 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

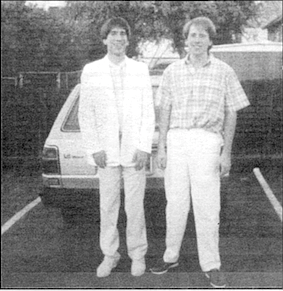
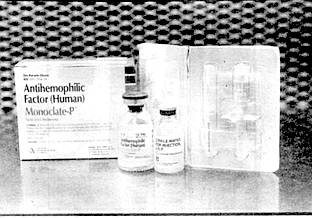
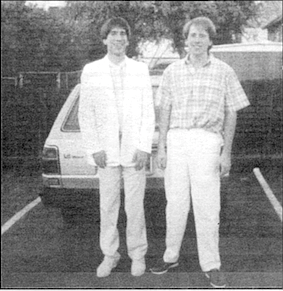
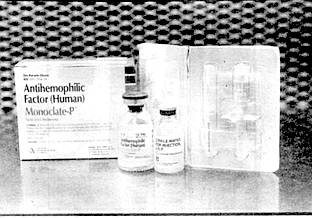
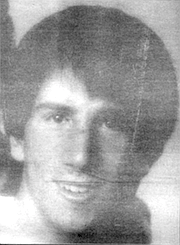
The Son, Rick Valdez: In a lot of ways my brother and I were opposites. Steven was conventional and I was the rebel. He was the good boy, and I always questioned things. We were both severe hemophiliacs, and we’d been going to Children’s Hospital — I can’t even tell you for certain, but since the mid-’60s. When we were young we were always at the hospital because we were bleeding all the time. I had a lot of emergencies, and there was always bleeding into the joints, so we were there to get the blood. First the whole blood, then later the cryoprecipitate, the cryo, and then starting in, like, 1972, the concentrate called Factor VIII that causes our blood to clot normally. It was the Factor VIII that saved us at first, then it killed my brother last June. He was 25 when he died of AIDS. And it will eventually kill me too. I’m 31.
When I was really young, when Factor VIII first came out, at times we were on what they called a prophylactic treatment, which means you would get it regardless of whether you were bleeding or not, as a preventative. You’d get the Factor intravenously every couple of days. It's like brushing your teeth after a while. We learned to do it ourselves at home, and it was a hell of a lot better than having to go to the hospital.

But we weren’t on the prophylactic treatment very long. Eventually we just started treating ourselves when we felt a twinge indicating a bleed. It’s a little hard now to tell when there’s a bleed because of arthritis in my knees and in my ankles. Back in the mid-’80s is when the arthritis got real bad, and it's hard to discriminate now between the arthritic pain and the pain that occurs when there’s a bleed going on.
So once we started using the Factor, we only had to go to the hospital every few months for checkups, and that was a lot better. I started doing my own IVs when I was about 14. And all that time we had the same doctor, Gary Hartman.
I looked at him as someone you could trust. I had complete faith in him. and because of that I partially blame my trust in him for me not being more inquisitive, not asking questions sooner. Because when this AIDS thing hit the newspapers and television in the early 1980s, they were saying, oh, well, it’s affecting gays — and every once in a while there would be a little thing that, hey, it might affect hemophiliacs through the blood products. And I can remember thinking, well, you know, Gary’s not saying anything about it, so I didn’t figure there was anything to go in for.
Then at the end of 1983, Gary called a meeting of his hemophiliac patients. I had no idea what AIDS was and in fact ended up telling another hemophiliac that was there, hey, if Gary wasn’t saying anything about it then I wasn’t going to worry about it. It seemed like the media were changing their description of it and who it was affecting almost daily. If you tried to keep up with that, you would realize it was worthless, because there were no absolutes at all.
So the way this meeting was set up, we didn’t get a phone call or anything. He didn’t call and say, “Hey, this could affect you, it may be in the Factor, better come in and talk with us right now.” What we got was a notice in the mail announcing this meeting a couple of weeks ahead of time. And of course, in the meantime, we’re still giving ourselves the Factor. Gary has no idea how many times we’re doing it. So in my mind this thing was really downplayed.
Steven was at the meeting with his girlfriend Linda. Some of the other hemophiliacs were there with their wives. Gary’s presentation was low key — “Well, here’s my view....” And the gist was, he didn’t know for sure if the Factor was contaminated. The actual test to detect the AIDS virus wasn’t developed until 1985. All he said was, well, if you want, you could try to go back to the cryo, which was the earlier way we were treated and entailed going into the hospital for treatment.
But to me, based on the facts he presented, the chances of us getting this thing [AIDS] were slim to none. The air he had about him, there was no panic. He said there was a heat-treated Factor that would probably take care of any possible contamination, and that was supposed to be available within a couple of months. My brother came away feeling the same way I did. that this was no big deal. It turned out that he died of AIDS, and he gave it to Linda and she died of AIDS last summer on Steven’s birthday, and I’m HIV positive. Basically, almost every severe hemophiliac who was bom before 1985 is either dead or is HIV positive.
I look at it in comparison to the Tylenol poisoning. Remember that? Someone died after taking Tylenol and it was a national alert, and Tylenol was taken off the shelves immediately. But the Factor continued to be sold to us after they suspected it was contaminated. We were poisoned. That’s a crime.
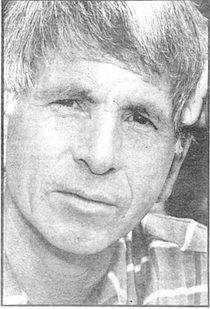
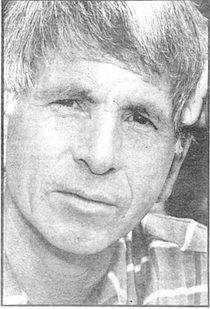
The Doctor, Gary Hartman:
I recall my message at that meeting. Actually, there were two meetings about six months apart. They were very somber, very upsetting. It was a time when it became clearer and clearer that there was big problems, that the Factor was contaminated. It was difficult to know how to react.
First of all, everyone who had been on prophylaxis to prevent bleeding, all that was stopped, which was real hard. Some people didn’t want to stop it. There were kids who felt real normal using Factor three times a week, who could play baseball, and all of a sudden without the Factor they’re hemophiliacs again. I said we can’t do this anymore, because we don’t know which lots [of Factor VIII] are bad. People had their own supplies at home, and they ’re going to do what they’re going to do. all I can do is present material, give recommendations.
We talked about development of AIDS at that meeting. We didn’t call it HIV then, it was HTLV-3. Rick and Steven were at that meeting; and other people there came away with a different perception than they did. One man came away believing that he was already infected with the virus. It was very somber, very draining.
We talked about going back to cryoprecipitate, and I remember at least one patient — and there were probably others — who said that cryo was really bad. it was hard to deal with. “Life was lousy with it, and I’m not going back to that.” And how clean was cryo? It wasn’t made from pooled blood, true, but when you start to use 10 or 20 bags at a time, all of a sudden that’s a form of pooling. There was no test available to determine what was clean and what wasn’t. If Rick was waiting for a signal from me to go back to cryo, well, I wasn’t going to give one, because it didn’t seem like it was a good idea at the time.
The fact is. the die was cast by the time we realized it was a problem. It’s true that the first announcement from the Centers for Disease Control about hemophilia and immune failures was in July 1982. But there was no consensus in the hemophilia community until April of ’83 that this was a blood problem. People were already infected. I think most of them were already infected at that point. We didn’t know for sure, but that was my fear then. I didn't know what to think, but that was my fear.
As you approach something like this, you try to look at the facts, you try to plumb the emotions, and then try to make a recommendation and problem-solve. Thinking back on those times — the problem-solving thing was terrible, it was very difficult. Some people really cope and go through the world by taking information in. as much information as they can, even when it’s tough. And some people have more difficulty with that. It’s just another way. another style of living or coping, to tend to deny and push things out. And the other thing is. Rick was having memory problems at the time. "He had had a brain hemorrhage a couple years before and was having some memory problems.
Did I consider taking my patients off Factor? You know, I just talked to some other people about this. I don’t think any doctor would have taken everybody off of all of their Factor. It would be a really very difficult decision. The bigger centers, L.A. Children’s, L.A. Orthopedic, and San Diego Children’s, we were sort of all very closely aligned. None of us thought we should drop Factor completely. And that was not the recommendation from the National Hemophilia Association. Even if we had all dropped Factor in 1983, it might not have made much difference. You know, once a good HIV test was developed. some lots of Factor were found to be contaminated as early as 1978.
I’ve heard the term “medically induced AIDS" used by some hemophiliacs. Well, what a strange term. Something was prescribed, something which was used, appreciated. and welcomed by the patients, and none of us knew that it was tainted. And it wasn't tainted, initially. May I give you an example of this? In 1982. Richard Valdez had a headache at work, and he went home and told his grandmother that he was going to sleep. And she gave him a Tylenol. Now headaches and sleepiness, put together, are strong evidence of something wrong inside the brain of a hemophiliac. What it indicates is a bleed. You don’t have to have any head injury; it can be spontaneous intracranial bleeding.
Now we found out about this sort of by accident. I think Dick [Rick's father] had called Sallie [Rick’s mother], and Sallie had called Rick's grandmother, where he was living, and said, “Why don’t you go and wake him up?” The grandmother could not wake him up. He was basically dying.
They called us [at Children’s Hospital], they called 911,1 talked with the police over the phone, and I talked with the paramedics. Now what I had to do was get the paramedics to bring him to our facility, which is something that takes, like, a Richter 7 of energy because they are programmed only to go to the nearest hospital. I’m on the phone screaming at them, saying there's no hemophilia care at the nearest hospital, however fine a hospital it is. Get him to where I can do it, which was Sharp’s emergency room, because Children’s didn’t have an emergency room at that time. And they did. This was, like, miraculous. I had 4000 units, lots of vials, of Factor VIII.
