 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
Ed Guzman usually divides death three ways: in beds, in cars, and in alleys. In the beds are the old, in cars the unlucky or irresponsible, in alleys the victims. There are, of course, other divisions, other places to die. Guzman could tell you about those, too. In fact, he could spend all day and all night just telling you a few things he’s noticed about death.
But death occupies only a small part of Guzman’s job as a paramedic. Most of the time, he deals with hurt and confusion. He will tell you about a motorcyclist who scraped off his skin in a skid. He was drunk, Guzman says. No helmet, no shirt. No sympathy. Or the old woman who called an ambulance because she felt poorly and couldn’t afford to go to the doctor. She wasn’t really sick, just scared and lonely. Here, compassion lowers his voice.
He’s got this annoying answer for people who ask him what he did at work today. Same old thing, he says, grinning. Saving lives.
“This was a few months ago, in September or something like that,” Guzman recalls. “This poor girl was sixteen years old, driving her car along the transition ramp from Highway 94 to the southbound 805. For some unknown reason, she lost control of her car, it overturned, and she was thrown out of it. Then another car came along. The driver saw the car, but not the girl in the road. He swerved to miss the car and saw the girl. He swerved again but couldn’t avoid her and overturned his car, too. He didn’t get hurt because he was wearing seatbelts, but the girl had ex-" tensive injuries. Ah geez, she broke almost every bone in her body. She suffered massive head injuries, internal injuries.
“She was in ICU for something like two months, and six months in the hospital altogether. No one really expected her to live, and if she did, everyone expected her to be nothing more than a vegetable. Yet little by little, after suffering all sorts of complications in the hospital like pneumonia, she finally got better. She was discharged just two weeks ago. She had suffered some neurological damage, but she was walking and talking. That was a pretty miraculous recovery. You just have to picture somebody being run over by a two- or three-thousand-pound car and that’s exactly what she looked like. She was squashed. She looked, ah, I can’t even describe it. She just looked so bad. I thought we were going through the motions. I thought she was going to die for sure. But she didn’t. She made it.
“I visited her several times while she was in a coma. When she came out of the coma, they moved her upstairs and I didn’t go up to visit her, so she actually never knew who I was and neither did her family. But yet, I kept an eye on her. I was curious. It was a happy ending, and so many times in something like that we see people who are either not that bad or death is imminent and it’s so very rare that you can actually rip someone from the jaws of death. In her case we did, literally. We, along with everybody else in the hospital, saved her life. She lived to walk out. It was the classic reward of the job. ”
Guzman admits the “classic rewards’’ don’t come very often. “As you begin to work, you realize pretty quickly that only a small part of the calls are true emergencies, the kind people always imagine. Usually they’re something less, but we try to treat everyone like it’s an emergency. Sometimes it’s pretty hard. I can lose my temper with the chronic callers — the widows or widowers — the people who are lonely. They’ll call because they don’t want to be alone at night. They may have some small problem that during the day they can handle. At night, however, when it’s quiet, the problem just gets too big.
“At three in the morning, when you’ve already been out on three calls since midnight and you’re very tired and you recognize the address when the call comes in, you can very easily lose your temper and self-control. The immediate impulse is to lash out at the person who called, but as these things work out, the people who are clironic callers are usually in bad health and you know that one day they’re going to have a real emergency ... so you always treat them as an emergency. ”
More often, however, the calls are mundane, the same things over and over again. They vary only in the different parts of the city. In Southeast San Diego and Logan Heights, it’s beatings and stabbings. Downtown, it’s drunken alcoholic seizures. In Point Loma, heart attacks. And in Ocean Beach, where Guzman works now, it’s drug overdoses. In every part of the city, there is a kind of call that is predominant. The best places to work, Guzman says, are the busy places. Point Loma may have a lot of nice houses and people, but there just isn’t much business out there. Southeast San Diego is poor and sometimes a very scary place. But there, Guzman got to work a lot, seeing calls he just wouldn’t see in a wealthy area where people take better care of themselves.
