant TB,” says Heffernan, adding that this is now the case in both the Philippines and New York City.
Only one more step is necessary for a multi-drug-resistant strain of TB to emerge: not getting the right medicines or not taking them for long enough. If someone has TB that’s resistant to the two best anti-tubercular drugs, INH and rifampin, he has a 50 percent or lower chance of cure, even aided by all the remaining drugs, states Heffernan. His colleague Catanzaro echoes, “We have had about 12 to 15 drugs that we’ve been able to use against tuberculosis, and we’ve known for some time that 2 or 3 are enough. So we figured we had lots of cushion. But when we start finding cases that are resistant to INH, resistant to rifampin, all of a sudden we’re realizing, yeah, we’ve got another 13 or so, but they’re very weak! I mean, they’re so weak it’s pathetic! When you lose INH and rifampin, you are in deep yogurt!”
San Diego isn’t yet in that plight. Though the number of INH- and rifampin-resistant cases has been climbing, last year’s eight cases are hardly cause for panic. Heffernan offers the further reassurance that drug-resistant TB is somewhat harder to catch than regular TB — which in itself is not extraordinarily infectious. “It’s not like chicken pox or measles or pneumonic plague,” the doctor comments. Despite its history of carnage, Mycobacterium tuberculosis humanis has to overcome some formidable hurdles before it can take up residence in someone’s alveolus. It has to get past the person’s defense system against airborne invaders — all the hairs and mucus and cilia lining the nose, trachea, and bronchi. It’s almost always harmless if swallowed. Although it can float in the air for weeks, if it floats into direct sunshine, it will die within seconds (destroyed by the ultraviolet rays). Outdoors there’s so much air relative to the size of the bugs that they’re almost impossible to catch. But even indoors it takes an average of 400 hours of exposure before household members of TB victims get infected, studies have shown.
That doesn’t mean it isn’t important to try to limit TB’s spread, particularly in light of its increasing incidence, which most observers attribute to the rise of social problems such as homelessness, AIDS, and uncontrolled immigration. For the past year, Heffernan has been focusing on the UCSP Medical Center, where 50 TB patients were hospitalized in 1992. Hospitals, of course, are particularly vulnerable places — they harbor people who are actively infectious (some diagnosed, others not). Medical workers do procedures that bring them into much closer contact with the germs than the average household member. Catanzaro, for example, tells of a case at UCSD where the medical staff threaded a lighted tube into the lungs of a pneumonia patient to try to identify what type of pneumonia the person had (this procedure is known as a bronchoscopy). Only later did it become clear that the patient had TB, and testing revealed that 16 people had become infected during the exam, among them “the intern, the resident, the attending [physician], the fellow, several nurses, the respiratory tech, even the poor secretary sitting by the door!” says Catanzaro. “From that one bronchoscopy!”
UCSD’s hospital doesn’t have the additional problem that many facilities acquired in the energy-crisis days of the ’70s, namely, closed ventilation systems that recirculate their air. At the UCSD Medical Center, air flows from each patient room directly to the roof, with fresh air drawn in constantly. But the UCSD facility was unable to build any rooms specially designed to have negative air pressure, which keeps the microorganisms from flowing out into the corridor. For a long time, “when no one was worried anymore about TB,” in Heffernan’s words, state regulators wouldn't allow such rooms in hospitals because of their impact on Fire safety. The rules changed recently, but now it would cost USCD hundreds of thousands of dollars to tear out and replace the duct work necessary to create the invisible germ barriers.
Heffernan says he and the hospital’s environmental safety officer finally got the idea of testing the private rooms to sec if any of them accidentally had negative pressure. They found eight that are persistently negative, “So that’s where we’ve been putting our TB or suspect-TB patients. It’s an ad hoc solution.” And Heffernan has been investigating other cheap and easy ways to lessen the chances of the disease spreading, such as installing portable air filters in both the hospital’s in-patient rooms and its AIDS clinic. But Heffernan offers the opinion that “the heart of TB control is not all the stuff the regulatory agencies are talking about, all the reengineering...in the hospital.” He says, “The way to control this epidemic is to put our increasingly finite resources at the front end: having outreach programs, supporting public health....”
Cheryl Dalton toils in those trenches. Whenever any doctor anywhere in San Diego County diagnoses or even suspects a case of TB, he or she must report it to the county health department. The health department then uses its corps of public health nurses to try to insure that everyone who has TB gets cured of it, so they won’t make more people sick. The county’s 50 public health nurses thus play a role that’s part cop, part nagging mother, part UN diplomat, part guardian angel. In the South Bay Health Center, Dalton and six other full- and part-time public health nurses fill those roles, and as the “TB specialist,” it is Dalton who makes the first visit to the home of every single person diagnosed with TB in the South Bay, from Southeast San Diego to the Mexican border.