Rick was terribly sick. He was basically dying. His heart rate and his breathing rate started to change. We gave him the Factor to try to stop the bleeding in his brain. Finally, an anesthesiologist came down, got him breathing, took him to a CT scanner, found this big intracranial bleed; I had a neurosurgeon there, took him up to the operating room, and I stayed with him. They evacuated a big blood clot that was all the way through into the brain. It was an amazing wad of stuff. The surgeon said, “I still think he’s bleeding.” So I gave him more Factor. This is 1982 Factor. For all I know, this is where the virus came in. There was no question of using Factor — if you’d wanted to use cryo or fresh-frozen plasma, it wouldn’t have worked. You needed such huge volumes.
Even if we knew then that something was wrong with the Factor — which we didn’t — what would you say? Let him die? Let his head bleed? Of course not. But this is 1982, and in retrospect the Factor was contaminated. So if he got the virus then, that was medically induced, okay? I don't know; I think people are expecting, looking through 1992 eyes, to make the world different from the way it was. We did the damnedest best we could.
I have not felt guilty about it. I have felt thoughtful, somber, unhappy; there are a lot of different feelings I have. But as far as guilt, no. Responsibility? Well, yes. We share the responsibility for taking Factor. Yeah, we did it together, we did it as a team, and we share responsibility, my patients and I. In my heart of hearts, I know I did not give them AIDS, and I could not have prevented it.
The Mother, Sallie Bankston:
I have to tell you one thing about Dr. Hartman. I had always felt that he was a very special doctor. I looked up to him. He always seemed very sensitive to the needs of the guys and even of the family. And it was just a shock to me when all of a sudden he calls a meeting and they’re going to explain things to the guys. That, of course, is when they tell us [about AIDS] for the first time.
And didn't really make a big deal out of it.
I was not at the meeting, but the boys came home and said there was something going on about the blood, you know, the Factor that they got. And that’s the first time I knew that the Factor VIII they used was bought off the street, so to speak.
They said not every thing was in yet, but it was looking like the blood may be contaminated. And at that time I instantly called and tried to get some answers. I called the hematology nurse at Children’s, Bettie Spangler, and she said, “Don’t worry about it yet, Sallie, because we’re still just getting in the information on it.” But I told her, no, that's not the way it’s going to be. 1 was going to start looking into what it was all about. So I decided where to go to look would be the San Diego Blood Bank. I thought maybe the blood bank would be able to bail us out. 1 had the hope that maybe the boys hadn’t been exposed yet.
The blood bank could make fresh Factor VIII, but they only did that for small children. There was a shock period I went through when I got so knocked down by the blood bank saying there was no way they could supply us with fresh Factor VIII. They didn’t have enough blood, it was impossible. I tried to fight them, but the administrator stood firm.
It wasn’t until much later that I found out that everyone involved was making big bucks off the Factor, including Children’s Hospital. It came out accidentally. It was said to another parent, after we were all dumped over to University Hospital. that, boy, we really miss having that Factor VIII in our budget because we were really making money off of it. And I said, "What do you mean?" I hadn't even thought about anyone making a big profit on it.
Children’s asking us to leave and go over to University Hospital was like a nightmare that I'll never forget. This is the summer of 1987. Steven was already diagnosed as having, being in the illness. Children's was looking at what AIDS was. and it was really too much for them to handle. We were dumped, after being with Children’s for more than 20 years. Every adult hemophiliac got dumped when a few of them started getting sick. At first they said, now, we'll give you a year, it’ll take about a year to get you transferred over there. Well, it took them maybe a month. They wanted us out of there. We had no idea what was going on. It happened so quick, and we just didn’t know what was happening.
I did not know the boys had been tested for HIV. They never told them and they never told us, the family. It was all done underhanded, and the only reason it was found out was because a friend, another person with hemophilia, saw the results of an AIDS test in his records, saw everybody’s name, and Rick’s name was negative. And he got so excited for Rick. At least Rick was negative, you know. This was 1987, but the test had been done two years earlier. In 1987 we were still in the dark, but we knew by then that something was really bad about this AIDS thing. Of course, later Rick asked to be tested and he came up positive.
Dr. Hartman never did say to me that the Factor was contaminated and Steven had AIDS. He only told me that Steven was very ill. He did confront me with that. He went into the particular parts of the body, that his liver, that his body was not making platelets, but he didn't make a personal thing of calling it AIDS. Every word that came out of his mouth was very measured, because he supposedly didn’t know what was going on either. Now I feel that this was all untrue. I feel he knew a year before he moved us to UCSD, and we were all kept quiet by not being told. The topper was, when Steve got sick, we all got dumped.
Dr. Hartman called a big meeting of all the hemophiliac families to tell us that this was the end, we were all going over to UCSD. and I want to tell you, our hearts all fell. What was going to go on for those next few months was a nightmare. If you’ve gone to the same doctor for 20 years and all of a sudden you're tossed to this place that you cannot believe — UCSD is just a maze of people. 1 guess we'd been spoiled. Dr. Hartman said they were being moved because they were adults — he didn't say anything about AIDS — and they needed to be with doctors that treated adults, and that was his big way of getting us to move without any trouble. But many of his patients had been adults for several years; Rick was 26 then.
I was so devastated. I just slid into the position of. What do we do now? And that was to go to the doctors most of the time. And go from one emergency to the next emergency. And knowing that I was losing my son. I’ve lost the fight, you know. I was having to fight at UCSD just to get decent care, because they didn’t have a lot of hemophiliacs then or know how to treat them, so we got into a lot of care problems. Many limes an intern would come along, see us in the emergency room, and they just didn’t know what they were supposed to know. I understand they’re getting better now. Steven was the one who trained them, and you know, it was a sad way to go. Leaving Children’s was like leaving the Marriott and going to a low-budget motel.
When you sit for a couple of hours in a room full of AIDS patients that are so sick, can you imagine how that makes you feel? Rick was still well, and he’d have to go and see that. I know with Steve it just really got to him.
Last spring, right before Steven passed away, he went into UCSD and they needed to give him something intravenously. Anybody that knows hemophiliacs in the medical field knows that you really have to tourniquet anything where there’s been something bleeding. And so the woman gouged and pushed and pulled and she couldn’t find a vein, so she just gave up on that arm and went on to the other arm. When I got there his arm was swollen up like a balloon, and it was turning purple and black. I asked to see the doctor that oversees the whole thing, and he said to me, well, Steven’s a hemophiliac, those things can happen. I said, "Don’t give me that stuff, it’s not true. This does not need to happen. We’re in a new age now. Where are you from?”
Steven suffered over that arm until he died, about three weeks later. His whole arm was filled up with blood, right into the fingers.
You know. I’ve thought about all this, and I think Dr. Hartman could have handled that initial meeting better. I don’t think he really gave the boys a choice. Everyone should have been given the choice of being more crippled or even losing their life, gambling, rather than go on using this Factor that is tainted. If you're working in the medical field, you'd have to have known that thing was going on with the blood supply way before they told us.
Linda. Steve’s fiancee, was at that meeting. When I asked what happened at the meeting, she said it was no big deal, no emergency-type thing. If I was Dr. Hartman or the nurse. Bettie Spangler, and I’d seen little Linda sitting there — she wasn’t a hemophiliac — how could they let them walk out of the room? When there’s an emergency, you don't just say. well, by the way, there’s an emergency. It seems like it was just kind of pushed under the carpet.
Rick:
Bettie Spangler, this woman who had been our nurse for so many years, came to my brother’s memorial after he died. I wasn’t sure I wanted to talk to her. And she has the nerve to say that when we went to the other hospital, they lost a lot of money in Factor sales. She said that to me! I couldn't believe it. And that’s the whole point of this whole thing.
Most hemophiliacs don’t have private insurance; we’re covered by the State of California.
At some point in the 1970s, a law was passed that created the Genetically Handicapped Persons Program, and that covered hemophiliacs once we reached 21. Prior to that we were covered by the Crippled Children’s Society. So all of our Factor was purchased through the hospital, and the hospital was reimbursed at a profit. And then when the heat-treated Factor came in in 1983, the cost of it doubled. Now it costs about $1000 for one treatment, and some hemophiliacs need several treatments a week.
Sometime in 1985 these brokerage companies started coming to sell us the Factor. That year this broker came to San Diego and was basically trying to infiltrate the hemophilia population here locally so he could sell his product. He was a hemophiliac too. He came to me and asked if I wanted to start utilizing his services. And I can’t believe I said this, but I did. "Well, let me talk to Dr. Hartman, because they have taken care of us so well, I want to see what he says." In 1985 I still didn’t know what was really going on. The idea was I would get half my Factor from this brokerage firm and half of it from Children’s.
So I asked Bettie Spangler, because I guess when I thought of it she was there, and she went, “You’re supposed to talk to Gary.” But she talked with him and came back to me later and said, "Well, we’d rather not have you do that because this is how we keep our clinic open is by selling this stuff.”
And when my dad and I confronted Gary last summer after my brother had died, he — I don’t know what kind of case he was trying to build in his favor — but he said he went to the administrators of the hospital and tried to advocate for us to keep us at Children’s, because the amount of Factor they were selling to us was actually helping pay for other areas in the hospital, not only our clinic. And this is what Gary himself said.
My whole point is that Children's Hospital was making big money selling this stuff to us. And Gary Hartman tells us that he went to the administrators who wanted us out of there because they knew what was coming, they wanted us out of there, but he supposedly went on our behalf to say keep these guys here — there were about ten adult hemophiliacs — keep them here because we make such a good profit on selling them the Factor that they help support some of the other clinics in the hospital. They hung on to us as long as they could so they could continue to make the money off of us.
My brother could have gone over to UCSD sooner. Maybe he'd still be alive today if he had gone earlier to where they were treating AIDS patients as a specialty. I don’t know if that would have helped, but it might have. They definitely knew most of us were HIV positive at least a year, maybe two years before they dumped us. I can’t tell you exactly when they knew it, but I was tested without asking to be tested and without my knowledge.