Most of us have jobs that require making decisions. Very few of us, however, have to make any involving — literally — somebody else’s life. Guzman does and he loves it. “It can be exciting, although it’s certainly not always exciting. There’s a large percentage of ego involved; to say I do it just to help people is too altruistic. It’s more honest for me to say I became a paramedic to have the opportunity to make decisions, to take action to save a life or relieve suffering, saying that feeds the ego a little more.
“Paramedics have a certain arrogance about their professional lives. They are very sure of themselves, almost to a fault. Within about five minutes, they have to walk into a situation, gather an impression, and make decisions, often in adverse conditions, though they have to treat patients as if they’re in a quiet hospital room. There’s a smugness about how they deliver the patient. It’s a common experience among paramedics waiting in the emergency room after bringing in a patient to see nurses and doctors running around in confusion when a patient walks in. It’s kind of amusing.”
At the scene of an accident or injury, a paramedic is usually welcomed as something of a savior. Doctors may save more lives, but they don’t do it with everybody watching. On the street, the paramedic is better than a doctor. “What paramedics have is concentrated training to handle a few specific life-threatening emergencies. In those areas, there’s no doubt in my mind that a paramedic is better able to handle those few emergencies than a doctor. It’s because we have specialized training in a few specialized areas. We aren’t supposed to know all about medicine, only a handful of life-threatening emergencies and immediate, direct intervention.”
On a warm, sunny day in December, a young girl fights for her life in the waters of San Diego Bay near Ballast Point. Above her, white cotton clouds billow to cover a blue sky. Below, a smaller cloud spreads slowly away from the girl, darkening the water to a deeper, rustier shade of gray. Inside this cloud of blood, the girl struggles, one arm thrashing to stay afloat, the other dangling at her side, connected to her body only by ragged tendons and tattered flesh.
Moments before, she had been perched on the bow of a motorboat, sunning herself and enjoying the bouncing ride. Then the boat angled through a wave awkwardly, jerking the bow and the girl into the air. She fell forward into the water, and the boat raced on and caught her in its propeller. Numbly, she can feel her panicked friends pulling her into the boat and laying her gently on the deck. There seems to be blood everywhere, but she feels no pain. She talks to her friends while the boat speeds for shore.
When the call came in, Guzman was lolling around doing nothing in particular. It was one of those days when the calls are infrequent and un-momentous. There was time for a big call, the kind all paramedics like in a weird sort of way. The young girl was that kind of call.
“The call didn’t come in as a drowning. It came in over the alarm system as a stabbing. When we arrived at the harbor patrol, I saw this girl lying on the lawn in front of the office. She had a lot of obvious trauma to her — chest trauma and a three-quarter amputation of her arm at the shoulder. We were unable to tell how internal her injuries were. She was pulseless and abneic, that is, her heart wasn’t beating and she wasn’t breathing. We found out about the boating accident. Apparently she had been talking, communicating with people until she got progressively drowsier and lapsed into unconsciousness. She wasn’t bleeding when we got to her, but she had bled in the water and on the way in. It’s hard to tell how much blood she lost in the water, everything gets so distorted. But by the mechanism of injury, I was assuming her state of cardiac arrest was brought about by excessive hemorrhage. We started to do an I.V. Well, we attempted an I.V., but actually she was so vascularly collapsed that it was impossible to establish a line. Her veins had collapsed because she didn’t have any blood in them.
