 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

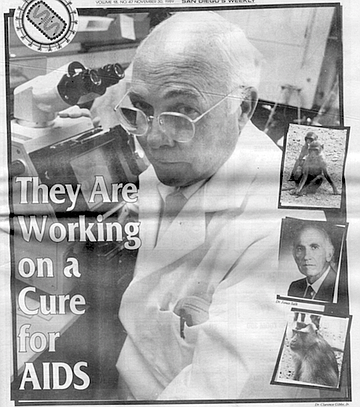
When you hear hoofbeats, think horses, not zebras, it’s an often-repeated med-school axiom that means consider the simple solution first. Dr. Clarence "Joe” Gibbs, Jr., a researcher at the National Institutes of Health (NIH), hears hoofbeats, and unlike many of his colleagues, he’s thinking horses.
Along with San Diego's Dr. Jonas Salk, the developer of the first successful polio vaccine, Gibbs is working on a vaccine to immunize against human immunodeficiency virus (HIV), the riddling parasite that causes AIDS and may already have infected more than one million people in the U.S. alone. In their work, Gibbs and Salk are not employing such post-Watson-and-Crick technologies as recombinant DNA, synthetic peptides, or anti idiotypes.

"Everybody wanted to rush in with recombinant (genetically engineered] vaccines here, there, and the other,” says Gibbs, who heads an infectious-disease lab at the NIH's Institute of Neurological and Communicative Disorders and Stroke in Bethesda, Maryland. "We took the classical approach."
That classical approach is to create a vaccine that contains "inactivated” or killed HIV. Salk used that approach when he developed the killed-poliovirus vaccine in the '50s. Preliminary studies on chimpanzees and humans suggest that the killed-HIV vaccine Gibbs and Salk are developing is one of the most promising strategies yet devised for stopping the virus before it ransacks the body.
An entire industry revolves around the design and testing of AIDS vaccines, an industry that one Wall Street analyst says potentially has a $974 million market. Gibbs and Salk are but two of hundreds of AIDS vaccine researchers. Their killed-HIV vaccine, a project of the San Diego-based Immune Response Corporation (IRC) — a company Salk co-founded — is but one of at least three dozen vaccine strategies being pursued. Still, the IRC vaccine is breaking away from the pack and helping to change the minds of pessimistic researchers who one year ago argued that, as a Washington Post headline put it, an AIDS vaccine may never work.
But the IRC vaccine has its share of detractors. "There's a lot of heartburn about what we're doing," says Gibbs.
While most researchers are working on vaccines to protect people not yet infected with HIV, IRC has set its sights on the HIV-infected population, calling its vaccine an "AIDS immunotherapeutic." The same post-infection vaccine strategy is used for hepatitis-B and rabies, both of which have a relatively long lag time between infection and the onset of symptoms. With AIDS, the lag time is an average of 7.8 years.
Only one scientific paper has been published about Salk's HIV research, a 1987 commentary by him that appeared in the British scientific journal Nature. The paper presents no data but meticulously spells out the theory behind a post-infection vaccine, insisting that if it prevented the symptoms of AIDS, the vaccine "would have a greater and more rapid impact in reducing HIV morbidity and mortality" than a vaccine for the uninfected population.
At the time of the Nature commentary, AIDS-vaccine researchers viewed Salk as a Johnny-come-lately to the AIDS field. "When Jonas showed up at (1987's Third International Conference on AIDS in Washington, D.C.) and presented his ideas, he was laughed out of the conference," says Dr. Brandon Fradd of Shearson Lehman Hutton, Inc, an M.D. who analyzes the AIDS-vaccine market for investors. But two years later, at the Fifth International AIDS Conference in Montreal this past June, Fradd says Salk and Gibbs "stole the show." "Research is inherently unpredictable," says Fradd.
The accelerating pace of research into a virus that was only identified five years ago has astonished even seasoned scientists. As swarms of researchers have rushed to publish each new picogram of information, HIV has become one of the best understood viruses on earth.
There's a colossal difference, though, between understanding a virus and stopping it from plundering a human body, so it would be foolhardy to predict when - or even if - a successful HIV vaccine will be added to the medical arsenal. But for Gibbs, Salk, and a handful of other AIDS-vaccine researchers, 1989 has proven to be a glowing year, and 1990 promises to be even brighter.
Joe Gibbs speaks like a sailor, cerebrates like a Thomist, and looks like a scientist. Which, as he might say, makes plenty of damn sense.
Gibbs joined the Navy in 1943 and served in World War II as a hospital corpsman on a heavy cruiser and then entered the reserves. By the time he retired his uniform in 1987, he had risen to the rank of captain and had served as a commanding officer five times. Gibbs, a disciple of St. Thomas Aquinas and an active Catholic, received his B.A. (biology/philosophy), M.A. (zoology/chemistry), and Ph.D. (microbiology, with minors in cytology, ecology, and chemistry) from Catholic University, in Washington, D.C.
"I've literally had three careers running simultaneously," says Gibbs of his Navy, church, and science work. "When people say, 'Why haven't you done this? Why haven't you done that?' I think, 'You bastards, all you've done is one thing.' " Unlike Jonas Salk, Gibbs - as with 99 percent of the world's scientists -still has his anonymity, though he is well known and respected among his colleagues.
Gibbs's father was a veterinarian who convinced his son that killed vaccines were better than live ones. "My father refused to use the attenuated (live) vaccine," says Gibbs. "His logic was simple: It might revert." (Attenuated viruses occasionally mutate back into a virulent form.)
"So I like killed vaccines," Gibbs says matter-of-fadly. "Because of that, I was interested in a possible killed vaccine for AIDS.”
Gibbs says he was killing a batch of HIV the day Jonas Salk first called him in February 1987. According to Gibbs (Salk, as is his policy, declined to be interviewed about his AIDS vaccine work), the conversation went like this:
"Joe, I have a putative vaccine," said Salk.
"For what?" asked Gibbs.
"HIV"
"It's not recombinant, I hope,” said Gibbs, adding that he didn't know why someone wasn't making a killed-virus vaccine.
Salk explained that he had fashioned just such a putative vaccine but needed chimpanzees to test it on.
"Jonas didn't have an animal to his name," says Gibbs, who had several chimpanzees. They decided to collaborate, and on April 15 of that year, Gibbs inoculated three chimpanzees with Salk's vaccine These animals were compared to a fourth "control" chimp, which was not given the vaccine.
"We didn’t waste any time," says Gibbs.
Forget Susan Sontag’s warning - war is an apt metaphor for AIDS. When a virus invades the body, the immune system calls out troops of antibodies and white blood cells to stop the enemy. Usually, the body wins the battle, and the immune system remembers - in some cases, for life - how to defeat the virus should it reinvade. But sometimes viruses overwhelm the immune system, causing disease. Scientists design vaccines to stage mock wars in the immune system. By attacking the body with a harmless foe, vaccines teach the immune system how to fight the real thing, should it later raid the body. Though one dose of some vaccines can protect for life, others require periodic "booster" doses to retrain the immune system's soldiers.
Human immunodeficiency virus is a devious, complex, quick-change artist that can live in the body for up to 15 years without causing disease. Once it gains the upper hand over the immune system, it opens the door for pneumonia, fungal infections, tuberculosis, chronic fevers, chronic diarrhea, cancer, wasting syndrome, and dementia. The U.S. AIDS body count now stands at 61,655. More than 100,000 Americans are HIV-infected and also have AIDS symptoms. Unless a medical breakthrough alters HIV's ways, scientists believe all of those infected will eventually succumb to complications associated with the disease.
To do its dirty work, HIV must finagle itself into a cell. The two types of cells it favors are macrophages and white blood cells called T4 lymphocytes. One of the reasons HIV is so devastating is that macrophages and T4 lymphocytes are front-line combatants in the immune system's army.
HIV is shaped like a sphere with mushrooms sprouting off it. The mushroom stems are glycoproteins, known scientifically as gp41, and the mushroom caps are called gpl20. The whole mushroom is referred to as gpl60. Because these glycoproteins are on the HIV outer membrane, they are called envelope proteins.
Once inside the bloodstream, HIV hunts for CD4, a protein that juts from the outer membrane of T4 lymphocytes and macrophages. CD4 and gpl20 (the "mushroom cap") snap together like pieces in a jigsaw puzzle. After CD4 and gpl20 embrace, gp41 (the "mushroom stem") springs out from under gpl20 and hooks the immune cell's membrane. HIV and the immune cell then fuse.
At this stage, HIV drops the bomb, injecting its core - made of proteins and two strands of RNA -inside the cell. The virus then weaves its genetic information into its host's DNA and can turn the cell into an HIV factory. One of the most ominous traits of HIV is that it can lie dormant inside the cell's DNA, hiding from the immune system.
AIDS vaccines have two missions: stop HIV from fusing with cells, and kill cells the virus has already infected. The most common vaccine battle plan is to block the union of the virus's caplike gpl20 structures and the immune cell's CD4. HIV-infected people naturally develop antibodies that latch onto gpl20, preventing CD4 from snapping into place, but eventually, the virus outnumbers the antibodies, and a cell becomes infected. Theoretically, a single such fusion can lead to AIDS.