When I found out about it was 1987, but I think the test was done in 1985. Another hemophiliac patient at Children’s Hospital found this list of all the hemophiliacs at that treatment center. It was in his medical file. Each of us had been tested for the AIDS virus. They leave your records out for your doctor to look at, and this guy always looked through his and he found this list. I was the only one on the list who tested negative. I was never informed of it. I went to Gary then and asked to be tested, and my test came back positive. This was right before they moved us to UCSD.
So I went into my own denial. I mean, this is insane. You gotta remember it’s died down, as far as the publicity that AIDS gets now and depictions of people dying in the hospitals. You don’t see that anymore. But back then you did. And it’s like, no way do you think you have this. And so I kind of for a while let it ride at that. Okay, one test was negative and one test was positive, so as far as I was concerned, you know, that didn’t tell me anything, okay? And so I went along for a while, until sometime in ’88, before I asked to be tested again. Of course, it was positive. And in the meantime my brother got sick.
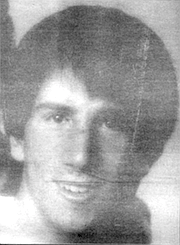
He had moved back in with my mom in ’86, and sometime later on he and his girlfriend Linda got another apartment and lived together again for just a few months. And then she started going out with a friend of my brother’s, and my brother got sick then and never got well. He moved back in with my mom then. My mother chased Linda down after she and my brother were broken up and said, “Hey, you gotta get tested." That was my mother’s project, to go and get the girl tested, because Linda didn’t really care. Turned out she was positive too.
To say it was hard on my mother to nurse Steven and watch him die is an understatement. She still hasn’t recovered, and I don’t know that she will. When I start getting sick, I don’t know what’s going to happen, where I’m going to go, because I can’t stay with my grandmother. She couldn’t handle it. And I wouldn’t want my mother to go through it again. My parents divorced when I was about eight, in the late ’60s, and they’re both remarried. Moving in with my dad isn't an option.
I didn’t see my brother too often, only really at the end, the last eight months of his life, and it was pretty bad. He was in and out of the hospital. and I visited him.and ran into him two times in the emergency room. Toward the end of 1990, he was at the hospital every day. and on two separate occasions I was there for something and I felt. well. I’m going to go by the emergency room, which is usually where you have to go to get any care at UCSD. On both these occasions my brother was there, and it was insane what I saw.
The main thing I remember was he had this thing called a neuropathy; I can’t even tell you exactly what it is. It’s a type of nerve damage affecting the central nervous system. He was in agony. The way he described it to me was. these nerv e impulses were moving through his body and they were doing something so outrageous to his system he could see his skin moving. That’s how he described it. and it was agony. He was on a gurney, and I tried to step away to see if I could get him some relief, and the nurse’s attitude over there was, well, we don’t want to give him any pain medication because it will cover up the symptoms. And as I stepped away Steven started bawling. He just didn’t want me to go away because he was so afraid. He didn’t know what was going to happen, and they wouldn’t give him any medicine. You know, he’d had this thing for quite some time, so they knew it was neuropathy. I don’t know what the hell their problem was.
You know, these are the kinds of things I have to look forward to. I already witnessed my future when I saw what my brother was going through. They put you in a room with at least two other guys that arc dying of AIDS, and they’re in different stages. I mean, it’s just a horror to see these guys, some of them are skeletons and they’re tied to different machines. It’s just a nightmare.
I’m fucked. There’s no other way to say it. I don’t have an alternative. I have no insurance. I’ll never get insurance. I'm a ward of the state. And what the state is, you go to UCSD and whatever you can get over there, that’s what you get.
I haven’t really thought about suicide because I don’t want to die. Gimme drugs, gimme morphine. My brother did it. and — I can say to you right now I haven’t sat down and said, okay, once it gets to the point where I can’t deal with it. I’m going to kill myself. No. Whereas I talked to this other person who was gay who had AIDS, and he told me that if it gets to a real bad point, he’d already been through hell, he had a w ay planned and was going to do it with pills — downers. But he never did it, because it killed him.
Dr. Hartman:
In 1985. just prior to the development of a reliable test for the AIDS virus, someone from a laboratory called me and said, “I have an investigational test kit for HTLV-3. I would like some specimen to test. What would you think?" And I said okay.
We sent him blood samples, and he tested them and he sent the results back in an informal way. and we put it in each person’s chart just as it came in. For better or for worse, that’s how we did it. Richard came back negative on that test. I don’t remember if all of my 20 or so patients were tested, but several were.
On that test also was another young man who had a different illness, who’d had a lot of transfusions. He was clearly dying of AIDS, and his test was negative. Okay. In fact, we sent two of his samples to be tested, and they were both negative. I knew that the guy had AIDS. He was wasting away.
So here I was with a test which was unproven, and I knew that it had certain weaknesses, like it had missed this guy. This is early 1985. and the real AIDS test was to come out in the middle of that year. I didn’t know that the real test was so close. So what would you do for someone who had hemophilia who had a negative HIV test? What would you do? Put him on the best product available, for one thing, to protect that person. And if he’s negative, the best product available for a hemophiliac is clean Factor. He’d been on heat-treated Factor for over a year. And that’s what we did for the ones who tested positive too. I was afraid of that test. I didn't trust it. So why did we do it and why was it around? If I remember right, it was a desperation kind of thing. It was investigational, but it had clinical implications. And the real testing came out soon after. But there was a big rigamarole about that. It was very difficult to get testing.
I didn’t inform the patients who’d been tested because I knew it was an inaccurate test. Did I start testing my patients when the real test eamc out ? You know. I think so but I can’t remember. And when I review the charts I can’t find anything. Once people started realizing the implications. there were no results of AIDS testing allowed in medical records. Not even the order that you’d been doing AIDS testing. You could get thrown in jail even for telling another person that a patient had been tested. From a medical standpoint, this was very awkward. So testing results were kept separately in a division of medical records under lock and key. And I recently went up and looked, and there was nothing there. I don’t know. It was a very awkward time.
A lot of people didn’t want to know and didn’t want to be tested. That’s one thing. A lot of spouses didn’t want to be tested either for years afterward and probably still don’t. You know, there’s a blank. I don’t remember if we tested everybody. There were a lot of things going on, a lot of very busy and important things. I had a talk with a hemophilia nurse at the time, and her recollection was, yes. that we had done the testing.
I'm sure we sat down with patients and talked about having positive tests. I remember it. I would hope and think it was a matter of policy but. you know. I don’t recall if we talked to everybody. Rick says he was never told? Okay, on the other hand, maybe it was sort of almost a given that everyone was positive.
Then shouldn’t they have been given the best AIDS treatment available at that time? Well, what was the AIDS treatment? What was it? AZT was being worked on. but only w ith very sick patients, not hemophiliacs and not children. Very sick gay men who were basically dying. I remember that these people started doing better. But AZT is a very toxic drug. You don’t take this for a cold, okay? You could really do a lot of harm with this drug. They tried it on people who were a little less sick, and lo and behold, these people did much better too. Okay. Amen. Eventually it was tested on gay men who were HIV positive but asymptomatic. Then the study came down to hemophiliacs.
But in 1987, no one was giving AZT to asymptomatic people. It would have been crazy. It was not indicated. So the point is, there was no best treatment for positive hemophiliacs. There was nothing else being done. It was really important for me to get the best that was available, and that’s why I started sending them over to UCSD when it became clear that that clinic could be more helpful.
Now I want to make it real clear that it was the adults, whether or not they were HIV positive. who were sent to University Hospital. True, basically all of them were positive. But the children. the hemophiliacs who were not yet 18, stayed at Children’s, whether or not they were HIV positive. I did not send HIV people away, okay? I sent adults away.
“Dumped” certainly is a charged word, isn’t it? I want to clear that up now. When they started getting sick — first of all. let me tell you about another patient. I won’t identify him. He called me one day to say he’s got the chicken pox. Now chicken pox in you or me or a normal kid is not bad. But chicken pox when you’re immune-suppressed can be devastating. It’s a really powerful virus if you don’t have an immune system that works. I said, “Come over to the hospital. I’ll meet you outside, in the parking lot.” We don’t even let chicken pox patients inside the door. I looked at him, I said. "I want you to get in the car, go right to UCSD. I’m going to call and tell them you’re coming." And I did. Where was I going to put him? Anybody over the age of 18 can’t be hospitalized at Children’s.
He got to UCSD. he was admitted, he was looked at. Twelve hours later he was on a ventilator, very sick. He was pulled through by their critical care, their pulmonary doctors, and a whole team with a lot of expertise. I was really impressed. That was very reinforcing to me. I had no place to hospitalize and take care of him. though Children's was wonderful. It’s terrific, but there’s nobody over the age of 18. and even 16 to 18 is borderline. So when one person got sick, I started to realize I had no place to put these people. And I had enjoyed this wonderful relationship with them since 1971; we grew up together in many ways, we went through a lot of things together.
In certain kinds of childhood illnesses, such as cystic fibrosis and muscular dystrophy, kids generally move out of children’s hospitals when they’re 18. But that isn’t generally true of hemophiliacs, where internists aren’t that familiar with the principles of treatment. Plus, with hemophiliacs you establish this primary, close relationship. It’s like family, so you hang on. And it was fun. I would see them all every 6 to 12 months and go over their hemophilia stuff and try to coordinate their care.
But eventually I ended up taking care of adults. It was okay when they weren’t getting sick and there was no treatment for HIV; I might as well do it. I mean. I knew them. A lot of them came in and talked because they were worried about HIV. There was a lot of that. But I realized that the decision was whether to continue this wonderful relationship or to get the best medical care, and I didn’t have it. It was an agonizing, soul-searching. very difficult decision made on medical principles only. But I know it felt like abandonment to them.