“So we took her to the hospital and when we got there, the doctor took over. There was some question about the doctor being led to believe — not by us but by his staff or his own impressions — that she was just a simple drowning. He could see her injuries, but because they weren’t bleeding profusely and because he didn’t have a clear picture of how they had occurred, it didn’t enter the doctor’s mind that she wasn’t simply a drowning victim. It’s possible to believe this because it’s possible to suffer an amputated arm without bleeding to death. Her injuries were isolated and she wasn’t bleeding. You can’t really say that’s a terrible thing if you’re a physician and you see only one of these things in your lifetime. He continued on his treatment for drowning for over an hour until she expired. The bottom line is that the autopsy revealed she had exsanguinated her entire blood contents. It’s not so much the controversy of her drowning. The doctor was right: she had suffered a salt-water drowning. Her drowning alone was probably enough to kill her. And the injury alone was certainly enough to kill her. The two together probably made her nonsalvageable, even with aggressive care. ’’
The language Guzman uses, the calm, clinical way he can describe a call, makes him seen unfeeling. Phrases like chest trauma, mechanism of injury, nonsalvageable are simply decorum. “It’s the way doctors talk, the way nurses talk. It’s the way we talk. It’s the only language we have to describe something. Maybe it helps us to remain detached. We can say, ‘Well, the mechanism of injury was such that we suspect internal injuries,’ or we could say, ‘She slammed her chest into the steering wheel and bent it back.’ It saves us from being so graphic.’’
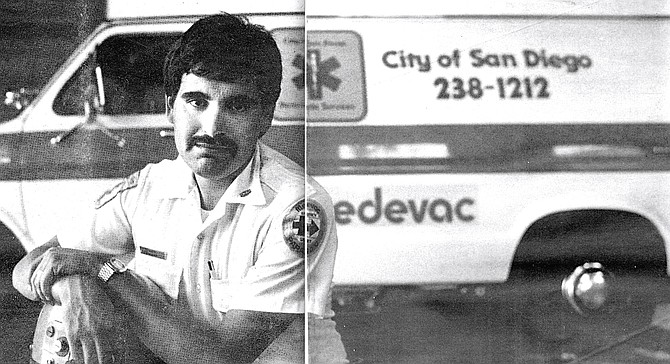
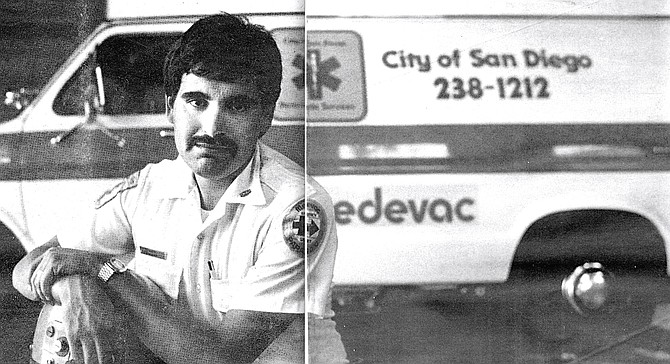
When Guzman smiles, his twenty-six-year-old face — mustachioed and slightly cherubic — becomes a portrait of compassionate tolerance and mild good humor. Anger, disgust, hurt are emotions that rarely show, although certainly he feels them. The girl’s death still bothers him because she was so young and beautiful; it seems so pointless. “There’s more of a feeling of helplessness, more frustration, when these kind of things happen to somebody young. That’s not to say that all people don’t deserve the best care, but it always seems to be such a terrible waste and shame when tragedies occur with somebody young. Paramedics are more affected when it happens to the young than they are when it happens to an older person. You relate more to patients your own age. Not so much in a freak boat accident where you might exercise better judgment than she did sitting in the front of the boat like that. You would hope you know better. It’s the things you know you can’t control, like for example, when you see young people injured in auto accidents. Nobody thinks it will ever happen to them, but every paramedic has got stories of young people they’ve seen get killed. The car crashes they’ve had nothing to do with, minding their own business driving down the road.
“It’s a funny thing about first reactions. I myself have two speeds: slow and fast. You make that initial impression of how serious your patient is, whether you can go slowly at a nice, easy pace or very fast because a lot has to be done because somebody’s life or limb may hang in the balance. When I saw the young girl on the lawn, I switched into the fast mode. In cases like that, I don’t usually see the patient’s face until well into the run. I see it, but I don’t look at it. It wasn’t until well into the run to the hospital that I could see what she looked like. That’s when it starts getting hard. When I’m working fast, the patient’s very anonymous. You can detach yourself. But when you get to the hospital and the family arrives behind you and there’s a name associated with the patient, you can look at the patient and watch the scenario unfold.