Immunological science has devised three main types of vaccines: killed, live, and "subunit.” Killed vaccines are made by killing the virus with chemicals, heat, or light but leaving the shape of the virus intact. Live vaccines are made from weakened forms of the virus. Subunit vaccines are made from pieces of the virus. All three vaccines are teachers of immunologic warfare.
Because the weakened viruses in live vaccines can mutate back into potent viruses, no pharmaceutical company is developing a live HIV vaccine. Most every commercial vaccine developer is making a subunit type.
Northern California's Chiron Corporation and Ciba Geigy are co-developing a subunit vaccine composed of pieces of genetically engineered or synthetically made gpl20. The companies' goal is a vaccine that teaches the immune system to produce rapidly large amounts of gpl20 antibodies. Should the vaccinated person later encounter HIV, Chiron/Ciba Geigy expects the strong gpl20 antibody response to prevent HIV/immune cell fusion, effectively slamming the door in HIV's face.
Repligen Corporation in Cambridge, Massachusetts, and the pharmaceutical house Merck Sharp & Dohme are jointly developing another gpl20 subunit vaccine. Seattle-based Oncogen, a division of Bristol-Myers Co., is working on a similar vaccine that exploits gpl60. Connecticut's MicroGeneSys, Inc., also is fabricating a gpl60 vaccine.
But these subunit vaccines have a flaw: The genes that code for gpl20 and gpl60 mutate frequently, meaning there are hundreds of different strains of these glycoproteins. Because an antibody to one strain may not work on a different strain, a vaccine made from one strain of gpl20, for example, may not prevent cell/HIV fusion if another strain of gpl20 shows up. And fusion equals death.
Dr. Scott Putney, head of molecular biology at Repligen, explains that a part of gpl20 called the loop varies little from strain to strain. "We think the loop is it," says Putney. Repligen has found that there are three predominant variations of the loop, and it hopes that mixing them together into a vaccine cocktail will produce a panoplied antibody response. "I have much higher enthusiasm now than a year ago," says Putney.
Dr. Dino Dina, chief virologist at Chiron, says his company has recently found "conserved" regions of gpl20 that don't vary much from strain to strain. "I think the data emerging from our lab and Repligen/ Merck about the number of prevalent strains is encouraging," says Dina. "I'm very optimistic about it. Perhaps we can protect 80 or 90 percent of the people. That's really quite acceptable."
At the Southwest Foundation for Biomedical Research in San Antonio, Texas, Dr. Ronald Kennedy is marching to the beat of the immune cells' CD4. Kennedy, who's allied with drug manufacturer Becton Dickinson, reasons that if he can flood the body with a substance that looks like CD4, he can fool gpl20 into binding with the impostor, leaving the CD4-studded immune cells as stout as ever.
Kennedy manufactures his fake CD4 by first locating antibodies to CD4. He then raises a population of antibodies to these CD4 antibodies. These antiantibodies are called anti idiotypes and have a shape similar to CD4’s. "People think I'm in left field," says Kennedy. "I’ve certainly got colleagues who think it's absolute bullshit."
An anti idiotype AIDS vaccine, admits Kennedy, may take longer to perfect than other approaches. "But as long as it’s the best and it works," he says, "well...."
Joining Kennedy in left field is AIDS researcher Dr. Allan Goldstein, chairman of the biochemistry department of George Washington University, Washington, D.C. "We proposed a radically different approach," Goldstein surmises, "and we ran into a lot of static." Goldstein's subunit vaccine, called HGP-30 and funded by the D.C.-based Viral Technologies, Inc., uses a protein inside the virus rather than one from its surface, or envelope.
"I've always felt going after the envelope protein is an exercise in futility," says Goldstein. "There are so many different strains. It constantly keeps changing. How are you going to make a vaccine?" By contrast, the internal protein Goldstein's banking on (pl7) is highly conserved from strain to strain.
What’s more, he explains, envelope proteins primarily trigger an antibody response — antibodies that block the fusion of HIV and immune cells. Internal proteins primarily marshal troops of killer cells that selectively attack HIV-infected cells. Eliciting these killer cells, argues Goldstein, "is the most relevant component in an effective vaccine."
Because HGP-30 targets infected cells, Goldstein posits that, like IRC's vaccine, it might prevent the onset of AIDS in HIV-infected people. He believes it might somehow protect the uninfected population as well.
"The herd mentality has been to develop 'envelope' approaches to vaccines," says Goldstein. "I think what you'll see in the next year is that the 'envelope' people will say they're wrong, and they'll include internal proteins in their vaccines." (Connecticut's MicroGeneSys, which has centered its research on gpl60, is now doing just that.)
We may also see companies leaving the AIDS-vaccine business altogether. San Francisco's Genentech recently dropped its gpl20-vaccine project to work on a drug to treat AIDS instead. "At first, people thought an AIDS vaccine would be a cinch," says company spokesman Jack Murphy. "I suppose we thought that too. But it's just not so."
When Gibbs and Salk began, they planned to test a vaccine made from whole, killed HIV. But, says Gibbs, "What happened was - much to our surprise - on the manufacture of this vaccine, we stripped off the outer envelope of the virus. It was happenstance. That was not planned. Now it appears to us that envelope proteins do not contribute very much to protection."
This is particularly true when protection is defined as preventing an HIV-infected person from developing AIDS symptoms. One of the markers of an HIV infection progressing into full-blown AIDS is that antibodies to the HIV core proteins drop sharply and HIV levels rise. But antibodies to the HIV envelope proteins persist. This could mean - and Salk and Gibbs certainly hope it does - that maintaining high levels of antibodies to core proteins might be a key to thwarting AIDS.
Whatever the theory, Goldstein says at the Montreal AIDS conference this summer, Gibbs and Salk startled colleagues with their chimp data. "They have made all of the 'envelope’ groups very, very nervous," says Goldstein. "I couldn't be happier."
Before vaccines are evaluated in humans, researchers examine what those vaccines do in test tubes and animals. But there's a bottleneck with AIDS vaccines because scientists have yet to discover a good animal model in which to conduct their tests.
The predominant type of HIV in this country infects only humans and chimpanzees. Chimps and man have virtually identical immune systems; and while chimps can contract the HIV virus, no chimp has ever developed AIDS symptoms. Further hampering researchers is the fact that chimps are scarce because they are a threatened species; according to Dr. Jorg Eichberg, the head veterinarian at Texas’ Southwest Foundation, there are a paltry 1200 chimps in the country available for research, and each one costs thousands of dollars.
"The use of chimpanzees is so tightly controlled by the U.S. Public Health Service that it's unbelievable," says Gibbs. "Jane Goodall would go around in circles the minute you use a chimp."
In Gibbs's provocative study, he injected only three chimps with the killed-HIV vaccine. Experimentally speaking, this is a small sample size, and it has led some to criticize the data. "Be happy, brother, that I got it into three chimps," says Gibbs. "I also snuck in a control [chimp]."
The standard method of testing a vaccine is to inoculate an uninfected ("naive") animal and then challenge it with an injection of potent virus. If the vaccine works, the animal should wipe out the invader before it gets a foothold.
Because the IRC vaccine is designed as a postinfection vaccine, Gibbs inoculated two HIV-infected chimps with the vaccine. The third chimp he inoculated was naive. In the two previously infected chimps, HIV disappeared.
Gibbs then challenged all three chimps with an injection of HIV. During the past eight months, Gibbs has bled the animals once every two weeks. He has not found any HIV in the previously infected chimps. And though the naive chimp became infected, it appears that the IRC vaccine is helping the animal slowly knock out the virus.
"I was surprised," says Gibbs of the three chimps' responses. "It certainly panned out very well."
Gibbs, not Salk, presented the findings in Montreal. "I said, 'Here's the data, here's my interpretation of the results - take it, leave it, I don't care,’" says Gibbs. "In contrast, Jonas would have gone into all sorts of details, and people would have lost sight of what works."
Gibbs, for one, is thrilled with the early success. As for Salk, Gibbs says, "He's walking on cloud nine right now. This is his last hurrah." Gibbs says they are currently writing up the data they presented in Montreal and plan to submit it for publication in the next few weeks.
Only three other U.S. research groups have publicly revealed that they have inoculated chimps with vaccines and then challenged them with HIV. All three were subunit vaccines made from envelope proteins. All three failed to protect the animals.
One vaccine was Genentech's, the San Francisco company that has since scuttled its AIDS-vaccine project. Another was developed at the Frederick Cancer Research Facility, a branch of the National Cancer Institute in Frederick, Maryland. Dr. Larry Arthur, who heads the AIDS vaccine group at Frederick, says he still has hope for an envelope protein vaccine if it is made differently, and he plans to challenge chimps again next year. "With a virus that can integrate into the host's DNA, you'd like to prevent initial infection," says Arthur. "But other proteins definitely, definitely should be looked at."
Arthur says Gibbs and Salk’s findings are "really important’' and ventures that "maybe not enough people are incorporating both envelope and core proteins."
The third challenge that failed was with the vaccine made by Seattle’s Oncogen.