And now I’m being faulted for transferring them to University, and I’m being faulted for not transferring them earlier. It’s difficult to respond to the criticism, but I’m going to go down swinging.
It was my decision to transfer the adult patients. I went to the medical director and I said. I want you to know what I'm doing because. I mean, this is, like, big stuff. I think it’s for the best. Did the cost of losing the Factor ever come up? Never. Money for the hospital had nothing to do with my hanging on to the patients until 1987. I know how that question came up It was when the entrepreneurial brokers started moving in. and I asked someone, a patient. Would you keep buying your Factor from us? Would you consider it?
The brokers were actually giving very good service, which we weren’t doing, and the big hospitals sort of had to adjust to this. It was a new world. But the brokers had a bad rep. They had a rep that they were giving medical advice, and that didn’t go down well with the hemophilia centers. It was an issue of medical control The money was secondary. The thing I was concerned about was medical control.
Most of the patients were on MediC al, or GHPP. and some were on private insurance What is the reimbursement for Factor? It was about cost plus two percent. That’s it. So there was a profit there, and there was more profit from people with private insurance, okay. It was not a gold mine, but there was profit. You have to look at the net versus the gross cost, and sometimes the pharmacies look at that and sometimes the hospital administrators do. and I know this is an issue. But you have to look at how we treated them medically too.
There was me. there was an orthopedic surgeon who saw patients, who I don’t think even charged except if he did operations, which was a few. There was a specialized hemophilia nurse who was paid by the hospital. There was a social worker who was paid by the hospital. The routine clinic visits were about every six months; everybody sees the patient, it takes a long time. And what was the payment — $50. $75? Not a money-making thing. That's not why you go into hemophilia care. And there were times when administrators looked at it and said. look, you have 25 patients, we have limited resources. People arc ratcheting down the amount of money that goes to hospitals, why not cut your social worker? And they did. They cut our social worker, and that hurt people. The Factor sales brought some money in, and it gave me some clout, gave me some sort of validity with administration at a time when they were thinking money, bottom line. That clout helped the patients. And I want to make it super clear that this has nothing to do with personal money to me.
I’m 50, and I’ve recently retired. I have been in pediatric hematology and oncology for about 20 years, and I had a lot of rewards. It’s been really good to me. And I think I'm really good at it. But it begins to take its toll after a while, and I decided that I had to make a change. I said goodbye to an awful lot of people, and I've been to enough funerals.
The Father, Dick Valdez:
When I found out Children's Hospital was having a telethon last summer, I said. “Let's picket the thing.” Steve had only been dead about two weeks. Rick, and myself, and my mother, Rick’s grandmother, were out there, and later another hemophiliac joined us. People who worked at the hospital were giving us the bird, and the volunteers coming in didn't know what to think. I stayed on the sidewalk easement. I wasn’t about to get on their property. One of the security guys who was in a suit came out and tried to bait me onto the property. I said, “If you want to know why I’m here and what I’m concerned about, come down and read." We had Steven’s obituary, and we had all the basic facts laid out.
He wouldn’t come down, but he went and got another suit-type guy. I guess one of the vice presidents. Children’s has got a lot of vice presidents — and eventually, the next day actually, a guy was sent out who was a human relations type, and he was a total mediator. He asked. “What does this have to do with us?” I said, “Well, because you took care of my son for 20 years. The only reason he went to University Hospital was because he was HIV positive, and your doctor said you people couldn't handle it.” At that point I didn’t know that Hartman knew Steve was positive for a year before he transferred him. Then he said. “Well, what are you saying?” I answered, “He was in your care when he got infected, which nobody has ever survived. So as far as I’m concerned, Children’s Hospital killed my son. plain and simple. Your doctor killed my son."
He asked what I wanted, and I told him I wanted to sit down face to face with Dr. Hartman and find out exactly what happened. “Well, he’s in the midst of retiring.” Yeah, isn't that convenient? Eventually we were given a meeting with another doctor who is part of the administration, and of course, his defense was, “We didn’t know.” That’s how they all do it. That’s how the pharmaceutical people do it. that’s how the blood bank does it, the medical community in total. That’s their whole defense. But I don’t accept that at all. There’s too many facts, too many things that have come up in trials. There’s trials all over the country involving hemophiliacs. Some have been settled out of court, with no details announced as part of the settlement. That’s the typical settlement, in fact. Others are still pending.
So this doctor told us we were entitled to know what happened, and he set us up a meeting with Dr. Hartman. But he made us understand that Hartman was not an employee of the hospital, he was an independent contractor. We met in late July, the five of us — Dr. Hartman, Bettie Spangler, the nurse, this other doctor who set up the meeting, and Rick and myself. It started badly. I mean. Dr. Hartman was trying to be very friendly, and we immediately let him know that we weren’t there to be friendly.
The first thing I said was. “Tell me what happened. Why did my son die?" And of course, he went into the medical explanation. I said. “No. I don’t want the medical explanation. Why with all the things that had happened prior to his being tested positive — by the way. when was he tested positive?" This is when I lit my fuse.
He gave me two dates. ’85 and ’86. I said, “Okay, which was it? ’85 or ’86?” I never got a straight answer, and I said, “You’re a liar. Tell me. Give me a date. What are you hiding now? He’s already dead.” Hartman said. “We were waiting for an accurate test, which didn’t happen until 1985.” That’s the first thing that all his people point to — “We didn’t have an accurate test until 1985. Before then we were guessing.” My answer to that is, you’re dealing with somebody's life. It’s sort of like when the Pinto started catching fire. What did they do? They started looking into it and then they pulled the cars. By 1985 a lot of hemophiliacs had died. Lots had died in 1983 and 1984.
Certain people knew in 1983 that there was a problem with the blood Factor. The Cutter memo proves that. Cutter is one of the six large pharmaceutical companies that manufactures blood products, and they had a memo in hand from their attorney in 1983 that said, “We feel that there’s a large potential problem here, and I feel as your counsel that we should put in a warning label and an instruction sheet to the doctors, warning that it could be contaminated.” But Cutter resisted doing that for more than a year. This came out in one of the trials.
So even after talking with Hartman, I still cannot get a date for when my sons were first tested. The only thing that I have in concrete, from Steven’s medical records, is they put him through a whole battery of tests in the summer of 1987, just before they transferred him to University Hospital. So Hartman said at the meeting that he knew for sure Steven was positive in '86, and maybe ’85. I said. “Okay. I’ll give you the benefit of the doubt. Why did you keep my son in your facility from ’86. when you knew he was HIV positive, until September of ’87 ’’’
His answer was, “Well, I thought we could give him good care.” I said, “You’re lying, number one. Number two, if you transferred him because UCSD had the best care available for AIDS, why didn’t you transfer him there in ’86? It’s always been the best AIDS treatment center
“We felt that there wasn’t anything going on that we could not handle.”
“Baloney. He could have been in a clinical trial, he could have gotten on medication, you were not giving him AZT or anything. It wouldn’t have hurt my sons to be at UCSD in 1985. Why not test my sons immediately, find out what’s going on. then let them decide what to do?”
I agree with Rick. I think the money being made for Children’s Hospital on the Factor had a lot to do with it. Children's was like a retailer for the Factor. Over the long haul, they didn’t charge cost plus two percent. That was only for the heat-treated Factor. Before that, the hospital was making tons of money on it. Tons of money. I used to follow the costs.
I asked Hartman, Why didn’t you tell Steven he was positive until 1987? “We didn’t feel it was necessary —” I said. “What do you mean? He’s living with a lady, you know. We’re talking about two people that died because of this. You killed two people.” Of course, he doesn’t want to hear that. Anytime I can sec the man I will tell him he's a killer.
I’ve gotten very cynical since we’ve been victimized so badly with this whole thing. Hartman denies this, but the way I see it developing, I can envision the administration and Hartman getting together with the other pediac docs when they suspected something, maybe in ’83. but ’84 for sure. And I could see the administration doing exactly what the Red Cross did — that’s another memo — and looking at this whole thing in pure economics.
So they decided to do nothing, to hope for the best. To roll the dice and hope they lucked out. If they had come out in 1983 and given any indication that they had given my sons contaminated Factor. I’d have been down at my attorney’s office that afternoon. Looking back, the hospital decided to play a waiting game, hoping that not too many people would be infected. But they lost. We lost. My sons paid with their lives. We’re the ones who pay, not the hospital, and not the doctor.
And the Band Played On, reporter Randy Shilts’s definitive study of the AIDS epidemic, provides a reliable context within which the personal tragedy of the Valdez family played out. According to Shilts, hemophilia specialists at the federal Center for Disease Control in Atlanta first became suspicious in late 1981 that the immune system malady (which didn't receive the AIDS acronym until July 1982) was being transmitted to hemophiliacs through a blood-clotting agent called Factor VIII. manufactured from donated blood. The first public announcement from the CDC warning that AIDS might be transmitted through blood products came on December 10. 1982, in the “Morbidity and Mortality Weekly Report.” a CDC newsletter that is mailed to thousands of hospitals worldwide. The announcement also included an update on five new hemophiliacs who had contracted AIDS. Already, 6 of 100 hemophiliacs in Ohio had died of AIDS, and 3 more were ill.
It took years for the blood industry to reach consensus that Factor VIII was contaminated. According to Shills, the National Hemophilia Foundation resisted having hemophiliacs identified with a “gay disease.” And the blood product manufacturers, as well as the blood banks, fought government efforts to prod them to test their blood pools for the vims that was causing AIDS. Today, many of the nation's approximately 10,000 HIV-infected hemophiliacs look back on the early foot-dragging as almost criminal negligence that has resulted in “genocide” for them.
Early CDC efforts to radically change the way blood was collected were blocked by the FDA and the Reagan administration’s Public Health Service. Shilts describes CDC staffers in 1983 as being “enraged” at the government’s inaction. Dr. Bruce Evatt, the CDC’s hemophilia specialist, “had not anticipated that the CDC would be so definitively thwarted in its influence on public policy,” Shilts writes.