On the afternoon I met with her, she said she had wanted to take me to the home of a newly diagnosed patient so I could observe the teaching necessary on the first visit. “But there’s such a privacy about this disease that I couldn’t find [one] who would allow a reporter in,” she said. “In fact, many of the patients that I’ve worked with for a long time wouldn’t [open up to an outsider] because of the stigma.” Three had agreed, and we would be visiting them.
According to Dalton, the Chula Vista clinic normally follows about 140 TB patients. Many are poor and non-white, though they can come from anywhere on the socioeconomic spectrum. Dalton recently attended to one upper-middle-class high school teacher from Bonita, for example. At the other extreme, the public health nurses sometimes visit people living in their cars. “We’ve had nurses who’ve had active cases in crack houses. You drive around the house a couple of times to make sure there’s not a drug deal going down at that moment. You go to the door, and the hand comes out to get the medicine!”
At 38, Dalton has been a nurse for 15 years, with the last 5 spent in public health. “And I love this work,” she says. “I have a passion for it. Because we’re dealing with the whole family. We’re not just treating a disease.... Maybe there’s no food in the house. We know how to get food. We know how to get diapers for the baby. Satisfy some of those basic needs, and then you can do health care.”
The public health nurses visit each TB patient at least three times. After the initial diagnosis is made, Dalton goes out and administers skin tests to everyone else living in the household, and sometimes to co-workers or schoolmates of the sick person. If those tests show that others have been infected, they also may have to take medicine to protect them from getting active TB. About a month later, a public health nurse returns to assess whether the TB patient is “compliant” — that is, taking his or her medicine. If nothing looks suspicious, the nurse will return only once every three or four months until the treatment ends.
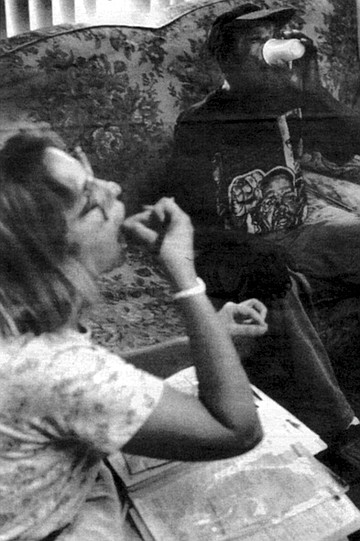
But many people need closer supervision. Dalton tells the story of one alcoholic with advanced tuberculosis. Dalton suspected he might have trouble taking his pills on his own and decided to monitor him weekly. She took him a seven-compartment pill case with each day clearly marked. “I filled it up for him every week, and I said to myself, 'I’m doing such a good job!’ ” And then one day, “one of the other little old drunks in the house took me aside one time when [the patient] wasn’t there and told me he wasn’t taking his pills.” The informant advised Dalton to check inside the household’s oatmeal box. “So I go in the big, roach-infested kitchen. I open the cupboards and I peek into the oatmeal box, and there’s, like, 200 pills! Every week he would dump them all in!” At the memory, Dalton laughs uproariously.
Dalton placed that patient on “directly observed therapy” or DOT, in the jargon of the TB healers. The nurse actually watches such patients put the pills in their mouths; she watches them swallow. “Some patients will try to tongue the pills.” Patients are supposed to be on their honor over the weekends — but the nurses don’t count toward the completion of the therapy any pills that they haven’t actually witnessed being consumed. Dalton says that at any time the Chula Vista office usually has from 23 to 26 DOT patients. On the afternoon that I accompanied her, we visited one named Willie Lee Smith.
Smith lives in a surprisingly rural patch of Southeast San Diego; you reach his home by driving down an unpaved lane next to an open field. That day, heavy fruit hung from robust tomato plants in his front yard. Dalton greeted a few of Smith’s housemates as if they were old friends, then proceeded into the bungalow. Out of the dim interior emerged the figure of her patient, an emaciated black man wearing a baseball cap and a Malcolm X T-shirt. He looked 60, but when I asked his age he replied, “I’m 42.”
“Willie was real sick with TB,” Dalton said, sympathetically. “He had to go to the hospital.”