Veterinarian Jorg Eichberg, who has tested 13 different AIDS vaccines in chimps - more than anyone else in the world - conducted the Oncogen and Genentech challenges. Data from many of these experiments have not been publicly discussed, and he shies away from specifics, other than to say no vaccine has offered protection. Eichberg points out that Gibbs and Salk actually challenged only one animal -the naive chimp. And he's suspicious of the data from the previously infected animals.
"It's too good to be true," says Eichberg, who plans to repeat the experiment. "Nobody believes it."
Many vaccine developers react coolly when asked about Gibbs and Salk's work. MicroGeneSys President Frank Volvovitz’s response is typical: "We really haven’t been able to see much data coming out of the group in a scientific forum or publication." Still, the two researchers certainly have their believers. And many are primate experts.
Dr. Michael Murphey-Corb, a vaccine investigator at the Delta Regional Primate Center in Covington, Louisiana, calls Salk and Gibbs's work "a notable finding.” That's not to say she thinks they have the answer. "I have this fear of making too much of work," says Murphey-Corb. "I don't think we're ever going to see one major thing that says this is it. There are single steps in science, and (Gibbs and Salk) have made a step."
Murphey-Corb knows from where she speaks. She is a developer of a killed vaccine for simian immunodeficiency virus (SIV), a close relative of HIV that causes an AIDS-like disease in rhesus and pigtail macaque monkeys. As Murphey-Corb points out, "One can predict that what works in rhesus monkeys with SIV will work in humans with HIV."
Because macaques are plentiful in the wild and breed well in captivity - Murphey-Corb has 200 -they are an ideal testing ground for vaccine theories. She doesn't want to discuss the details of her early findings other than to say they are "encouraging rather than discouraging."
The climate is right, she says, to explore the venerable killed-virus approach. "It was reasonable at the time to start with the envelope glycoproteins. It was reasonably safe. There were good scientific reasons why it should work. But it didn't work -none of the chimps have been protected — and we shouldn't belabor the point. We should dig in our heels and start at the beginning. Let's just erase the blackboard."
Murphey-Corb, who's now collaborating with Salk on some experiments, says her colleagues still slag the killed-vaccine approach. "I'm running into a lot of resistance to my work,” she says, adding that she commiserated with Salk when he visited her lab recently. "He patted me on the back and kissed me on the cheek and said, 'I have paid dearly for proving them wrong.'"
Another animal researcher who unabashedly believes in Gibbs’ and Salk's work is Dr. Murray Gardner, a virology professor at the University of California, Davis, which has a primate center of its own. “I share (their) enthusiasm for killed-virus vaccines," says Gardner, who is testing SIV vaccines in macaques and has inoculated some animals for SaJk.
The costs of vaccine production, Gardner suggests, are driving research. "The economics of recombinant engineering make it easier to make big batches of vaccine," he says. "The cost of preparing killed vaccine the old-fashioned way is so expensive. And then they're all worried about litigation."
Over the years, many drug companies have stopped making vaccines because of liability lawsuits. Gardner says researchers fear a replay of the "Cutter incident," in which Cutter Laboratories failed to kill all of the poliovirus in a batch of killed-poliovirus vaccine it made in 1955. The catastrophic result was the death or crippling of more than 260 children. Although Cutter - not Salk's killed-vaccine recipe -was responsible for the accident, a stigma was attached to the killed-vaccine's reputation and to Salk's. "Salk has had to re-live that thing a billion times,” Gardner says.
Questions about that vaccine's safety, in part, led to the U.S. government's 1963 declaration that it was no longer the polio "vaccine of choice." It is rarely used in this country today, a reality Salk has relentlessly fought to change.
Several researchers working on subunit and antiidiotype vaccines, which pose no risk of causing the disease they're trying to prevent, say they don't trust the killed-virus approach. Gibbs has heard it all before. According to Gibbs, he has been shooed away from the project by no less an investigator than Dr. Robert Gallo, the NIH scientist who first identified HIV in this country and an influential vaccine researcher. "Gallo will still say, 'Joe, why are you making a vaccine that will never be approved?'" says Gibbs. Gallo did not return repeated phone calls.
Gibbs sloughs off the criticism, noting that the HIV in the IRC vaccine is killed twice, first chemically (with betapropiolactone) and then with irradiation. It's also tested for live virus before it is injected. "I envision this ultimately as being one of the vaccines used to stop AIDS," says Gibbs. "Whether it will stand alone or be used with another chemotherapeutic agent, I don't know."
Dr. Janet Woodcock, director of the U.S. Food and Drug Administration's (FDA) Biologies Investigational New Drugs Division - the group that sanctions new vaccine clinical trials - assures that the government has no a priori prejudice against a killed-HIV vaccine. "We've approved a lot of very serious pathogens that are inactivated," she says. "That's basically where it's at for eradication of several diseases."
Though UC-Davis's Gardner supports the killed-vaccine approach, he doesn't dismiss genetic engineering. "It's an abling technology," he says. "But hell, we re only 15 years into the recombinant DNA era." (And it has already paid off in other areas: Genetically engineered human insulin and growth hormone are both commercially available.) Making an AIDS vaccine, says Gardner, "is a hell of a problem." But he's optimistic. "Singles, not home runs, are going to win it - with a lot of foul balls."
Curiously, Dr. Ronald Desrosiers, the first SIV-vaccine researcher to successfully protect animals from that virus and publish his findings, is a resolute skeptic. "I have hope, but 1 have my doubts that we're ever going to make a vaccine," says Desrosiers, whose August paper in the Proceedings of the National Academy of Sciences described how his killed-SIV vaccine protected six monkeys from the disease. As with Murphey-Corb’s killed-SIV vaccine, Desrosiers's contains whole virus, meaning it has both envelope and core proteins.
"I don't think an inactivated, whole-virus vaccine is going to be practical in humans," says Desrosiers. "It doesn't give a sustained, high level of antibody protection. And once HIV gets its foot in the door, it's going to get you.”
Desrosiers, with uncommon candor for a scientist, calls his experiments "highly artificial," explaining that he did everything he could - without cheating -to arrive at positive results. "It's highly unlikely that there's any chance in hell it would work in the real world,” he says.
Gibbs is abrupt when asked about Desrosiers's pessimism. "My point is that what we have presented supports the use of an inactivated vaccine," he says. "Murphey-Corb's data supports our observations. And like it or not like it, Desrosiers's supports our observations."
On September 13 this year, the privately held Immune Response Corporation -which has been largely funded by the multinational pharmaceutical Rorer Group, Inc., and by the Colgate-Palmolive Company - went public with a stock offering. The 59-page prospectus filed by the company with the SEC reveals more details about the IRC vaccine than anything previously published. (A company spokeswoman promised to arrange an interview with an IRC principal and then did not return several phone calls.)
The IRC vaccine is one of seven vaccines tested in human beings so far. Because every new drug runs the risk of harming people, all of these clinical trials are still attempting to determine whether the vaccine in question is safe, not whether it works.
From the drug manufacturer’s point of view, the FDA’s new drug approval process is an exhausting, time-consuming obstacle course that often dead ends. To date, MicroGeneSys and Oncogen are the only companies that have FDA approval to test their vaccines in humans in the U.S. Both of these vaccines have been tested at six vaccine evaluation units set up around the country by the National Institute of Allergy and Infectious Diseases. Humans have received other AIDS vaccines in European and African tests.
Thanks to a 1940 state law, the California Department of Health Services Food and Drug Branch can authorize clinical trials of new drugs within its borders. In November 1987, University o£ Southern California researcher Dr. Alexandra Levine began a trial with the IRC vaccine that would eventually include 19 HIV-infected people who had early AIDS symptoms. "At one year into these studies, 16 of the 19 patients stabilized their T4 cell count [the lymphocytes that HIV targets and that also help kill HIV-infected cells] and showed no additional signs of infection," states the SEC filing. One patient recorded a drop in T4 cells but did not develop any AIDS symptoms. According to the SEC filing, "These results have been sustained." The other two patients both developed pronounced AIDS symptoms.
Levine's next trial had even more dramatic results. The trial began in July 1988 with 54 HIV-infected people who showed no symptoms of AIDS. Because HIV can hide in cells, infected people may not always have the virus swimming around in their blood. Still, HIV in the blood is a good indicator of the severity of an infection. At the beginning of Levine's 54-person trial, 93 percent of the participants had HIV in their blood.
One half of the participants were immunized with the IRC vaccine; the other half, the controls, did not receive the vaccine. Six months into the study, reports the SEC filing, 36 percent of the immunized group tested negative for the virus compared to 13 percent of the nonimmunized group. In other words, the immune systems of people inoculated with the vaccine were nearly three times as likely to have cleared the blood of HIV.
The control participants were given the vaccine at this point. "As of August 1989,” states the SEC filing, ”85 percent of the immunized subjects (including subsequently immunized control subjects) had developed enhanced immunity to HIV." Only one participant had developed AIDS symptoms, and one other had a drop in T4 cells but no symptoms. Though the data are exciting, this does not mean the IRC vaccine works, especially when you fold in the fact that HIV on average does not cause disease for nearly eight years.
Scant data are available from other clinical trials, and what's been publicly revealed is more informative than inspiring. "Most of what I've seen in human trials is leading nowhere," says Fradd of Shearson Lehman Hutton.