Adding to the frustration of hemophiliacs and their families is the difficulty of suing the manufacturers of Factor VIII, who are legally shielded from product liability laws because Factor VIII is considered more of a service than a product. Many hemophilia activists are calling for a congressional investigation into the actions of the blood industry, the Food and Drug Administration that regulates it, and the National Hemophilia Foundation in failing to prevent contamination of the blood supply.
Shilts concludes. “The lost opportunities of 1982 would be explained later with the chorus: ‘How were we to know?’ This had no meaning in 1983. By then, vast numbers of people knew better, but confronted with knowledge and the chance to do something, they usually did the wrong thing, if they did anything at all. At the time, their postures seemed like the right thing to do in order to preserve civil rights or, say. the economic viability of the blood industry. The problem, of course, was that such considerations constantly overshadowed concerns of medicine and public health.”


The Son, Rick Valdez: In a lot of ways my brother and I were opposites. Steven was conventional and I was the rebel. He was the good boy, and I always questioned things. We were both severe hemophiliacs, and we’d been going to Children’s Hospital — I can’t even tell you for certain, but since the mid-’60s. When we were young we were always at the hospital because we were bleeding all the time. I had a lot of emergencies, and there was always bleeding into the joints, so we were there to get the blood. First the whole blood, then later the cryoprecipitate, the cryo, and then starting in, like, 1972, the concentrate called Factor VIII that causes our blood to clot normally. It was the Factor VIII that saved us at first, then it killed my brother last June. He was 25 when he died of AIDS. And it will eventually kill me too. I’m 31.
When I was really young, when Factor VIII first came out, at times we were on what they called a prophylactic treatment, which means you would get it regardless of whether you were bleeding or not, as a preventative. You’d get the Factor intravenously every couple of days. It's like brushing your teeth after a while. We learned to do it ourselves at home, and it was a hell of a lot better than having to go to the hospital.

But we weren’t on the prophylactic treatment very long. Eventually we just started treating ourselves when we felt a twinge indicating a bleed. It’s a little hard now to tell when there’s a bleed because of arthritis in my knees and in my ankles. Back in the mid-’80s is when the arthritis got real bad, and it's hard to discriminate now between the arthritic pain and the pain that occurs when there’s a bleed going on.
So once we started using the Factor, we only had to go to the hospital every few months for checkups, and that was a lot better. I started doing my own IVs when I was about 14. And all that time we had the same doctor, Gary Hartman.
I looked at him as someone you could trust. I had complete faith in him. and because of that I partially blame my trust in him for me not being more inquisitive, not asking questions sooner. Because when this AIDS thing hit the newspapers and television in the early 1980s, they were saying, oh, well, it’s affecting gays — and every once in a while there would be a little thing that, hey, it might affect hemophiliacs through the blood products. And I can remember thinking, well, you know, Gary’s not saying anything about it, so I didn’t figure there was anything to go in for.
Then at the end of 1983, Gary called a meeting of his hemophiliac patients. I had no idea what AIDS was and in fact ended up telling another hemophiliac that was there, hey, if Gary wasn’t saying anything about it then I wasn’t going to worry about it. It seemed like the media were changing their description of it and who it was affecting almost daily. If you tried to keep up with that, you would realize it was worthless, because there were no absolutes at all.
So the way this meeting was set up, we didn’t get a phone call or anything. He didn’t call and say, “Hey, this could affect you, it may be in the Factor, better come in and talk with us right now.” What we got was a notice in the mail announcing this meeting a couple of weeks ahead of time. And of course, in the meantime, we’re still giving ourselves the Factor. Gary has no idea how many times we’re doing it. So in my mind this thing was really downplayed.
Steven was at the meeting with his girlfriend Linda. Some of the other hemophiliacs were there with their wives. Gary’s presentation was low key — “Well, here’s my view....” And the gist was, he didn’t know for sure if the Factor was contaminated. The actual test to detect the AIDS virus wasn’t developed until 1985. All he said was, well, if you want, you could try to go back to the cryo, which was the earlier way we were treated and entailed going into the hospital for treatment.
But to me, based on the facts he presented, the chances of us getting this thing [AIDS] were slim to none. The air he had about him, there was no panic. He said there was a heat-treated Factor that would probably take care of any possible contamination, and that was supposed to be available within a couple of months. My brother came away feeling the same way I did. that this was no big deal. It turned out that he died of AIDS, and he gave it to Linda and she died of AIDS last summer on Steven’s birthday, and I’m HIV positive. Basically, almost every severe hemophiliac who was bom before 1985 is either dead or is HIV positive.
I look at it in comparison to the Tylenol poisoning. Remember that? Someone died after taking Tylenol and it was a national alert, and Tylenol was taken off the shelves immediately. But the Factor continued to be sold to us after they suspected it was contaminated. We were poisoned. That’s a crime.
The Doctor, Gary Hartman:
I recall my message at that meeting. Actually, there were two meetings about six months apart. They were very somber, very upsetting. It was a time when it became clearer and clearer that there was big problems, that the Factor was contaminated. It was difficult to know how to react.
First of all, everyone who had been on prophylaxis to prevent bleeding, all that was stopped, which was real hard. Some people didn’t want to stop it. There were kids who felt real normal using Factor three times a week, who could play baseball, and all of a sudden without the Factor they’re hemophiliacs again. I said we can’t do this anymore, because we don’t know which lots [of Factor VIII] are bad. People had their own supplies at home, and they ’re going to do what they’re going to do. all I can do is present material, give recommendations.
We talked about development of AIDS at that meeting. We didn’t call it HIV then, it was HTLV-3. Rick and Steven were at that meeting; and other people there came away with a different perception than they did. One man came away believing that he was already infected with the virus. It was very somber, very draining.
We talked about going back to cryoprecipitate, and I remember at least one patient — and there were probably others — who said that cryo was really bad. it was hard to deal with. “Life was lousy with it, and I’m not going back to that.” And how clean was cryo? It wasn’t made from pooled blood, true, but when you start to use 10 or 20 bags at a time, all of a sudden that’s a form of pooling. There was no test available to determine what was clean and what wasn’t. If Rick was waiting for a signal from me to go back to cryo, well, I wasn’t going to give one, because it didn’t seem like it was a good idea at the time.
The fact is. the die was cast by the time we realized it was a problem. It’s true that the first announcement from the Centers for Disease Control about hemophilia and immune failures was in July 1982. But there was no consensus in the hemophilia community until April of ’83 that this was a blood problem. People were already infected. I think most of them were already infected at that point. We didn’t know for sure, but that was my fear then. I didn't know what to think, but that was my fear.
As you approach something like this, you try to look at the facts, you try to plumb the emotions, and then try to make a recommendation and problem-solve. Thinking back on those times — the problem-solving thing was terrible, it was very difficult. Some people really cope and go through the world by taking information in. as much information as they can, even when it’s tough. And some people have more difficulty with that. It’s just another way. another style of living or coping, to tend to deny and push things out. And the other thing is. Rick was having memory problems at the time. "He had had a brain hemorrhage a couple years before and was having some memory problems.
Did I consider taking my patients off Factor? You know, I just talked to some other people about this. I don’t think any doctor would have taken everybody off of all of their Factor. It would be a really very difficult decision. The bigger centers, L.A. Children’s, L.A. Orthopedic, and San Diego Children’s, we were sort of all very closely aligned. None of us thought we should drop Factor completely. And that was not the recommendation from the National Hemophilia Association. Even if we had all dropped Factor in 1983, it might not have made much difference. You know, once a good HIV test was developed. some lots of Factor were found to be contaminated as early as 1978.
I’ve heard the term “medically induced AIDS" used by some hemophiliacs. Well, what a strange term. Something was prescribed, something which was used, appreciated. and welcomed by the patients, and none of us knew that it was tainted. And it wasn't tainted, initially. May I give you an example of this? In 1982. Richard Valdez had a headache at work, and he went home and told his grandmother that he was going to sleep. And she gave him a Tylenol. Now headaches and sleepiness, put together, are strong evidence of something wrong inside the brain of a hemophiliac. What it indicates is a bleed. You don’t have to have any head injury; it can be spontaneous intracranial bleeding.
Now we found out about this sort of by accident. I think Dick [Rick's father] had called Sallie [Rick’s mother], and Sallie had called Rick's grandmother, where he was living, and said, “Why don’t you go and wake him up?” The grandmother could not wake him up. He was basically dying.
They called us [at Children’s Hospital], they called 911,1 talked with the police over the phone, and I talked with the paramedics. Now what I had to do was get the paramedics to bring him to our facility, which is something that takes, like, a Richter 7 of energy because they are programmed only to go to the nearest hospital. I’m on the phone screaming at them, saying there's no hemophilia care at the nearest hospital, however fine a hospital it is. Get him to where I can do it, which was Sharp’s emergency room, because Children’s didn’t have an emergency room at that time. And they did. This was, like, miraculous. I had 4000 units, lots of vials, of Factor VIII.
Rick was terribly sick. He was basically dying. His heart rate and his breathing rate started to change. We gave him the Factor to try to stop the bleeding in his brain. Finally, an anesthesiologist came down, got him breathing, took him to a CT scanner, found this big intracranial bleed; I had a neurosurgeon there, took him up to the operating room, and I stayed with him. They evacuated a big blood clot that was all the way through into the brain. It was an amazing wad of stuff. The surgeon said, “I still think he’s bleeding.” So I gave him more Factor. This is 1982 Factor. For all I know, this is where the virus came in. There was no question of using Factor — if you’d wanted to use cryo or fresh-frozen plasma, it wouldn’t have worked. You needed such huge volumes.