“I rarely get so upset I can’t function. It’s only happened about twice in my career. Yet I’ll still get moved, have bouts of depression and anger. Different things affect me. I remember one case when I wasn’t even involved. I was working overtime at the hospital. The paramedics brought in this little old woman. She and her husband — they must have been as old as the hills — in their seventies or eighties. They had been married for eons. Anyway, they were walking, jaywalking across the street and weren’t paying attention. It was dark and a driver didn’t see them and his car hit the woman and broke her hip, her leg, and some internal injuries. Injuries that to you and me wouldn’t be fatal by any means — they would lay us up, but we wouldn’t die. It’s not the same with an old person. I remember watching them work on her in the emergency room and they were working very hard. They worked for hours on her, but she died. I remember watching her die. I was as upset then as I have ever been. I felt so sorry for her and her husband waiting outside.”
Guzman pauses, dark eyes glistening behind tinted glasses, then goes on. ‘‘Because I was the ‘tech’ [technician] on duty, I had to see him, talk to him. He was trying to make a phone call to their son. His eyes were bad and he couldn’t read the phone book, so I looked up the number and dialed the phone for him. He just seemed so helpless, so pathetic. You could tell he just lived and breathed for his wife. He had no idea she was dying. I knew she was dying and I couldn’t tell him.”
It is usually a relief to turn a patient over to the hospital. It only gets tough when paramedics release the patient to a doctor they don’t trust. ‘‘Physicians develop a reputation just like paramedics and anyone else. Sometimes if a good physician will blow it, I’ll think that’s a terrible thing but he’s a good doc, he probably knows he blew it and so I won’t feel too badly about it. But there are doctors I don’t trust, who I wouldn’t let look at me or my wife, Mona. It’s frustrating to bring critical patients to those doctors and know they ’re going to blow it. These doctors are all survivors. They know how to fudge on documentation, on charts to protect themselves. So we try to work around them. If we know a physician we don’t trust is on duty, we’ll do our damdest not to bring him any critical patients. What we ’ll do is fudge a little on where we are. The rules say we’ve got to go to the closest appropriate facility. Of course, you can only do that within limits. I mean, if you’re at one end of town and the only hospital at that end is your hospital, it’s pretty hard to say you ’re not going there. But sometimes when you’re in the middle, in that gray area of overlapping hospital boundaries, you can pick.
“But you can only do that so much and it’s really our only recourse. If a physician does something that we think is really terrible, actually detrimental to the patient, we can file a complaint to the emergency department. Nothing will ever happen, but at least . . . well, you never know. I can’t really say that, that’s cynical. There will be an investigation. It’s just tough because the first thing they ’ll say is, ‘What makes you, someone who’s had maybe a couple of years of experience, six months’ training as a paramedic, what makes you think you could possibly know what a doctor knows?’ ’’
Although Guzman says paramedics share very little in common, they must all have one thing: the ability to make decisions, quickly and confidently. A paramedic can come in any size, shape, shade, or gender, but they must have that one quality. Guzman doesn’t look like a paramedic. At least not like the paramedics of the old television show Emergency! He is short, barrelchested, and inclined toward pudginess. There was a time when he wanted to be a fireman. He went into the physical with folded paper taped to the soles of his feet and two pairs of socks in order to meet the minimum height requirement of five-foot-six. He taped ankle weights beneath his underwear to meet the minimum of 140 pounds. He got halfway through the training before his body told him it didn’t want to be a fireman.
Physical bravery is not part of the job. Guzman leaves that to cops and firemen. “I don’t get paid to risk my life for things like shootings or stab-bings. It’s also policy that in a shooting or stabbing, we wait until the police arrive and tell us the scene is secure. Otherwise, we could end up hostages or worse. So we don’t go in even when we know someone may be bleeding to death, because we have to think of our own safety and the safety of the people who aren’t involved first, and then the well-being of our patient.”