MicroGeneSys has reported that its gpl60 vaccine, the first to receive FDA approval for clinical trials, is safe and produces immune responses in both uninfected gay and bisexual men and men and women from low-risk groups. These immune responses may well be too weak and HIV-strain specific to offer any real protection from infection. More damning still, there's no evidence that antibodies to gpl60 can prevent an HIV infection in chimpanzees.
Oncogen's FDA-approved gpl60 vaccine trial in 30 uninfected people had results similar to MicroGene-Sys's, but these data could be even less significant. The Oncogen vaccine is made by placing the genes for gpl60 inside live vaccinia virus, the agent once used in the smallpox vaccine. It appears that the only people who respond immunologically to the Oncogen vaccine are those who have never been vaccinated for smallpox. Their immune systems apparently are fighting the vaccinia virus rather than the gpl60 infection.
At the Montreal conference, MicroGeneSys and Bristol-Myers/Oncogen announced that they plan to begin a joint clinical trial, giving people who've received the Oncogen vaccine booster shots of MicroGeneSys's preparation.
Testing vaccines on humans without first demonstrating effectiveness in chimps has been hotly debated and criticized. MicroGeneSys out-and-out skipped the chimpanzee challenge test. (MicroGeneSys President Volvovitz declines to discuss details of his company's vaccine work.) Oncogen held chimp challenges that failed. A principal Oncogen investigator did not return phone calls.
Dr. Harold McClure, who is chief of pathology and immunology at the Yerkes Regional Primate Center in Atlanta and worked on the failed chimp challenge, says he is baffled that Oncogen is conducting human trials. "Rather than moving to human clinical trials in vaccines we know don't work," McClure says, "we should be using animal models to test other vaccines. I don’t think you'll find anyone in the country who'll say we should be testing those vaccines." Even the sober Committee for the Oversight of AIDS Activities, a branch of the National Academy of Sciences' Institute of Medicine, has reproached the trials as premature.
The FDA's Woodcock says the government must evaluate vaccines differently when a good animal model doesn't exist. "I've had this discussion many times," she says, stressing that the two FDA-approved trials involve low-risk vaccines. Her conclusion: "Unless you ask questions and do comparisons, you can't learn.”
Wall Street analyst Fradd chokes on the official line. "Historically, it’s bizarre," he says of the MicroGeneSys trial. "Tb be honest with you, I think they made a mistake. I think what they did was human experimentation, and I think they made a whole hullabaloo over nothing." He's less charitable toward Oncogen, which went on to human trials even though its vaccine failed a chimp challenge.
The FDA approvals, charges Fradd, were politically motivated. "There was a lot of pressure on the FDA to do something," he says, "and the FDA knew it could argue that there was no clear animal model to test this sort of thing."
Gibbs also rejects the idea of human trials before challenging chimps. "Not one drop of this stuff [the IRC vaccine] went into a human in California until after it had been evaluated in chimps," he says. "So we knew that there was no reason to suspect any untoward reaction."
Chiron/Ciba Geigy, Viral Technologies, and the Southwest Foundation/Becton Dickinson are either preparing to or have already begun human tests of their vaccines in Europe. The preliminary results are, at best, similar to those of MicroGeneSys and Oncogen.
The first AIDS vaccine ever tested in humans was developed by France’s Dr. Daniel Zagury. In high scientific tradition. Zagury and a colleague injected themselves in 1986 before administering the gpl60 vaccine to ten Zaireans. It, too, has proven safe and elicits an immune response.
Of all the AIDS vaccines now being developed, Shearson's Fradd has the most faith in the Repligen/Merck gpl20 candidate. And not, he notes, because his brokerage house has handled a public offering of Repligen stock. "Merck is a class-one research organization, and they have taken a rigorous approach," says Fradd. "At each step, they have a clear indication that they should go on to the next stage."'
In addition to finding a snip of gpl20 that doesn't vary much from strain to strain, Repligen/Merck has yielded impressive results from a novel chimp study. After injecting the vaccine into chimps, researchers extracted antibodies, mixed them with live HIV, and then injected that combination into chimps. The chimps did not get infected. Though this is not as important a test as a challenge, it indicates that the antibodies elicited by the vaccine neutralized HIV and prevented infection. Repligen/Merck intends to challenge vaccinated chimps in the next few months and proceed to human trials if warranted.
Fradd, who has co-authored two investor's guides analyzing the AIDS-vaccine market, also likes the work of George Washington University's Allan Goldstein ("a strong contender in the race to develop an effective vaccine") and Gibbs and Salk. "The chimp results that [IRC] came up with were truly astounding,” says Fradd.
Following the 1988 international conference on AIDS held in Stockholm, the Washington Post reported that "there were no major advances reported in vaccine research, and the general consensus among scientists is that progress is not being made any faster than expected." In 1989 several advances were reported in vaccine research, and the general consensus among scientists is that progress is being made at a steady clip.
And the year's not over. A few weeks ago, researchers at the University of Washington's Regional Primate Research Center reported that they had successfully vaccinated macaques against SAID-D, an AIDS-like disease caused by a virus more distant from HIV than SIV. The genetically engineered vaccine, which was made by Oncogen, relied on envelope proteins.
In the next few months, a Vienna, Virginia biomedical firm intends to start marketing a New Zealand white rabbit that can be infected with HIV and develops symptoms. Many researchers are suspicious of the rabbit model; but if it works, HIV research will advance more quickly, costs will drop, and the FDA will have a better way to evaluate AIDS vaccines before they are injected into humans.
IRC is currently waiting on FDA approval to begin the largest clinical trial yet. This proposed 650-person study, which IRC requested approval for in August, would evaluate its vaccine's efficacy. According to the company's SEC filing, all of the subjects would be HIV-infected and have early disease symptoms. The plans call for this placebo-controlled nationwide trial to last three years and to be double-blind (neither the patients nor the clinicians know who is receiving the real vaccine). All participants would concurrently take AZT so that the study “will not encounter ethical issues associated with keeping test subjects from what would then be an approved drug."
IRC is also asking the FDA to approve a one-year trial in healthier HIV-infected people who would not need to take AZT. IRC hopes to begin both trials before the end of the year.
Gibbs says he and Salk expect that they'll soon revaccinate some new HIV-iniected chimps.
Many scientists have lived their whole lives developing a vaccine, never to find the magic bullet. Still, they take shots in the dark - calculated shots in the dark - and, step by difficult step, knowledge accrues. Maybe Gibbs and Salk are testing what one day will be heralded as having stopped HIV. Maybe they're not. Maybe it will be only one of several AIDS vaccines. Maybe it will be completely forgotten about, just one more bullet fired in a war. Gibbs is keeping his feet on the ground. "So far, ours is the only one that shows protective efficacy,” he says. "But in this business, you never know who's going to lurch ahead."
La Jolla's Immune Response Corporation, known primarily for its sponsorship of Jonas Salk's AIDS vaccine research, wants to sell its stock to the public. Federal law forbids companies with such pending offerings from talking about its work, and although the stock issue failed on its first try last month when not enough buyers lined up for 3 million shares priced at Sll to $13 each, IRC apparently hopes to try again.
Company executives like Dennis Carlo, IRC's research director, who already owns 480,000 shares of common stock in IRC, which he purchased from the company for $13,000, might make a huge profit if the stock catches fire on Wall Street. IRC co-founder and director Jonas Salk made a similar arrangement, and he and his family also stand to benefit substantially from any market windfall. Anything that interferes with a successful stock offering could be extremely costly to both men as well as to the other company executives and private investors who provided money to start IRC, and so they have remained silent.
Wall Street's rejection of the IRC issue is not news for many other small, San Diego-based companies that have pinned their hopes for developing new vaccines and other revolutionary medical treatments on our increased understanding of how cells regulate themselves at the molecular level. "Although there are a lot of companies in San Diego, they are very small," notes stock market analyst Brandon Fradd, a medical doctor employed by Shearson Lehman Hutton. "Their technology is very good, but it is very difficult to get products from it."
In addition to spending years developing the basic science needed to understand how cells interact with each other, intensive testing of the final product in animals and humans must be conducted. "It takes 10 to 12 years from conception of idea to approval time before the drug even gets on the market," Fradd says.
"You can't plan this stuff. You get to phase II, and suddeniy the drug gets canned due to a life-threatening reaction." Larger companies can spread this risk over many products, he notes.
Of the IRC stock, Fradd says: "It's a high-risk issue but not a sham. They may just wait another six months and do it again." Last month, Chugai, a large Japanese pharmaceutical manufacturer, agreed to buy all the shares of GentProbe, a La Jolla biotech firm that develops genetically engineered molecular "probes" to detect infectious diseases. That is unlikely with IRC, says Fradd. "I would be very surprised if somebody came in and took the company over straight out. Japanese would be unlikely to take on a high-risk research company. There isn't much AIDS in Japan, so they aren't going to buy an AIDS company."
In material prepared for its recent public stock offering, IRC claimed that it may be ready by late next year for the first phases of human clinical trials of a multiple sclerosis vaccine being developed by IRC researcher Dr. Steve Brostoff. The same general concept might also be applied to other diseases linked to the body's attack upon itself, including rheumatoid arthritis and a type of diabetes suffered by more than a million Americans.