Even if we knew then that something was wrong with the Factor — which we didn’t — what would you say? Let him die? Let his head bleed? Of course not. But this is 1982, and in retrospect the Factor was contaminated. So if he got the virus then, that was medically induced, okay? I don't know; I think people are expecting, looking through 1992 eyes, to make the world different from the way it was. We did the damnedest best we could.
I have not felt guilty about it. I have felt thoughtful, somber, unhappy; there are a lot of different feelings I have. But as far as guilt, no. Responsibility? Well, yes. We share the responsibility for taking Factor. Yeah, we did it together, we did it as a team, and we share responsibility, my patients and I. In my heart of hearts, I know I did not give them AIDS, and I could not have prevented it.
The Mother, Sallie Bankston:
I have to tell you one thing about Dr. Hartman. I had always felt that he was a very special doctor. I looked up to him. He always seemed very sensitive to the needs of the guys and even of the family. And it was just a shock to me when all of a sudden he calls a meeting and they’re going to explain things to the guys. That, of course, is when they tell us [about AIDS] for the first time.
And didn't really make a big deal out of it.
I was not at the meeting, but the boys came home and said there was something going on about the blood, you know, the Factor that they got. And that’s the first time I knew that the Factor VIII they used was bought off the street, so to speak.
They said not every thing was in yet, but it was looking like the blood may be contaminated. And at that time I instantly called and tried to get some answers. I called the hematology nurse at Children’s, Bettie Spangler, and she said, “Don’t worry about it yet, Sallie, because we’re still just getting in the information on it.” But I told her, no, that's not the way it’s going to be. 1 was going to start looking into what it was all about. So I decided where to go to look would be the San Diego Blood Bank. I thought maybe the blood bank would be able to bail us out. 1 had the hope that maybe the boys hadn’t been exposed yet.
The blood bank could make fresh Factor VIII, but they only did that for small children. There was a shock period I went through when I got so knocked down by the blood bank saying there was no way they could supply us with fresh Factor VIII. They didn’t have enough blood, it was impossible. I tried to fight them, but the administrator stood firm.
It wasn’t until much later that I found out that everyone involved was making big bucks off the Factor, including Children’s Hospital. It came out accidentally. It was said to another parent, after we were all dumped over to University Hospital. that, boy, we really miss having that Factor VIII in our budget because we were really making money off of it. And I said, "What do you mean?" I hadn't even thought about anyone making a big profit on it.
Children’s asking us to leave and go over to University Hospital was like a nightmare that I'll never forget. This is the summer of 1987. Steven was already diagnosed as having, being in the illness. Children's was looking at what AIDS was. and it was really too much for them to handle. We were dumped, after being with Children’s for more than 20 years. Every adult hemophiliac got dumped when a few of them started getting sick. At first they said, now, we'll give you a year, it’ll take about a year to get you transferred over there. Well, it took them maybe a month. They wanted us out of there. We had no idea what was going on. It happened so quick, and we just didn’t know what was happening.
I did not know the boys had been tested for HIV. They never told them and they never told us, the family. It was all done underhanded, and the only reason it was found out was because a friend, another person with hemophilia, saw the results of an AIDS test in his records, saw everybody’s name, and Rick’s name was negative. And he got so excited for Rick. At least Rick was negative, you know. This was 1987, but the test had been done two years earlier. In 1987 we were still in the dark, but we knew by then that something was really bad about this AIDS thing. Of course, later Rick asked to be tested and he came up positive.
Dr. Hartman never did say to me that the Factor was contaminated and Steven had AIDS. He only told me that Steven was very ill. He did confront me with that. He went into the particular parts of the body, that his liver, that his body was not making platelets, but he didn't make a personal thing of calling it AIDS. Every word that came out of his mouth was very measured, because he supposedly didn’t know what was going on either. Now I feel that this was all untrue. I feel he knew a year before he moved us to UCSD, and we were all kept quiet by not being told. The topper was, when Steve got sick, we all got dumped.
Dr. Hartman called a big meeting of all the hemophiliac families to tell us that this was the end, we were all going over to UCSD. and I want to tell you, our hearts all fell. What was going to go on for those next few months was a nightmare. If you’ve gone to the same doctor for 20 years and all of a sudden you're tossed to this place that you cannot believe — UCSD is just a maze of people. 1 guess we'd been spoiled. Dr. Hartman said they were being moved because they were adults — he didn't say anything about AIDS — and they needed to be with doctors that treated adults, and that was his big way of getting us to move without any trouble. But many of his patients had been adults for several years; Rick was 26 then.
I was so devastated. I just slid into the position of. What do we do now? And that was to go to the doctors most of the time. And go from one emergency to the next emergency. And knowing that I was losing my son. I’ve lost the fight, you know. I was having to fight at UCSD just to get decent care, because they didn’t have a lot of hemophiliacs then or know how to treat them, so we got into a lot of care problems. Many limes an intern would come along, see us in the emergency room, and they just didn’t know what they were supposed to know. I understand they’re getting better now. Steven was the one who trained them, and you know, it was a sad way to go. Leaving Children’s was like leaving the Marriott and going to a low-budget motel.
When you sit for a couple of hours in a room full of AIDS patients that are so sick, can you imagine how that makes you feel? Rick was still well, and he’d have to go and see that. I know with Steve it just really got to him.
Last spring, right before Steven passed away, he went into UCSD and they needed to give him something intravenously. Anybody that knows hemophiliacs in the medical field knows that you really have to tourniquet anything where there’s been something bleeding. And so the woman gouged and pushed and pulled and she couldn’t find a vein, so she just gave up on that arm and went on to the other arm. When I got there his arm was swollen up like a balloon, and it was turning purple and black. I asked to see the doctor that oversees the whole thing, and he said to me, well, Steven’s a hemophiliac, those things can happen. I said, "Don’t give me that stuff, it’s not true. This does not need to happen. We’re in a new age now. Where are you from?”
Steven suffered over that arm until he died, about three weeks later. His whole arm was filled up with blood, right into the fingers.
You know. I’ve thought about all this, and I think Dr. Hartman could have handled that initial meeting better. I don’t think he really gave the boys a choice. Everyone should have been given the choice of being more crippled or even losing their life, gambling, rather than go on using this Factor that is tainted. If you're working in the medical field, you'd have to have known that thing was going on with the blood supply way before they told us.
Linda. Steve’s fiancee, was at that meeting. When I asked what happened at the meeting, she said it was no big deal, no emergency-type thing. If I was Dr. Hartman or the nurse. Bettie Spangler, and I’d seen little Linda sitting there — she wasn’t a hemophiliac — how could they let them walk out of the room? When there’s an emergency, you don't just say. well, by the way, there’s an emergency. It seems like it was just kind of pushed under the carpet.
Rick:
Bettie Spangler, this woman who had been our nurse for so many years, came to my brother’s memorial after he died. I wasn’t sure I wanted to talk to her. And she has the nerve to say that when we went to the other hospital, they lost a lot of money in Factor sales. She said that to me! I couldn't believe it. And that’s the whole point of this whole thing.
Most hemophiliacs don’t have private insurance; we’re covered by the State of California.
At some point in the 1970s, a law was passed that created the Genetically Handicapped Persons Program, and that covered hemophiliacs once we reached 21. Prior to that we were covered by the Crippled Children’s Society. So all of our Factor was purchased through the hospital, and the hospital was reimbursed at a profit. And then when the heat-treated Factor came in in 1983, the cost of it doubled. Now it costs about $1000 for one treatment, and some hemophiliacs need several treatments a week.
Sometime in 1985 these brokerage companies started coming to sell us the Factor. That year this broker came to San Diego and was basically trying to infiltrate the hemophilia population here locally so he could sell his product. He was a hemophiliac too. He came to me and asked if I wanted to start utilizing his services. And I can’t believe I said this, but I did. "Well, let me talk to Dr. Hartman, because they have taken care of us so well, I want to see what he says." In 1985 I still didn’t know what was really going on. The idea was I would get half my Factor from this brokerage firm and half of it from Children’s.
So I asked Bettie Spangler, because I guess when I thought of it she was there, and she went, “You’re supposed to talk to Gary.” But she talked with him and came back to me later and said, "Well, we’d rather not have you do that because this is how we keep our clinic open is by selling this stuff.”
And when my dad and I confronted Gary last summer after my brother had died, he — I don’t know what kind of case he was trying to build in his favor — but he said he went to the administrators of the hospital and tried to advocate for us to keep us at Children’s, because the amount of Factor they were selling to us was actually helping pay for other areas in the hospital, not only our clinic. And this is what Gary himself said.
My whole point is that Children's Hospital was making big money selling this stuff to us. And Gary Hartman tells us that he went to the administrators who wanted us out of there because they knew what was coming, they wanted us out of there, but he supposedly went on our behalf to say keep these guys here — there were about ten adult hemophiliacs — keep them here because we make such a good profit on selling them the Factor that they help support some of the other clinics in the hospital. They hung on to us as long as they could so they could continue to make the money off of us.
My brother could have gone over to UCSD sooner. Maybe he'd still be alive today if he had gone earlier to where they were treating AIDS patients as a specialty. I don’t know if that would have helped, but it might have. They definitely knew most of us were HIV positive at least a year, maybe two years before they dumped us. I can’t tell you exactly when they knew it, but I was tested without asking to be tested and without my knowledge.
When I found out about it was 1987, but I think the test was done in 1985. Another hemophiliac patient at Children’s Hospital found this list of all the hemophiliacs at that treatment center. It was in his medical file. Each of us had been tested for the AIDS virus. They leave your records out for your doctor to look at, and this guy always looked through his and he found this list. I was the only one on the list who tested negative. I was never informed of it. I went to Gary then and asked to be tested, and my test came back positive. This was right before they moved us to UCSD.