There have been times when Guzman has wondered what the hell he was doing wandering around deserted, dangerous neighborhoods. “I got scared mostly working at Southeast and Logan Heights. One time we got a call for this beating victim in front of a bar in Logan Heights. We got there and we tried to assess this drunk who had been hit over the head with a bottle or something. He was being real uncooperative, kind of belligerent. We were trying to ask him questions and people were coming out of the bar saying, ‘Leave him alone, he’ll be okay.’ We’re saying, ‘Why don’t you let us check him out?’ My partner Lynda and I were trying to be real low-key. They’re getting more excited so we call the police on our radio. This is outside the bar and the crowd is getting bigger. Then somebody throws a bottle at our feet. At that point we left — without the drunk. ‘Sorry, buddy, we gotta go.’
“We got back into the ambulance and I radio all this in, making it sound a little more dramatic. Boy, it didn’t take one minute for the whole place to be surrounded by police cars. Brought their paddy wagon in, closed the bar, and took everybody, including our patient. We drove back and everybody was gone.
“There have been some scary times, always late at night. There are some places in Southeast, like around the fire station at Thirty-sixth and Ocean View, that are really scary. I think that place is the most dangerous, most violent block in the city of San Diego or the county. You can just feel the tension in the air. At any time, day or night, there are always groups of people hanging out on the streets in front of liquor stores or on the curbs. You feel very uneasy, and going there at night is very frightening. On that street, I know I won’t — and I know most paramedics won’t — go into that area without the police. In Logan Heights, it’s around Chicano Park. It’s pretty scary there because there aren’t many residences. It’s all industrial and very dark. A very violent area.
“Still, people are a little more passive there [in Logan Heights]. I think maybe it’s their perception of us. For some reason, they don’t bother us. They’re glad to see us. They appreciate our efforts and think of us as basically the good guys. In Southeast San Diego, I don’t know if we’re viewed as an authority figure or what, but we seem to be resented. That’s an awful generalization because lots of times we go on calls and people are grateful for what we do, but we run into a lot more resentment and threats of violence in that area than we do in Logan Heights, even though both are low-income, minority areas.”
Working in places like Logan Heights and Southeast changes a paramedic. There, the most common calls are the result of abuse or crime — beatings, fights, alcoholic seizures. ‘‘When you see these kinds of people so often, when the problems are mostly those of abusing their own bodies through alcohol or poor nutrition, you can’t help but become bitter and start taking it a little personally when you keep being called out of bed. Many times these people are not nice individuals. Paramedics sometimes take a lot of verbal and even physical abuse. But medics are like everyone else. They need to be appreciated, maybe more than others. They like to be heroes and sometimes, some paramedics expect to be treated like heroes.
‘‘It’s become a battle to avoid becoming cynical and embracing pat answers for complex issues. It’s too easy to become cynical about human nature. The racial issue affects some more than others, but I think it affects everybody to some point. I won’t say working in Logan Heights and Southeast San Diego has made me prejudiced. I will say that it has made me more moderate, more realistic. Maybe even more pessimistic about life and people. I used to think of myself — jokingly — as a bleeding-heart liberal. It was probably fairly true, but after being in these areas I think I can consider myself more of a moderate. I don’t think I’m a bigot. Yet at the same time, I find myself having to work at considering each person as an individual instead of grouping people — and it’s not just by race. Now that I work in Ocean Beach I see all the longhairs who are all druggie-loads and hang out at the beach. The same thing is going to happen there. If I’m not careful when I look at a longhair or someone who’s slightly grungy, I’ll just assume they’re a drug fiend. Just like people did with hippies in the Sixties. Of course, then they all were.” Guzman laughs, remembering the days when he wore beads and long hair.
The job demands teamwork and a special bond between partners and between paramedics, a bond that is reinforced by a sometimes macabre sense of humor. They talk about ‘‘kill lists,” imaginary lists of the people they have personally killed. They complain about some dead guy not being able to take a joke. ‘ ‘He didn’t even die laughing.” And there’s the line about an old, perhaps terminally ill person being reluctant to go to the hospital: ‘‘Like a Roach Motel, they check in, but they don’t check out.”