Wall Street analyst Fradd, however, remains cautious. "The concept seems reasonable," he says. "I think there are a number of companies looking at this... [but] the stock still looked a little expensive to me."


When you hear hoofbeats, think horses, not zebras, it’s an often-repeated med-school axiom that means consider the simple solution first. Dr. Clarence "Joe” Gibbs, Jr., a researcher at the National Institutes of Health (NIH), hears hoofbeats, and unlike many of his colleagues, he’s thinking horses.
Along with San Diego's Dr. Jonas Salk, the developer of the first successful polio vaccine, Gibbs is working on a vaccine to immunize against human immunodeficiency virus (HIV), the riddling parasite that causes AIDS and may already have infected more than one million people in the U.S. alone. In their work, Gibbs and Salk are not employing such post-Watson-and-Crick technologies as recombinant DNA, synthetic peptides, or anti idiotypes.

"Everybody wanted to rush in with recombinant (genetically engineered] vaccines here, there, and the other,” says Gibbs, who heads an infectious-disease lab at the NIH's Institute of Neurological and Communicative Disorders and Stroke in Bethesda, Maryland. "We took the classical approach."
That classical approach is to create a vaccine that contains "inactivated” or killed HIV. Salk used that approach when he developed the killed-poliovirus vaccine in the '50s. Preliminary studies on chimpanzees and humans suggest that the killed-HIV vaccine Gibbs and Salk are developing is one of the most promising strategies yet devised for stopping the virus before it ransacks the body.
An entire industry revolves around the design and testing of AIDS vaccines, an industry that one Wall Street analyst says potentially has a $974 million market. Gibbs and Salk are but two of hundreds of AIDS vaccine researchers. Their killed-HIV vaccine, a project of the San Diego-based Immune Response Corporation (IRC) — a company Salk co-founded — is but one of at least three dozen vaccine strategies being pursued. Still, the IRC vaccine is breaking away from the pack and helping to change the minds of pessimistic researchers who one year ago argued that, as a Washington Post headline put it, an AIDS vaccine may never work.
But the IRC vaccine has its share of detractors. "There's a lot of heartburn about what we're doing," says Gibbs.
While most researchers are working on vaccines to protect people not yet infected with HIV, IRC has set its sights on the HIV-infected population, calling its vaccine an "AIDS immunotherapeutic." The same post-infection vaccine strategy is used for hepatitis-B and rabies, both of which have a relatively long lag time between infection and the onset of symptoms. With AIDS, the lag time is an average of 7.8 years.
Only one scientific paper has been published about Salk's HIV research, a 1987 commentary by him that appeared in the British scientific journal Nature. The paper presents no data but meticulously spells out the theory behind a post-infection vaccine, insisting that if it prevented the symptoms of AIDS, the vaccine "would have a greater and more rapid impact in reducing HIV morbidity and mortality" than a vaccine for the uninfected population.
At the time of the Nature commentary, AIDS-vaccine researchers viewed Salk as a Johnny-come-lately to the AIDS field. "When Jonas showed up at (1987's Third International Conference on AIDS in Washington, D.C.) and presented his ideas, he was laughed out of the conference," says Dr. Brandon Fradd of Shearson Lehman Hutton, Inc, an M.D. who analyzes the AIDS-vaccine market for investors. But two years later, at the Fifth International AIDS Conference in Montreal this past June, Fradd says Salk and Gibbs "stole the show." "Research is inherently unpredictable," says Fradd.
The accelerating pace of research into a virus that was only identified five years ago has astonished even seasoned scientists. As swarms of researchers have rushed to publish each new picogram of information, HIV has become one of the best understood viruses on earth.
There's a colossal difference, though, between understanding a virus and stopping it from plundering a human body, so it would be foolhardy to predict when - or even if - a successful HIV vaccine will be added to the medical arsenal. But for Gibbs, Salk, and a handful of other AIDS-vaccine researchers, 1989 has proven to be a glowing year, and 1990 promises to be even brighter.
Joe Gibbs speaks like a sailor, cerebrates like a Thomist, and looks like a scientist. Which, as he might say, makes plenty of damn sense.
Gibbs joined the Navy in 1943 and served in World War II as a hospital corpsman on a heavy cruiser and then entered the reserves. By the time he retired his uniform in 1987, he had risen to the rank of captain and had served as a commanding officer five times. Gibbs, a disciple of St. Thomas Aquinas and an active Catholic, received his B.A. (biology/philosophy), M.A. (zoology/chemistry), and Ph.D. (microbiology, with minors in cytology, ecology, and chemistry) from Catholic University, in Washington, D.C.
"I've literally had three careers running simultaneously," says Gibbs of his Navy, church, and science work. "When people say, 'Why haven't you done this? Why haven't you done that?' I think, 'You bastards, all you've done is one thing.' " Unlike Jonas Salk, Gibbs - as with 99 percent of the world's scientists -still has his anonymity, though he is well known and respected among his colleagues.
Gibbs's father was a veterinarian who convinced his son that killed vaccines were better than live ones. "My father refused to use the attenuated (live) vaccine," says Gibbs. "His logic was simple: It might revert." (Attenuated viruses occasionally mutate back into a virulent form.)
"So I like killed vaccines," Gibbs says matter-of-fadly. "Because of that, I was interested in a possible killed vaccine for AIDS.”
Gibbs says he was killing a batch of HIV the day Jonas Salk first called him in February 1987. According to Gibbs (Salk, as is his policy, declined to be interviewed about his AIDS vaccine work), the conversation went like this:
"Joe, I have a putative vaccine," said Salk.
"For what?" asked Gibbs.
"HIV"
"It's not recombinant, I hope,” said Gibbs, adding that he didn't know why someone wasn't making a killed-virus vaccine.
Salk explained that he had fashioned just such a putative vaccine but needed chimpanzees to test it on.
"Jonas didn't have an animal to his name," says Gibbs, who had several chimpanzees. They decided to collaborate, and on April 15 of that year, Gibbs inoculated three chimpanzees with Salk's vaccine These animals were compared to a fourth "control" chimp, which was not given the vaccine.
"We didn’t waste any time," says Gibbs.
Forget Susan Sontag’s warning - war is an apt metaphor for AIDS. When a virus invades the body, the immune system calls out troops of antibodies and white blood cells to stop the enemy. Usually, the body wins the battle, and the immune system remembers - in some cases, for life - how to defeat the virus should it reinvade. But sometimes viruses overwhelm the immune system, causing disease. Scientists design vaccines to stage mock wars in the immune system. By attacking the body with a harmless foe, vaccines teach the immune system how to fight the real thing, should it later raid the body. Though one dose of some vaccines can protect for life, others require periodic "booster" doses to retrain the immune system's soldiers.
Human immunodeficiency virus is a devious, complex, quick-change artist that can live in the body for up to 15 years without causing disease. Once it gains the upper hand over the immune system, it opens the door for pneumonia, fungal infections, tuberculosis, chronic fevers, chronic diarrhea, cancer, wasting syndrome, and dementia. The U.S. AIDS body count now stands at 61,655. More than 100,000 Americans are HIV-infected and also have AIDS symptoms. Unless a medical breakthrough alters HIV's ways, scientists believe all of those infected will eventually succumb to complications associated with the disease.
To do its dirty work, HIV must finagle itself into a cell. The two types of cells it favors are macrophages and white blood cells called T4 lymphocytes. One of the reasons HIV is so devastating is that macrophages and T4 lymphocytes are front-line combatants in the immune system's army.
HIV is shaped like a sphere with mushrooms sprouting off it. The mushroom stems are glycoproteins, known scientifically as gp41, and the mushroom caps are called gpl20. The whole mushroom is referred to as gpl60. Because these glycoproteins are on the HIV outer membrane, they are called envelope proteins.
Once inside the bloodstream, HIV hunts for CD4, a protein that juts from the outer membrane of T4 lymphocytes and macrophages. CD4 and gpl20 (the "mushroom cap") snap together like pieces in a jigsaw puzzle. After CD4 and gpl20 embrace, gp41 (the "mushroom stem") springs out from under gpl20 and hooks the immune cell's membrane. HIV and the immune cell then fuse.
At this stage, HIV drops the bomb, injecting its core - made of proteins and two strands of RNA -inside the cell. The virus then weaves its genetic information into its host's DNA and can turn the cell into an HIV factory. One of the most ominous traits of HIV is that it can lie dormant inside the cell's DNA, hiding from the immune system.
AIDS vaccines have two missions: stop HIV from fusing with cells, and kill cells the virus has already infected. The most common vaccine battle plan is to block the union of the virus's caplike gpl20 structures and the immune cell's CD4. HIV-infected people naturally develop antibodies that latch onto gpl20, preventing CD4 from snapping into place, but eventually, the virus outnumbers the antibodies, and a cell becomes infected. Theoretically, a single such fusion can lead to AIDS.
Immunological science has devised three main types of vaccines: killed, live, and "subunit.” Killed vaccines are made by killing the virus with chemicals, heat, or light but leaving the shape of the virus intact. Live vaccines are made from weakened forms of the virus. Subunit vaccines are made from pieces of the virus. All three vaccines are teachers of immunologic warfare.