So I went into my own denial. I mean, this is insane. You gotta remember it’s died down, as far as the publicity that AIDS gets now and depictions of people dying in the hospitals. You don’t see that anymore. But back then you did. And it’s like, no way do you think you have this. And so I kind of for a while let it ride at that. Okay, one test was negative and one test was positive, so as far as I was concerned, you know, that didn’t tell me anything, okay? And so I went along for a while, until sometime in ’88, before I asked to be tested again. Of course, it was positive. And in the meantime my brother got sick.
He had moved back in with my mom in ’86, and sometime later on he and his girlfriend Linda got another apartment and lived together again for just a few months. And then she started going out with a friend of my brother’s, and my brother got sick then and never got well. He moved back in with my mom then. My mother chased Linda down after she and my brother were broken up and said, “Hey, you gotta get tested." That was my mother’s project, to go and get the girl tested, because Linda didn’t really care. Turned out she was positive too.
To say it was hard on my mother to nurse Steven and watch him die is an understatement. She still hasn’t recovered, and I don’t know that she will. When I start getting sick, I don’t know what’s going to happen, where I’m going to go, because I can’t stay with my grandmother. She couldn’t handle it. And I wouldn’t want my mother to go through it again. My parents divorced when I was about eight, in the late ’60s, and they’re both remarried. Moving in with my dad isn't an option.
I didn’t see my brother too often, only really at the end, the last eight months of his life, and it was pretty bad. He was in and out of the hospital. and I visited him.and ran into him two times in the emergency room. Toward the end of 1990, he was at the hospital every day. and on two separate occasions I was there for something and I felt. well. I’m going to go by the emergency room, which is usually where you have to go to get any care at UCSD. On both these occasions my brother was there, and it was insane what I saw.
The main thing I remember was he had this thing called a neuropathy; I can’t even tell you exactly what it is. It’s a type of nerve damage affecting the central nervous system. He was in agony. The way he described it to me was. these nerv e impulses were moving through his body and they were doing something so outrageous to his system he could see his skin moving. That’s how he described it. and it was agony. He was on a gurney, and I tried to step away to see if I could get him some relief, and the nurse’s attitude over there was, well, we don’t want to give him any pain medication because it will cover up the symptoms. And as I stepped away Steven started bawling. He just didn’t want me to go away because he was so afraid. He didn’t know what was going to happen, and they wouldn’t give him any medicine. You know, he’d had this thing for quite some time, so they knew it was neuropathy. I don’t know what the hell their problem was.
You know, these are the kinds of things I have to look forward to. I already witnessed my future when I saw what my brother was going through. They put you in a room with at least two other guys that arc dying of AIDS, and they’re in different stages. I mean, it’s just a horror to see these guys, some of them are skeletons and they’re tied to different machines. It’s just a nightmare.
I’m fucked. There’s no other way to say it. I don’t have an alternative. I have no insurance. I’ll never get insurance. I'm a ward of the state. And what the state is, you go to UCSD and whatever you can get over there, that’s what you get.
I haven’t really thought about suicide because I don’t want to die. Gimme drugs, gimme morphine. My brother did it. and — I can say to you right now I haven’t sat down and said, okay, once it gets to the point where I can’t deal with it. I’m going to kill myself. No. Whereas I talked to this other person who was gay who had AIDS, and he told me that if it gets to a real bad point, he’d already been through hell, he had a w ay planned and was going to do it with pills — downers. But he never did it, because it killed him.
Dr. Hartman:
In 1985. just prior to the development of a reliable test for the AIDS virus, someone from a laboratory called me and said, “I have an investigational test kit for HTLV-3. I would like some specimen to test. What would you think?" And I said okay.
We sent him blood samples, and he tested them and he sent the results back in an informal way. and we put it in each person’s chart just as it came in. For better or for worse, that’s how we did it. Richard came back negative on that test. I don’t remember if all of my 20 or so patients were tested, but several were.
On that test also was another young man who had a different illness, who’d had a lot of transfusions. He was clearly dying of AIDS, and his test was negative. Okay. In fact, we sent two of his samples to be tested, and they were both negative. I knew that the guy had AIDS. He was wasting away.
So here I was with a test which was unproven, and I knew that it had certain weaknesses, like it had missed this guy. This is early 1985. and the real AIDS test was to come out in the middle of that year. I didn’t know that the real test was so close. So what would you do for someone who had hemophilia who had a negative HIV test? What would you do? Put him on the best product available, for one thing, to protect that person. And if he’s negative, the best product available for a hemophiliac is clean Factor. He’d been on heat-treated Factor for over a year. And that’s what we did for the ones who tested positive too. I was afraid of that test. I didn't trust it. So why did we do it and why was it around? If I remember right, it was a desperation kind of thing. It was investigational, but it had clinical implications. And the real testing came out soon after. But there was a big rigamarole about that. It was very difficult to get testing.
I didn’t inform the patients who’d been tested because I knew it was an inaccurate test. Did I start testing my patients when the real test eamc out ? You know. I think so but I can’t remember. And when I review the charts I can’t find anything. Once people started realizing the implications. there were no results of AIDS testing allowed in medical records. Not even the order that you’d been doing AIDS testing. You could get thrown in jail even for telling another person that a patient had been tested. From a medical standpoint, this was very awkward. So testing results were kept separately in a division of medical records under lock and key. And I recently went up and looked, and there was nothing there. I don’t know. It was a very awkward time.
A lot of people didn’t want to know and didn’t want to be tested. That’s one thing. A lot of spouses didn’t want to be tested either for years afterward and probably still don’t. You know, there’s a blank. I don’t remember if we tested everybody. There were a lot of things going on, a lot of very busy and important things. I had a talk with a hemophilia nurse at the time, and her recollection was, yes. that we had done the testing.
I'm sure we sat down with patients and talked about having positive tests. I remember it. I would hope and think it was a matter of policy but. you know. I don’t recall if we talked to everybody. Rick says he was never told? Okay, on the other hand, maybe it was sort of almost a given that everyone was positive.
Then shouldn’t they have been given the best AIDS treatment available at that time? Well, what was the AIDS treatment? What was it? AZT was being worked on. but only w ith very sick patients, not hemophiliacs and not children. Very sick gay men who were basically dying. I remember that these people started doing better. But AZT is a very toxic drug. You don’t take this for a cold, okay? You could really do a lot of harm with this drug. They tried it on people who were a little less sick, and lo and behold, these people did much better too. Okay. Amen. Eventually it was tested on gay men who were HIV positive but asymptomatic. Then the study came down to hemophiliacs.
But in 1987, no one was giving AZT to asymptomatic people. It would have been crazy. It was not indicated. So the point is, there was no best treatment for positive hemophiliacs. There was nothing else being done. It was really important for me to get the best that was available, and that’s why I started sending them over to UCSD when it became clear that that clinic could be more helpful.
Now I want to make it real clear that it was the adults, whether or not they were HIV positive. who were sent to University Hospital. True, basically all of them were positive. But the children. the hemophiliacs who were not yet 18, stayed at Children’s, whether or not they were HIV positive. I did not send HIV people away, okay? I sent adults away.
“Dumped” certainly is a charged word, isn’t it? I want to clear that up now. When they started getting sick — first of all. let me tell you about another patient. I won’t identify him. He called me one day to say he’s got the chicken pox. Now chicken pox in you or me or a normal kid is not bad. But chicken pox when you’re immune-suppressed can be devastating. It’s a really powerful virus if you don’t have an immune system that works. I said, “Come over to the hospital. I’ll meet you outside, in the parking lot.” We don’t even let chicken pox patients inside the door. I looked at him, I said. "I want you to get in the car, go right to UCSD. I’m going to call and tell them you’re coming." And I did. Where was I going to put him? Anybody over the age of 18 can’t be hospitalized at Children’s.
He got to UCSD. he was admitted, he was looked at. Twelve hours later he was on a ventilator, very sick. He was pulled through by their critical care, their pulmonary doctors, and a whole team with a lot of expertise. I was really impressed. That was very reinforcing to me. I had no place to hospitalize and take care of him. though Children's was wonderful. It’s terrific, but there’s nobody over the age of 18. and even 16 to 18 is borderline. So when one person got sick, I started to realize I had no place to put these people. And I had enjoyed this wonderful relationship with them since 1971; we grew up together in many ways, we went through a lot of things together.
In certain kinds of childhood illnesses, such as cystic fibrosis and muscular dystrophy, kids generally move out of children’s hospitals when they’re 18. But that isn’t generally true of hemophiliacs, where internists aren’t that familiar with the principles of treatment. Plus, with hemophiliacs you establish this primary, close relationship. It’s like family, so you hang on. And it was fun. I would see them all every 6 to 12 months and go over their hemophilia stuff and try to coordinate their care.
But eventually I ended up taking care of adults. It was okay when they weren’t getting sick and there was no treatment for HIV; I might as well do it. I mean. I knew them. A lot of them came in and talked because they were worried about HIV. There was a lot of that. But I realized that the decision was whether to continue this wonderful relationship or to get the best medical care, and I didn’t have it. It was an agonizing, soul-searching. very difficult decision made on medical principles only. But I know it felt like abandonment to them.
And now I’m being faulted for transferring them to University, and I’m being faulted for not transferring them earlier. It’s difficult to respond to the criticism, but I’m going to go down swinging.
It was my decision to transfer the adult patients. I went to the medical director and I said. I want you to know what I'm doing because. I mean, this is, like, big stuff. I think it’s for the best. Did the cost of losing the Factor ever come up? Never. Money for the hospital had nothing to do with my hanging on to the patients until 1987. I know how that question came up It was when the entrepreneurial brokers started moving in. and I asked someone, a patient. Would you keep buying your Factor from us? Would you consider it?
The brokers were actually giving very good service, which we weren’t doing, and the big hospitals sort of had to adjust to this. It was a new world. But the brokers had a bad rep. They had a rep that they were giving medical advice, and that didn’t go down well with the hemophilia centers. It was an issue of medical control The money was secondary. The thing I was concerned about was medical control.