‘‘The humor is absolutely necessary,” Guzman says. ‘‘We do have a macabre sense of humor. It’s a coping mechanism. The more stressful the call, the crazier I get afterwards. Everything’s silly.
‘‘The kill lists are just a part of the humor. We joke more about the ones we kill than the ones we save because most of the seriously ill still die and only a handful live. So often we get called out even when someone has already died. What happens so often is that people will die in bed, but stay nice and warm. The obvious signs of death won’t set in for quite a long time. In the morning, we’ll look at that patient and say he’s probably been dead for a couple of hours but he’s not cold yet so we’ve got to work him up. There’s a very strict set of guidelines for not initiating CPR, cardiopulmonary resuscitation. Things like rigor mortis have to set in, signs that the blood has pooled in the body or they have to be cold. Those things don’t happen if somebody’s in bed. They don’t happen for a couple of hours. So we go through the motions because we don’t make those judgments. That’s somebody on the kill list. They were long dead before you saw them. There was nothing you could do.
‘‘We only joke about the ones where there was nothing we could have done that would have made any difference. That makes them fair game for humor. If you had someone you really worked hard on, really fought for like this girl in the bay — although I knew in my heart she was going to die — you’ll work very hard because she was so young. We don’t joke about her. At least I don’t. There are people who would, but I don’t think it’s funny.”
The apartment complex on Del Monte Avenue in Ocean Beach was one of those typically nondescript buildings slapped up to house students and lower-income families. It makes no pretense at personality. Guzman and his partner, Tom Vrooman, roll quietly down the street looking for it. Finding it, they hurry through the open security gate, lugging a tackle box full of needles and drugs, an oxygen bottle, and their electrocardiograph machine. The inside of the complex is no more interesting. Two stories of apartments rimmed by walkways encircle a small, rectangular pool. Somewhere nearby an old woman waits, having called earlier complaining of pain. They find the apartment easily enough, but it is locked and the manager is gone. The living room drapes are open, however, and inside lies the woman propped against a bed. She is half sitting, half lying on the floor. Her head is slumped forward and she is leaning motionlessly against an end table covered with medicine bottles.
Guzman crawls through the window and opens the door. The apartment is small and dimly lit. An oscillating fan on the floor gently ruffles the short paisley nightgown of the old woman. Despite the fan and open windows, the air is warm and still. A sickly sweet odor of medicine and age hangs in the air. The paramedics are solicitous and concerned. They call her ‘‘honey ’’ and “dear.” The old woman moans and looks up; she is in terrible pain and cannot move. Her voice is low and raspy. Her name is Ivy. She fell and hurt her tailbone a week ago, but she didn’t want to bother her doctor. But the pain became too much, she couldn’t take it anymore.
Vrooman gently eases her into a more comfortable position and Guzman attaches wired pads to her chest to monitor her heart. Ivy looks fearfully at them and says she has black lung. She used to work in a glue factory until it went under. Vrooman nods, understanding now the reason for the scratchy breathing. The heart seems okay, but the medics are concerned about all the medicines nearby. There are at least seven prescriptions on the end table. “Ivy, do you take all these?” Ivy nods yes. She is seventy-two years old and very sick.
There isn’t much they can do for her but get her to a hospital for x-rays. Vrooman picks her up and gingerly lays her on the gurney. It is easy because Ivy must weigh less than ninety pounds. Ivy will not leave, however, until she has her purse and the paramedics close up and lock her apartment. The paramedics gather her things, turning off the lights and closing the windows. There is something unsettling about doing this, as if they are closing up for good, never to return. As they trundle Ivy through the door, she asks Guzman if the window screen he took off has been replaced. She is scared and it shows; there is suspicion she might never come back. She turns to Vrooman and tells him she has cancer in her chest.
Ed Guzman doesn’t know what happened to Ivy after they left the hospital. He left her with nurses in the emergency room and soon departed oil another call involving drunks in Ocean Beach. “To be honest, I don’t think about Ivy these days,” he says. “Except when I pass her apartment and see the ‘For Rent’ sign. Then I wonder.”