Because the weakened viruses in live vaccines can mutate back into potent viruses, no pharmaceutical company is developing a live HIV vaccine. Most every commercial vaccine developer is making a subunit type.
Northern California's Chiron Corporation and Ciba Geigy are co-developing a subunit vaccine composed of pieces of genetically engineered or synthetically made gpl20. The companies' goal is a vaccine that teaches the immune system to produce rapidly large amounts of gpl20 antibodies. Should the vaccinated person later encounter HIV, Chiron/Ciba Geigy expects the strong gpl20 antibody response to prevent HIV/immune cell fusion, effectively slamming the door in HIV's face.
Repligen Corporation in Cambridge, Massachusetts, and the pharmaceutical house Merck Sharp & Dohme are jointly developing another gpl20 subunit vaccine. Seattle-based Oncogen, a division of Bristol-Myers Co., is working on a similar vaccine that exploits gpl60. Connecticut's MicroGeneSys, Inc., also is fabricating a gpl60 vaccine.
But these subunit vaccines have a flaw: The genes that code for gpl20 and gpl60 mutate frequently, meaning there are hundreds of different strains of these glycoproteins. Because an antibody to one strain may not work on a different strain, a vaccine made from one strain of gpl20, for example, may not prevent cell/HIV fusion if another strain of gpl20 shows up. And fusion equals death.
Dr. Scott Putney, head of molecular biology at Repligen, explains that a part of gpl20 called the loop varies little from strain to strain. "We think the loop is it," says Putney. Repligen has found that there are three predominant variations of the loop, and it hopes that mixing them together into a vaccine cocktail will produce a panoplied antibody response. "I have much higher enthusiasm now than a year ago," says Putney.
Dr. Dino Dina, chief virologist at Chiron, says his company has recently found "conserved" regions of gpl20 that don't vary much from strain to strain. "I think the data emerging from our lab and Repligen/ Merck about the number of prevalent strains is encouraging," says Dina. "I'm very optimistic about it. Perhaps we can protect 80 or 90 percent of the people. That's really quite acceptable."
At the Southwest Foundation for Biomedical Research in San Antonio, Texas, Dr. Ronald Kennedy is marching to the beat of the immune cells' CD4. Kennedy, who's allied with drug manufacturer Becton Dickinson, reasons that if he can flood the body with a substance that looks like CD4, he can fool gpl20 into binding with the impostor, leaving the CD4-studded immune cells as stout as ever.
Kennedy manufactures his fake CD4 by first locating antibodies to CD4. He then raises a population of antibodies to these CD4 antibodies. These antiantibodies are called anti idiotypes and have a shape similar to CD4’s. "People think I'm in left field," says Kennedy. "I’ve certainly got colleagues who think it's absolute bullshit."
An anti idiotype AIDS vaccine, admits Kennedy, may take longer to perfect than other approaches. "But as long as it’s the best and it works," he says, "well...."
Joining Kennedy in left field is AIDS researcher Dr. Allan Goldstein, chairman of the biochemistry department of George Washington University, Washington, D.C. "We proposed a radically different approach," Goldstein surmises, "and we ran into a lot of static." Goldstein's subunit vaccine, called HGP-30 and funded by the D.C.-based Viral Technologies, Inc., uses a protein inside the virus rather than one from its surface, or envelope.
"I've always felt going after the envelope protein is an exercise in futility," says Goldstein. "There are so many different strains. It constantly keeps changing. How are you going to make a vaccine?" By contrast, the internal protein Goldstein's banking on (pl7) is highly conserved from strain to strain.
What’s more, he explains, envelope proteins primarily trigger an antibody response — antibodies that block the fusion of HIV and immune cells. Internal proteins primarily marshal troops of killer cells that selectively attack HIV-infected cells. Eliciting these killer cells, argues Goldstein, "is the most relevant component in an effective vaccine."
Because HGP-30 targets infected cells, Goldstein posits that, like IRC's vaccine, it might prevent the onset of AIDS in HIV-infected people. He believes it might somehow protect the uninfected population as well.
"The herd mentality has been to develop 'envelope' approaches to vaccines," says Goldstein. "I think what you'll see in the next year is that the 'envelope' people will say they're wrong, and they'll include internal proteins in their vaccines." (Connecticut's MicroGeneSys, which has centered its research on gpl60, is now doing just that.)
We may also see companies leaving the AIDS-vaccine business altogether. San Francisco's Genentech recently dropped its gpl20-vaccine project to work on a drug to treat AIDS instead. "At first, people thought an AIDS vaccine would be a cinch," says company spokesman Jack Murphy. "I suppose we thought that too. But it's just not so."
When Gibbs and Salk began, they planned to test a vaccine made from whole, killed HIV. But, says Gibbs, "What happened was - much to our surprise - on the manufacture of this vaccine, we stripped off the outer envelope of the virus. It was happenstance. That was not planned. Now it appears to us that envelope proteins do not contribute very much to protection."
This is particularly true when protection is defined as preventing an HIV-infected person from developing AIDS symptoms. One of the markers of an HIV infection progressing into full-blown AIDS is that antibodies to the HIV core proteins drop sharply and HIV levels rise. But antibodies to the HIV envelope proteins persist. This could mean - and Salk and Gibbs certainly hope it does - that maintaining high levels of antibodies to core proteins might be a key to thwarting AIDS.
Whatever the theory, Goldstein says at the Montreal AIDS conference this summer, Gibbs and Salk startled colleagues with their chimp data. "They have made all of the 'envelope’ groups very, very nervous," says Goldstein. "I couldn't be happier."
Before vaccines are evaluated in humans, researchers examine what those vaccines do in test tubes and animals. But there's a bottleneck with AIDS vaccines because scientists have yet to discover a good animal model in which to conduct their tests.
The predominant type of HIV in this country infects only humans and chimpanzees. Chimps and man have virtually identical immune systems; and while chimps can contract the HIV virus, no chimp has ever developed AIDS symptoms. Further hampering researchers is the fact that chimps are scarce because they are a threatened species; according to Dr. Jorg Eichberg, the head veterinarian at Texas’ Southwest Foundation, there are a paltry 1200 chimps in the country available for research, and each one costs thousands of dollars.
"The use of chimpanzees is so tightly controlled by the U.S. Public Health Service that it's unbelievable," says Gibbs. "Jane Goodall would go around in circles the minute you use a chimp."
In Gibbs's provocative study, he injected only three chimps with the killed-HIV vaccine. Experimentally speaking, this is a small sample size, and it has led some to criticize the data. "Be happy, brother, that I got it into three chimps," says Gibbs. "I also snuck in a control [chimp]."
The standard method of testing a vaccine is to inoculate an uninfected ("naive") animal and then challenge it with an injection of potent virus. If the vaccine works, the animal should wipe out the invader before it gets a foothold.
Because the IRC vaccine is designed as a postinfection vaccine, Gibbs inoculated two HIV-infected chimps with the vaccine. The third chimp he inoculated was naive. In the two previously infected chimps, HIV disappeared.
Gibbs then challenged all three chimps with an injection of HIV. During the past eight months, Gibbs has bled the animals once every two weeks. He has not found any HIV in the previously infected chimps. And though the naive chimp became infected, it appears that the IRC vaccine is helping the animal slowly knock out the virus.
"I was surprised," says Gibbs of the three chimps' responses. "It certainly panned out very well."
Gibbs, not Salk, presented the findings in Montreal. "I said, 'Here's the data, here's my interpretation of the results - take it, leave it, I don't care,’" says Gibbs. "In contrast, Jonas would have gone into all sorts of details, and people would have lost sight of what works."
Gibbs, for one, is thrilled with the early success. As for Salk, Gibbs says, "He's walking on cloud nine right now. This is his last hurrah." Gibbs says they are currently writing up the data they presented in Montreal and plan to submit it for publication in the next few weeks.
Only three other U.S. research groups have publicly revealed that they have inoculated chimps with vaccines and then challenged them with HIV. All three were subunit vaccines made from envelope proteins. All three failed to protect the animals.
One vaccine was Genentech's, the San Francisco company that has since scuttled its AIDS-vaccine project. Another was developed at the Frederick Cancer Research Facility, a branch of the National Cancer Institute in Frederick, Maryland. Dr. Larry Arthur, who heads the AIDS vaccine group at Frederick, says he still has hope for an envelope protein vaccine if it is made differently, and he plans to challenge chimps again next year. "With a virus that can integrate into the host's DNA, you'd like to prevent initial infection," says Arthur. "But other proteins definitely, definitely should be looked at."
Arthur says Gibbs and Salk’s findings are "really important’' and ventures that "maybe not enough people are incorporating both envelope and core proteins."
The third challenge that failed was with the vaccine made by Seattle’s Oncogen.
Veterinarian Jorg Eichberg, who has tested 13 different AIDS vaccines in chimps - more than anyone else in the world - conducted the Oncogen and Genentech challenges. Data from many of these experiments have not been publicly discussed, and he shies away from specifics, other than to say no vaccine has offered protection. Eichberg points out that Gibbs and Salk actually challenged only one animal -the naive chimp. And he's suspicious of the data from the previously infected animals.