Most of the patients were on MediC al, or GHPP. and some were on private insurance What is the reimbursement for Factor? It was about cost plus two percent. That’s it. So there was a profit there, and there was more profit from people with private insurance, okay. It was not a gold mine, but there was profit. You have to look at the net versus the gross cost, and sometimes the pharmacies look at that and sometimes the hospital administrators do. and I know this is an issue. But you have to look at how we treated them medically too.
There was me. there was an orthopedic surgeon who saw patients, who I don’t think even charged except if he did operations, which was a few. There was a specialized hemophilia nurse who was paid by the hospital. There was a social worker who was paid by the hospital. The routine clinic visits were about every six months; everybody sees the patient, it takes a long time. And what was the payment — $50. $75? Not a money-making thing. That's not why you go into hemophilia care. And there were times when administrators looked at it and said. look, you have 25 patients, we have limited resources. People arc ratcheting down the amount of money that goes to hospitals, why not cut your social worker? And they did. They cut our social worker, and that hurt people. The Factor sales brought some money in, and it gave me some clout, gave me some sort of validity with administration at a time when they were thinking money, bottom line. That clout helped the patients. And I want to make it super clear that this has nothing to do with personal money to me.
I’m 50, and I’ve recently retired. I have been in pediatric hematology and oncology for about 20 years, and I had a lot of rewards. It’s been really good to me. And I think I'm really good at it. But it begins to take its toll after a while, and I decided that I had to make a change. I said goodbye to an awful lot of people, and I've been to enough funerals.
The Father, Dick Valdez:
When I found out Children's Hospital was having a telethon last summer, I said. “Let's picket the thing.” Steve had only been dead about two weeks. Rick, and myself, and my mother, Rick’s grandmother, were out there, and later another hemophiliac joined us. People who worked at the hospital were giving us the bird, and the volunteers coming in didn't know what to think. I stayed on the sidewalk easement. I wasn’t about to get on their property. One of the security guys who was in a suit came out and tried to bait me onto the property. I said, “If you want to know why I’m here and what I’m concerned about, come down and read." We had Steven’s obituary, and we had all the basic facts laid out.
He wouldn’t come down, but he went and got another suit-type guy. I guess one of the vice presidents. Children’s has got a lot of vice presidents — and eventually, the next day actually, a guy was sent out who was a human relations type, and he was a total mediator. He asked. “What does this have to do with us?” I said, “Well, because you took care of my son for 20 years. The only reason he went to University Hospital was because he was HIV positive, and your doctor said you people couldn't handle it.” At that point I didn’t know that Hartman knew Steve was positive for a year before he transferred him. Then he said. “Well, what are you saying?” I answered, “He was in your care when he got infected, which nobody has ever survived. So as far as I’m concerned, Children’s Hospital killed my son. plain and simple. Your doctor killed my son."
He asked what I wanted, and I told him I wanted to sit down face to face with Dr. Hartman and find out exactly what happened. “Well, he’s in the midst of retiring.” Yeah, isn't that convenient? Eventually we were given a meeting with another doctor who is part of the administration, and of course, his defense was, “We didn’t know.” That’s how they all do it. That’s how the pharmaceutical people do it. that’s how the blood bank does it, the medical community in total. That’s their whole defense. But I don’t accept that at all. There’s too many facts, too many things that have come up in trials. There’s trials all over the country involving hemophiliacs. Some have been settled out of court, with no details announced as part of the settlement. That’s the typical settlement, in fact. Others are still pending.
So this doctor told us we were entitled to know what happened, and he set us up a meeting with Dr. Hartman. But he made us understand that Hartman was not an employee of the hospital, he was an independent contractor. We met in late July, the five of us — Dr. Hartman, Bettie Spangler, the nurse, this other doctor who set up the meeting, and Rick and myself. It started badly. I mean. Dr. Hartman was trying to be very friendly, and we immediately let him know that we weren’t there to be friendly.
The first thing I said was. “Tell me what happened. Why did my son die?" And of course, he went into the medical explanation. I said. “No. I don’t want the medical explanation. Why with all the things that had happened prior to his being tested positive — by the way. when was he tested positive?" This is when I lit my fuse.
He gave me two dates. ’85 and ’86. I said, “Okay, which was it? ’85 or ’86?” I never got a straight answer, and I said, “You’re a liar. Tell me. Give me a date. What are you hiding now? He’s already dead.” Hartman said. “We were waiting for an accurate test, which didn’t happen until 1985.” That’s the first thing that all his people point to — “We didn’t have an accurate test until 1985. Before then we were guessing.” My answer to that is, you’re dealing with somebody's life. It’s sort of like when the Pinto started catching fire. What did they do? They started looking into it and then they pulled the cars. By 1985 a lot of hemophiliacs had died. Lots had died in 1983 and 1984.
Certain people knew in 1983 that there was a problem with the blood Factor. The Cutter memo proves that. Cutter is one of the six large pharmaceutical companies that manufactures blood products, and they had a memo in hand from their attorney in 1983 that said, “We feel that there’s a large potential problem here, and I feel as your counsel that we should put in a warning label and an instruction sheet to the doctors, warning that it could be contaminated.” But Cutter resisted doing that for more than a year. This came out in one of the trials.
So even after talking with Hartman, I still cannot get a date for when my sons were first tested. The only thing that I have in concrete, from Steven’s medical records, is they put him through a whole battery of tests in the summer of 1987, just before they transferred him to University Hospital. So Hartman said at the meeting that he knew for sure Steven was positive in '86, and maybe ’85. I said. “Okay. I’ll give you the benefit of the doubt. Why did you keep my son in your facility from ’86. when you knew he was HIV positive, until September of ’87 ’’’
His answer was, “Well, I thought we could give him good care.” I said, “You’re lying, number one. Number two, if you transferred him because UCSD had the best care available for AIDS, why didn’t you transfer him there in ’86? It’s always been the best AIDS treatment center
“We felt that there wasn’t anything going on that we could not handle.”
“Baloney. He could have been in a clinical trial, he could have gotten on medication, you were not giving him AZT or anything. It wouldn’t have hurt my sons to be at UCSD in 1985. Why not test my sons immediately, find out what’s going on. then let them decide what to do?”
I agree with Rick. I think the money being made for Children’s Hospital on the Factor had a lot to do with it. Children's was like a retailer for the Factor. Over the long haul, they didn’t charge cost plus two percent. That was only for the heat-treated Factor. Before that, the hospital was making tons of money on it. Tons of money. I used to follow the costs.
I asked Hartman, Why didn’t you tell Steven he was positive until 1987? “We didn’t feel it was necessary —” I said. “What do you mean? He’s living with a lady, you know. We’re talking about two people that died because of this. You killed two people.” Of course, he doesn’t want to hear that. Anytime I can sec the man I will tell him he's a killer.
I’ve gotten very cynical since we’ve been victimized so badly with this whole thing. Hartman denies this, but the way I see it developing, I can envision the administration and Hartman getting together with the other pediac docs when they suspected something, maybe in ’83. but ’84 for sure. And I could see the administration doing exactly what the Red Cross did — that’s another memo — and looking at this whole thing in pure economics.
So they decided to do nothing, to hope for the best. To roll the dice and hope they lucked out. If they had come out in 1983 and given any indication that they had given my sons contaminated Factor. I’d have been down at my attorney’s office that afternoon. Looking back, the hospital decided to play a waiting game, hoping that not too many people would be infected. But they lost. We lost. My sons paid with their lives. We’re the ones who pay, not the hospital, and not the doctor.
And the Band Played On, reporter Randy Shilts’s definitive study of the AIDS epidemic, provides a reliable context within which the personal tragedy of the Valdez family played out. According to Shilts, hemophilia specialists at the federal Center for Disease Control in Atlanta first became suspicious in late 1981 that the immune system malady (which didn't receive the AIDS acronym until July 1982) was being transmitted to hemophiliacs through a blood-clotting agent called Factor VIII. manufactured from donated blood. The first public announcement from the CDC warning that AIDS might be transmitted through blood products came on December 10. 1982, in the “Morbidity and Mortality Weekly Report.” a CDC newsletter that is mailed to thousands of hospitals worldwide. The announcement also included an update on five new hemophiliacs who had contracted AIDS. Already, 6 of 100 hemophiliacs in Ohio had died of AIDS, and 3 more were ill.
It took years for the blood industry to reach consensus that Factor VIII was contaminated. According to Shills, the National Hemophilia Foundation resisted having hemophiliacs identified with a “gay disease.” And the blood product manufacturers, as well as the blood banks, fought government efforts to prod them to test their blood pools for the vims that was causing AIDS. Today, many of the nation's approximately 10,000 HIV-infected hemophiliacs look back on the early foot-dragging as almost criminal negligence that has resulted in “genocide” for them.
Early CDC efforts to radically change the way blood was collected were blocked by the FDA and the Reagan administration’s Public Health Service. Shilts describes CDC staffers in 1983 as being “enraged” at the government’s inaction. Dr. Bruce Evatt, the CDC’s hemophilia specialist, “had not anticipated that the CDC would be so definitively thwarted in its influence on public policy,” Shilts writes.
Adding to the frustration of hemophiliacs and their families is the difficulty of suing the manufacturers of Factor VIII, who are legally shielded from product liability laws because Factor VIII is considered more of a service than a product. Many hemophilia activists are calling for a congressional investigation into the actions of the blood industry, the Food and Drug Administration that regulates it, and the National Hemophilia Foundation in failing to prevent contamination of the blood supply.
Shilts concludes. “The lost opportunities of 1982 would be explained later with the chorus: ‘How were we to know?’ This had no meaning in 1983. By then, vast numbers of people knew better, but confronted with knowledge and the chance to do something, they usually did the wrong thing, if they did anything at all. At the time, their postures seemed like the right thing to do in order to preserve civil rights or, say. the economic viability of the blood industry. The problem, of course, was that such considerations constantly overshadowed concerns of medicine and public health.”
Comments