“I was feelin’ real tired and, well, I couldn’t eat nothin’. I was just feelin’ bad and losing weight all at the same time. I thought it might be comin’ from smokin’, and so I slacked off from smoking.”
“Which is very common,” Dalton interjected. “They’ll treat themselves. They’ll take cough medicine. They’ll stop smoking. They’ll do all these measures before they go to a doctor.”
When Smith began coughing up blood, he finally sought medical help. He was astonished to hear he had TB. He says he has no idea where he might have contracted the disease. “You can’t really tell who gave who because, see, germs, they spread.”
After about a month in the UCSD Medical Center, during which his weight fell to a skeletal 112, Smith finally improved enough to be discharged, but the pills caused several side effects, and “I forgot to take the medicine,” he told me. Under Dalton’s watchful eye since May, Smith would be completing his treatment in a month or two. He gulped his nine large pills in one swallow.
“I’ve got some people on 20 pills a day,” Dalton commented as we sped south again on I-5. Side effects are common. “They make you feel nauseated. A lot of people vomit. They make you feel tired. They make you feel headachy. They make you itch like crazy.” Dalton says the second- and third-line drugs taken by victims of drug-resistant TB are even worse. “Patients can lose their hearing. Or I have one guy who’s on this medication that turns your skin black/purple. He looks like the night!” Other patients “just look at their medicine and they vomit. And they’ve got to take them for so long!” (about two years, compared to the six-month regime for non-drug-resistant TB). “Can you imagine vomiting every day for two years?” Dalton asked.
Such side effects explain why some people don’t finish taking the medicine. Other people wrestle with denial. Dalton says, “TB has such a cultural stigma to it! We have Filipinos, Somalians, many Indochinese. There’s Laotian, Cambodian — you name it, we see it. And in their culture, if they get TB, they’re removed from the home.” Dalton recalls one case involving a young Mexican woman who was diagnosed in Mexico as having TB of the kidneys. “Her family from Mexico was so freaked by the TB diagnosis that they came up and took her child away from her! They told her to sterilize all her dishes and everything.” When Dalton visited her in a tiny trailer in San Ysidro, she had sprayed every surface with Lysol. “I could hardly breathe! She said her family told her to do this. I said, ‘Well, you know, if you took your urine and spritzed it all over the house, it might spread the disease. But it’s not infectious.’ ” In fact, tests here never did grow disease from the girl’s urine samples. “But her family took her baby away for four months!” Dalton says.
Faced with such reprisals, “People say, ‘I don’t have TB. Not me! I have pneumonia.’ Or they won’t take their medicine because they don’t believe they have TB. Or they’ll kind of take it and they kind of won’t.”
Dalton’s second appointment that afternoon took her to Sandi’s Rental Stables on Hollister Road, not far from the border. Her patient here was Jose, a 27-year-old Mexican who shoes horses for a living. He had a strain of TB resistant to both INH and ethambutol, another first-line drug. To combat the disease, he was taking seven pills a day and getting a daily injection of streptomycin, administered by Dalton. At her arrival, lose materialized, looking shy but cordial. He wore jeans but no shirt, showing off a lean but muscled torso that hardly looked ravaged by disease. “I was coughing up a lot of green stuff,” he recalled. When he visited his family in Mexico City, Jose’s mother heard him coughing at night. “My mom know. My mom told me first about tuberculosis. But I never believe it,” he said. When he returned to San Diego, he sought a skin test at the health department, which confirmed his mother’s diagnosis.
Dalton called José into the privacy of the stables office, where she injected an ampule of thick yellow streptomycin into his buttocks. “It hurts a lot. It really burns,” she said later. But the painful treatment appeared to be working. Although Jose had been prohibited by the county from working for two or three months, tests of his sputum had finally shown him to be non-infectious, so he was able to make a living again. “A week ago, he was wearing a mask when I went to see him,” Dalton explained. Not that a mask does much good. “The droplet nuclei go right through a mask,” Dalton said wryly. So what do the nurses do to protect themselves from infection? “You look at your case,” Dalton answered. “If I have a four-plus, smear-positive, real infectious case, I’ll go in and if it’s a really dosed-in place. I’ll stay near the door.” Sometimes she asks patients to open windows, and she reminds them to cough into a tissue. All the nurses get regular skin tests, and finally, “You know, you just kind of say a little prayer when you go in.” She laughed again.
Health officials say most patients welcome the nurses, but every so often someone reacts differently. Says UCSD’s Catanzaro, “I’ll never forget a woman I diagnosed a few years ago as having TB. I sat down and explained what that meant, and she said, ‘You mean I can make somebody sick just by breathing on them?’ And I said yeah, and she said, ‘Cooool!’ She was a working prostitute, and when she left the hospital, even though we made the liaison with the health department, she made an effort not to be found.”