"It's too good to be true," says Eichberg, who plans to repeat the experiment. "Nobody believes it."
Many vaccine developers react coolly when asked about Gibbs and Salk's work. MicroGeneSys President Frank Volvovitz’s response is typical: "We really haven’t been able to see much data coming out of the group in a scientific forum or publication." Still, the two researchers certainly have their believers. And many are primate experts.
Dr. Michael Murphey-Corb, a vaccine investigator at the Delta Regional Primate Center in Covington, Louisiana, calls Salk and Gibbs's work "a notable finding.” That's not to say she thinks they have the answer. "I have this fear of making too much of work," says Murphey-Corb. "I don't think we're ever going to see one major thing that says this is it. There are single steps in science, and (Gibbs and Salk) have made a step."
Murphey-Corb knows from where she speaks. She is a developer of a killed vaccine for simian immunodeficiency virus (SIV), a close relative of HIV that causes an AIDS-like disease in rhesus and pigtail macaque monkeys. As Murphey-Corb points out, "One can predict that what works in rhesus monkeys with SIV will work in humans with HIV."
Because macaques are plentiful in the wild and breed well in captivity - Murphey-Corb has 200 -they are an ideal testing ground for vaccine theories. She doesn't want to discuss the details of her early findings other than to say they are "encouraging rather than discouraging."
The climate is right, she says, to explore the venerable killed-virus approach. "It was reasonable at the time to start with the envelope glycoproteins. It was reasonably safe. There were good scientific reasons why it should work. But it didn't work -none of the chimps have been protected — and we shouldn't belabor the point. We should dig in our heels and start at the beginning. Let's just erase the blackboard."
Murphey-Corb, who's now collaborating with Salk on some experiments, says her colleagues still slag the killed-vaccine approach. "I'm running into a lot of resistance to my work,” she says, adding that she commiserated with Salk when he visited her lab recently. "He patted me on the back and kissed me on the cheek and said, 'I have paid dearly for proving them wrong.'"
Another animal researcher who unabashedly believes in Gibbs’ and Salk's work is Dr. Murray Gardner, a virology professor at the University of California, Davis, which has a primate center of its own. “I share (their) enthusiasm for killed-virus vaccines," says Gardner, who is testing SIV vaccines in macaques and has inoculated some animals for SaJk.
The costs of vaccine production, Gardner suggests, are driving research. "The economics of recombinant engineering make it easier to make big batches of vaccine," he says. "The cost of preparing killed vaccine the old-fashioned way is so expensive. And then they're all worried about litigation."
Over the years, many drug companies have stopped making vaccines because of liability lawsuits. Gardner says researchers fear a replay of the "Cutter incident," in which Cutter Laboratories failed to kill all of the poliovirus in a batch of killed-poliovirus vaccine it made in 1955. The catastrophic result was the death or crippling of more than 260 children. Although Cutter - not Salk's killed-vaccine recipe -was responsible for the accident, a stigma was attached to the killed-vaccine's reputation and to Salk's. "Salk has had to re-live that thing a billion times,” Gardner says.
Questions about that vaccine's safety, in part, led to the U.S. government's 1963 declaration that it was no longer the polio "vaccine of choice." It is rarely used in this country today, a reality Salk has relentlessly fought to change.
Several researchers working on subunit and antiidiotype vaccines, which pose no risk of causing the disease they're trying to prevent, say they don't trust the killed-virus approach. Gibbs has heard it all before. According to Gibbs, he has been shooed away from the project by no less an investigator than Dr. Robert Gallo, the NIH scientist who first identified HIV in this country and an influential vaccine researcher. "Gallo will still say, 'Joe, why are you making a vaccine that will never be approved?'" says Gibbs. Gallo did not return repeated phone calls.
Gibbs sloughs off the criticism, noting that the HIV in the IRC vaccine is killed twice, first chemically (with betapropiolactone) and then with irradiation. It's also tested for live virus before it is injected. "I envision this ultimately as being one of the vaccines used to stop AIDS," says Gibbs. "Whether it will stand alone or be used with another chemotherapeutic agent, I don't know."
Dr. Janet Woodcock, director of the U.S. Food and Drug Administration's (FDA) Biologies Investigational New Drugs Division - the group that sanctions new vaccine clinical trials - assures that the government has no a priori prejudice against a killed-HIV vaccine. "We've approved a lot of very serious pathogens that are inactivated," she says. "That's basically where it's at for eradication of several diseases."
Though UC-Davis's Gardner supports the killed-vaccine approach, he doesn't dismiss genetic engineering. "It's an abling technology," he says. "But hell, we re only 15 years into the recombinant DNA era." (And it has already paid off in other areas: Genetically engineered human insulin and growth hormone are both commercially available.) Making an AIDS vaccine, says Gardner, "is a hell of a problem." But he's optimistic. "Singles, not home runs, are going to win it - with a lot of foul balls."
Curiously, Dr. Ronald Desrosiers, the first SIV-vaccine researcher to successfully protect animals from that virus and publish his findings, is a resolute skeptic. "I have hope, but 1 have my doubts that we're ever going to make a vaccine," says Desrosiers, whose August paper in the Proceedings of the National Academy of Sciences described how his killed-SIV vaccine protected six monkeys from the disease. As with Murphey-Corb’s killed-SIV vaccine, Desrosiers's contains whole virus, meaning it has both envelope and core proteins.
"I don't think an inactivated, whole-virus vaccine is going to be practical in humans," says Desrosiers. "It doesn't give a sustained, high level of antibody protection. And once HIV gets its foot in the door, it's going to get you.”
Desrosiers, with uncommon candor for a scientist, calls his experiments "highly artificial," explaining that he did everything he could - without cheating -to arrive at positive results. "It's highly unlikely that there's any chance in hell it would work in the real world,” he says.
Gibbs is abrupt when asked about Desrosiers's pessimism. "My point is that what we have presented supports the use of an inactivated vaccine," he says. "Murphey-Corb's data supports our observations. And like it or not like it, Desrosiers's supports our observations."
On September 13 this year, the privately held Immune Response Corporation -which has been largely funded by the multinational pharmaceutical Rorer Group, Inc., and by the Colgate-Palmolive Company - went public with a stock offering. The 59-page prospectus filed by the company with the SEC reveals more details about the IRC vaccine than anything previously published. (A company spokeswoman promised to arrange an interview with an IRC principal and then did not return several phone calls.)
The IRC vaccine is one of seven vaccines tested in human beings so far. Because every new drug runs the risk of harming people, all of these clinical trials are still attempting to determine whether the vaccine in question is safe, not whether it works.
From the drug manufacturer’s point of view, the FDA’s new drug approval process is an exhausting, time-consuming obstacle course that often dead ends. To date, MicroGeneSys and Oncogen are the only companies that have FDA approval to test their vaccines in humans in the U.S. Both of these vaccines have been tested at six vaccine evaluation units set up around the country by the National Institute of Allergy and Infectious Diseases. Humans have received other AIDS vaccines in European and African tests.
Thanks to a 1940 state law, the California Department of Health Services Food and Drug Branch can authorize clinical trials of new drugs within its borders. In November 1987, University o£ Southern California researcher Dr. Alexandra Levine began a trial with the IRC vaccine that would eventually include 19 HIV-infected people who had early AIDS symptoms. "At one year into these studies, 16 of the 19 patients stabilized their T4 cell count [the lymphocytes that HIV targets and that also help kill HIV-infected cells] and showed no additional signs of infection," states the SEC filing. One patient recorded a drop in T4 cells but did not develop any AIDS symptoms. According to the SEC filing, "These results have been sustained." The other two patients both developed pronounced AIDS symptoms.
Levine's next trial had even more dramatic results. The trial began in July 1988 with 54 HIV-infected people who showed no symptoms of AIDS. Because HIV can hide in cells, infected people may not always have the virus swimming around in their blood. Still, HIV in the blood is a good indicator of the severity of an infection. At the beginning of Levine's 54-person trial, 93 percent of the participants had HIV in their blood.
One half of the participants were immunized with the IRC vaccine; the other half, the controls, did not receive the vaccine. Six months into the study, reports the SEC filing, 36 percent of the immunized group tested negative for the virus compared to 13 percent of the nonimmunized group. In other words, the immune systems of people inoculated with the vaccine were nearly three times as likely to have cleared the blood of HIV.
The control participants were given the vaccine at this point. "As of August 1989,” states the SEC filing, ”85 percent of the immunized subjects (including subsequently immunized control subjects) had developed enhanced immunity to HIV." Only one participant had developed AIDS symptoms, and one other had a drop in T4 cells but no symptoms. Though the data are exciting, this does not mean the IRC vaccine works, especially when you fold in the fact that HIV on average does not cause disease for nearly eight years.
Scant data are available from other clinical trials, and what's been publicly revealed is more informative than inspiring. "Most of what I've seen in human trials is leading nowhere," says Fradd of Shearson Lehman Hutton.
MicroGeneSys has reported that its gpl60 vaccine, the first to receive FDA approval for clinical trials, is safe and produces immune responses in both uninfected gay and bisexual men and men and women from low-risk groups. These immune responses may well be too weak and HIV-strain specific to offer any real protection from infection. More damning still, there's no evidence that antibodies to gpl60 can prevent an HIV infection in chimpanzees.