Ed Guzman usually divides death three ways: in beds, in cars, and in alleys. In the beds are the old, in cars the unlucky or irresponsible, in alleys the victims. There are, of course, other divisions, other places to die. Guzman could tell you about those, too. In fact, he could spend all day and all night just telling you a few things he’s noticed about death.
But death occupies only a small part of Guzman’s job as a paramedic. Most of the time, he deals with hurt and confusion. He will tell you about a motorcyclist who scraped off his skin in a skid. He was drunk, Guzman says. No helmet, no shirt. No sympathy. Or the old woman who called an ambulance because she felt poorly and couldn’t afford to go to the doctor. She wasn’t really sick, just scared and lonely. Here, compassion lowers his voice.
He’s got this annoying answer for people who ask him what he did at work today. Same old thing, he says, grinning. Saving lives.
“This was a few months ago, in September or something like that,” Guzman recalls. “This poor girl was sixteen years old, driving her car along the transition ramp from Highway 94 to the southbound 805. For some unknown reason, she lost control of her car, it overturned, and she was thrown out of it. Then another car came along. The driver saw the car, but not the girl in the road. He swerved to miss the car and saw the girl. He swerved again but couldn’t avoid her and overturned his car, too. He didn’t get hurt because he was wearing seatbelts, but the girl had ex-" tensive injuries. Ah geez, she broke almost every bone in her body. She suffered massive head injuries, internal injuries.
“She was in ICU for something like two months, and six months in the hospital altogether. No one really expected her to live, and if she did, everyone expected her to be nothing more than a vegetable. Yet little by little, after suffering all sorts of complications in the hospital like pneumonia, she finally got better. She was discharged just two weeks ago. She had suffered some neurological damage, but she was walking and talking. That was a pretty miraculous recovery. You just have to picture somebody being run over by a two- or three-thousand-pound car and that’s exactly what she looked like. She was squashed. She looked, ah, I can’t even describe it. She just looked so bad. I thought we were going through the motions. I thought she was going to die for sure. But she didn’t. She made it.
“I visited her several times while she was in a coma. When she came out of the coma, they moved her upstairs and I didn’t go up to visit her, so she actually never knew who I was and neither did her family. But yet, I kept an eye on her. I was curious. It was a happy ending, and so many times in something like that we see people who are either not that bad or death is imminent and it’s so very rare that you can actually rip someone from the jaws of death. In her case we did, literally. We, along with everybody else in the hospital, saved her life. She lived to walk out. It was the classic reward of the job. ”
Guzman admits the “classic rewards’’ don’t come very often. “As you begin to work, you realize pretty quickly that only a small part of the calls are true emergencies, the kind people always imagine. Usually they’re something less, but we try to treat everyone like it’s an emergency. Sometimes it’s pretty hard. I can lose my temper with the chronic callers — the widows or widowers — the people who are lonely. They’ll call because they don’t want to be alone at night. They may have some small problem that during the day they can handle. At night, however, when it’s quiet, the problem just gets too big.
“At three in the morning, when you’ve already been out on three calls since midnight and you’re very tired and you recognize the address when the call comes in, you can very easily lose your temper and self-control. The immediate impulse is to lash out at the person who called, but as these things work out, the people who are clironic callers are usually in bad health and you know that one day they’re going to have a real emergency ... so you always treat them as an emergency. ”
More often, however, the calls are mundane, the same things over and over again. They vary only in the different parts of the city. In Southeast San Diego and Logan Heights, it’s beatings and stabbings. Downtown, it’s drunken alcoholic seizures. In Point Loma, heart attacks. And in Ocean Beach, where Guzman works now, it’s drug overdoses. In every part of the city, there is a kind of call that is predominant. The best places to work, Guzman says, are the busy places. Point Loma may have a lot of nice houses and people, but there just isn’t much business out there. Southeast San Diego is poor and sometimes a very scary place. But there, Guzman got to work a lot, seeing calls he just wouldn’t see in a wealthy area where people take better care of themselves.