In such cases, county officials can issue an “order of isolation and quarantine,” and if the patient ignores the order he can be sent to jail. Moser of the health department says three or four people per year have been incarcerated (at the Vista Jail, which has respiratory isolation rooms) for that reason, though in many cases judges have ordered them released before their treatment was over. “And every time except once, out of about eight or nine cases, it has failed,” says Moser. “The people just disappear; we never see them again.”
If open hostility to the public health nurses is rare, Dalton says cultural differences create daily pitfalls. “When I go into Indochinese homes, I take off my shoes. I use an interpreter. I understand not to look at the women but to look at the men. You have to learn how to avoid offending them.” She says among the most difficult groups to work with are the Somalian refugees, who have a very high TB rate. “They almost all have to be on supervised therapy, because they don’t take their medicine. They’re a very male-dominant culture,” she says. “This is what happens. I go into the house. The man is very arrogant. ‘You come here. I show you how to cure arthritis.’ And there’s a young woman sitting at his feet, rubbing his leg with Wesson oil. She takes a razor— this is no lie! — and she cuts his leg and puts a cow’s horn on top of the cut to pull out the blood, which relieves the poison in the body to relieve the arthritis. It’s this kind of health practice that we’re dealing with. If they have a headache, they cut their head to bleed it.”
Subtler factors complicated the case of 15-year-old Paola, Dalton’s third and final patient of this afternoon. Paola lives with her family in a tidy, new-looking neighborhood just west of San Ysidro. “I’m sorry the house is such a mess,” she apologized as we arrived. It looked spotless, and it was hard to believe Paola’s lungs were any less immaculate. A sturdy girl with pretty eyes, she wore her thick, glossy hair pulled back with a hair ornament that looked as if it should be decorating a birthday present.
She explained that a routine TB skin test last fall had revealed that she and several family members were infected. The family’s doctor ordered a course of preventive medicine, which Paola took for a while, then abandoned. And why? “Because [the doctor] told me to take it in the morning when I had eaten breakfast, and I don’t eat breakfast, so I kept forgetting to take it,” the teenager explained. “Also I had it in my cabinet in the bathroom, so it wasn’t visible.”
A few months later, her mother saw a television news report about TB and was worried enough by it to take Paola back for a recheck. “I had no symptoms or nothing,” Paola recalls — but this time an X-ray showed the TB germs to be eating away at one of her lungs. Paola then had to begin taking three different types of medication a day, with the public health nurses stopping by every two to four weeks to do “pill counts” to check on her compliance.
“And she’s perfect on her count this time!” Dalton announced, beaming. She thus wouldn’t schedule another visit to Paola’s home for a full month. But she gently ordered the girl to let her know when she had rescheduled a doctor’s visit the girl had skipped because it conflicted with her school exams.
Driving back to the Chula Vista clinic, Dalton mentioned that she had recently toured the county’s TB lab, where much of the identification and testing of the germs takes place. An enthusiastic person, Dalton grew even more animated describing the facility. She urged me to visit it, and so one recent Wednesday I entered the large complex just east of the Midway/Rosecrans intersection.
This building used to be Fedmart’s corporate headquarters; today the TB lab is located down a maze of corridors deep within it. It’s not a huge space, and it’s cluttered with instruments and work benches and cabinets and test tubes and papers. Tightly stoppered vials of sputum arrive three times a week; some of them are teaming with TB bacteria. Every time the microbiologists and lab assistants open a vial or one of the Petri dishes in which they culture the bacteria, they don gloves and lab coats and withdraw into one of two isolation chambers in the innermost recesses of the lab. These chambers are flooded with ultraviolet light when empty. When workers enter, they switch the lights off, but as much as possible, they keep their hands and the TB containers inside a long “biological safety cabinet.” Air inside the cabinet is drawn up into a smaller metal chamber containing a filter that traps particles down to less than a micron, then exhausts the purified air to the outside. If ever any container cracks or breaks, the lab personnel follow a rigid set of decontamination procedures.
Here, in the laboratory, tuberculosis seems most real. It’s alive, growing under the microscope, mushrooming into colonies you can see unaided. It also seems least fearsome; I could understand why Dalton so liked the place. Amidst all the devices for studying them and containing them, the teeny germs (which killed more than three million human beings around the world last year) seem like they shouldn’t have a chance against us.
Comments