Oncogen's FDA-approved gpl60 vaccine trial in 30 uninfected people had results similar to MicroGene-Sys's, but these data could be even less significant. The Oncogen vaccine is made by placing the genes for gpl60 inside live vaccinia virus, the agent once used in the smallpox vaccine. It appears that the only people who respond immunologically to the Oncogen vaccine are those who have never been vaccinated for smallpox. Their immune systems apparently are fighting the vaccinia virus rather than the gpl60 infection.
At the Montreal conference, MicroGeneSys and Bristol-Myers/Oncogen announced that they plan to begin a joint clinical trial, giving people who've received the Oncogen vaccine booster shots of MicroGeneSys's preparation.
Testing vaccines on humans without first demonstrating effectiveness in chimps has been hotly debated and criticized. MicroGeneSys out-and-out skipped the chimpanzee challenge test. (MicroGeneSys President Volvovitz declines to discuss details of his company's vaccine work.) Oncogen held chimp challenges that failed. A principal Oncogen investigator did not return phone calls.
Dr. Harold McClure, who is chief of pathology and immunology at the Yerkes Regional Primate Center in Atlanta and worked on the failed chimp challenge, says he is baffled that Oncogen is conducting human trials. "Rather than moving to human clinical trials in vaccines we know don't work," McClure says, "we should be using animal models to test other vaccines. I don’t think you'll find anyone in the country who'll say we should be testing those vaccines." Even the sober Committee for the Oversight of AIDS Activities, a branch of the National Academy of Sciences' Institute of Medicine, has reproached the trials as premature.
The FDA's Woodcock says the government must evaluate vaccines differently when a good animal model doesn't exist. "I've had this discussion many times," she says, stressing that the two FDA-approved trials involve low-risk vaccines. Her conclusion: "Unless you ask questions and do comparisons, you can't learn.”
Wall Street analyst Fradd chokes on the official line. "Historically, it’s bizarre," he says of the MicroGeneSys trial. "Tb be honest with you, I think they made a mistake. I think what they did was human experimentation, and I think they made a whole hullabaloo over nothing." He's less charitable toward Oncogen, which went on to human trials even though its vaccine failed a chimp challenge.
The FDA approvals, charges Fradd, were politically motivated. "There was a lot of pressure on the FDA to do something," he says, "and the FDA knew it could argue that there was no clear animal model to test this sort of thing."
Gibbs also rejects the idea of human trials before challenging chimps. "Not one drop of this stuff [the IRC vaccine] went into a human in California until after it had been evaluated in chimps," he says. "So we knew that there was no reason to suspect any untoward reaction."
Chiron/Ciba Geigy, Viral Technologies, and the Southwest Foundation/Becton Dickinson are either preparing to or have already begun human tests of their vaccines in Europe. The preliminary results are, at best, similar to those of MicroGeneSys and Oncogen.
The first AIDS vaccine ever tested in humans was developed by France’s Dr. Daniel Zagury. In high scientific tradition. Zagury and a colleague injected themselves in 1986 before administering the gpl60 vaccine to ten Zaireans. It, too, has proven safe and elicits an immune response.
Of all the AIDS vaccines now being developed, Shearson's Fradd has the most faith in the Repligen/Merck gpl20 candidate. And not, he notes, because his brokerage house has handled a public offering of Repligen stock. "Merck is a class-one research organization, and they have taken a rigorous approach," says Fradd. "At each step, they have a clear indication that they should go on to the next stage."'
In addition to finding a snip of gpl20 that doesn't vary much from strain to strain, Repligen/Merck has yielded impressive results from a novel chimp study. After injecting the vaccine into chimps, researchers extracted antibodies, mixed them with live HIV, and then injected that combination into chimps. The chimps did not get infected. Though this is not as important a test as a challenge, it indicates that the antibodies elicited by the vaccine neutralized HIV and prevented infection. Repligen/Merck intends to challenge vaccinated chimps in the next few months and proceed to human trials if warranted.
Fradd, who has co-authored two investor's guides analyzing the AIDS-vaccine market, also likes the work of George Washington University's Allan Goldstein ("a strong contender in the race to develop an effective vaccine") and Gibbs and Salk. "The chimp results that [IRC] came up with were truly astounding,” says Fradd.
Following the 1988 international conference on AIDS held in Stockholm, the Washington Post reported that "there were no major advances reported in vaccine research, and the general consensus among scientists is that progress is not being made any faster than expected." In 1989 several advances were reported in vaccine research, and the general consensus among scientists is that progress is being made at a steady clip.
And the year's not over. A few weeks ago, researchers at the University of Washington's Regional Primate Research Center reported that they had successfully vaccinated macaques against SAID-D, an AIDS-like disease caused by a virus more distant from HIV than SIV. The genetically engineered vaccine, which was made by Oncogen, relied on envelope proteins.
In the next few months, a Vienna, Virginia biomedical firm intends to start marketing a New Zealand white rabbit that can be infected with HIV and develops symptoms. Many researchers are suspicious of the rabbit model; but if it works, HIV research will advance more quickly, costs will drop, and the FDA will have a better way to evaluate AIDS vaccines before they are injected into humans.
IRC is currently waiting on FDA approval to begin the largest clinical trial yet. This proposed 650-person study, which IRC requested approval for in August, would evaluate its vaccine's efficacy. According to the company's SEC filing, all of the subjects would be HIV-infected and have early disease symptoms. The plans call for this placebo-controlled nationwide trial to last three years and to be double-blind (neither the patients nor the clinicians know who is receiving the real vaccine). All participants would concurrently take AZT so that the study “will not encounter ethical issues associated with keeping test subjects from what would then be an approved drug."
IRC is also asking the FDA to approve a one-year trial in healthier HIV-infected people who would not need to take AZT. IRC hopes to begin both trials before the end of the year.
Gibbs says he and Salk expect that they'll soon revaccinate some new HIV-iniected chimps.
Many scientists have lived their whole lives developing a vaccine, never to find the magic bullet. Still, they take shots in the dark - calculated shots in the dark - and, step by difficult step, knowledge accrues. Maybe Gibbs and Salk are testing what one day will be heralded as having stopped HIV. Maybe they're not. Maybe it will be only one of several AIDS vaccines. Maybe it will be completely forgotten about, just one more bullet fired in a war. Gibbs is keeping his feet on the ground. "So far, ours is the only one that shows protective efficacy,” he says. "But in this business, you never know who's going to lurch ahead."
La Jolla's Immune Response Corporation, known primarily for its sponsorship of Jonas Salk's AIDS vaccine research, wants to sell its stock to the public. Federal law forbids companies with such pending offerings from talking about its work, and although the stock issue failed on its first try last month when not enough buyers lined up for 3 million shares priced at Sll to $13 each, IRC apparently hopes to try again.
Company executives like Dennis Carlo, IRC's research director, who already owns 480,000 shares of common stock in IRC, which he purchased from the company for $13,000, might make a huge profit if the stock catches fire on Wall Street. IRC co-founder and director Jonas Salk made a similar arrangement, and he and his family also stand to benefit substantially from any market windfall. Anything that interferes with a successful stock offering could be extremely costly to both men as well as to the other company executives and private investors who provided money to start IRC, and so they have remained silent.
Wall Street's rejection of the IRC issue is not news for many other small, San Diego-based companies that have pinned their hopes for developing new vaccines and other revolutionary medical treatments on our increased understanding of how cells regulate themselves at the molecular level. "Although there are a lot of companies in San Diego, they are very small," notes stock market analyst Brandon Fradd, a medical doctor employed by Shearson Lehman Hutton. "Their technology is very good, but it is very difficult to get products from it."
In addition to spending years developing the basic science needed to understand how cells interact with each other, intensive testing of the final product in animals and humans must be conducted. "It takes 10 to 12 years from conception of idea to approval time before the drug even gets on the market," Fradd says.
"You can't plan this stuff. You get to phase II, and suddeniy the drug gets canned due to a life-threatening reaction." Larger companies can spread this risk over many products, he notes.
Of the IRC stock, Fradd says: "It's a high-risk issue but not a sham. They may just wait another six months and do it again." Last month, Chugai, a large Japanese pharmaceutical manufacturer, agreed to buy all the shares of GentProbe, a La Jolla biotech firm that develops genetically engineered molecular "probes" to detect infectious diseases. That is unlikely with IRC, says Fradd. "I would be very surprised if somebody came in and took the company over straight out. Japanese would be unlikely to take on a high-risk research company. There isn't much AIDS in Japan, so they aren't going to buy an AIDS company."
In material prepared for its recent public stock offering, IRC claimed that it may be ready by late next year for the first phases of human clinical trials of a multiple sclerosis vaccine being developed by IRC researcher Dr. Steve Brostoff. The same general concept might also be applied to other diseases linked to the body's attack upon itself, including rheumatoid arthritis and a type of diabetes suffered by more than a million Americans.
Wall Street analyst Fradd, however, remains cautious. "The concept seems reasonable," he says. "I think there are a number of companies looking at this... [but] the stock still looked a little expensive to me."
Comments