Most of us have jobs that require making decisions. Very few of us, however, have to make any involving — literally — somebody else’s life. Guzman does and he loves it. “It can be exciting, although it’s certainly not always exciting. There’s a large percentage of ego involved; to say I do it just to help people is too altruistic. It’s more honest for me to say I became a paramedic to have the opportunity to make decisions, to take action to save a life or relieve suffering, saying that feeds the ego a little more.
“Paramedics have a certain arrogance about their professional lives. They are very sure of themselves, almost to a fault. Within about five minutes, they have to walk into a situation, gather an impression, and make decisions, often in adverse conditions, though they have to treat patients as if they’re in a quiet hospital room. There’s a smugness about how they deliver the patient. It’s a common experience among paramedics waiting in the emergency room after bringing in a patient to see nurses and doctors running around in confusion when a patient walks in. It’s kind of amusing.”
At the scene of an accident or injury, a paramedic is usually welcomed as something of a savior. Doctors may save more lives, but they don’t do it with everybody watching. On the street, the paramedic is better than a doctor. “What paramedics have is concentrated training to handle a few specific life-threatening emergencies. In those areas, there’s no doubt in my mind that a paramedic is better able to handle those few emergencies than a doctor. It’s because we have specialized training in a few specialized areas. We aren’t supposed to know all about medicine, only a handful of life-threatening emergencies and immediate, direct intervention.”
On a warm, sunny day in December, a young girl fights for her life in the waters of San Diego Bay near Ballast Point. Above her, white cotton clouds billow to cover a blue sky. Below, a smaller cloud spreads slowly away from the girl, darkening the water to a deeper, rustier shade of gray. Inside this cloud of blood, the girl struggles, one arm thrashing to stay afloat, the other dangling at her side, connected to her body only by ragged tendons and tattered flesh.
Moments before, she had been perched on the bow of a motorboat, sunning herself and enjoying the bouncing ride. Then the boat angled through a wave awkwardly, jerking the bow and the girl into the air. She fell forward into the water, and the boat raced on and caught her in its propeller. Numbly, she can feel her panicked friends pulling her into the boat and laying her gently on the deck. There seems to be blood everywhere, but she feels no pain. She talks to her friends while the boat speeds for shore.
When the call came in, Guzman was lolling around doing nothing in particular. It was one of those days when the calls are infrequent and un-momentous. There was time for a big call, the kind all paramedics like in a weird sort of way. The young girl was that kind of call.
“The call didn’t come in as a drowning. It came in over the alarm system as a stabbing. When we arrived at the harbor patrol, I saw this girl lying on the lawn in front of the office. She had a lot of obvious trauma to her — chest trauma and a three-quarter amputation of her arm at the shoulder. We were unable to tell how internal her injuries were. She was pulseless and abneic, that is, her heart wasn’t beating and she wasn’t breathing. We found out about the boating accident. Apparently she had been talking, communicating with people until she got progressively drowsier and lapsed into unconsciousness. She wasn’t bleeding when we got to her, but she had bled in the water and on the way in. It’s hard to tell how much blood she lost in the water, everything gets so distorted. But by the mechanism of injury, I was assuming her state of cardiac arrest was brought about by excessive hemorrhage. We started to do an I.V. Well, we attempted an I.V., but actually she was so vascularly collapsed that it was impossible to establish a line. Her veins had collapsed because she didn’t have any blood in them.
“So we took her to the hospital and when we got there, the doctor took over. There was some question about the doctor being led to believe — not by us but by his staff or his own impressions — that she was just a simple drowning. He could see her injuries, but because they weren’t bleeding profusely and because he didn’t have a clear picture of how they had occurred, it didn’t enter the doctor’s mind that she wasn’t simply a drowning victim. It’s possible to believe this because it’s possible to suffer an amputated arm without bleeding to death. Her injuries were isolated and she wasn’t bleeding. You can’t really say that’s a terrible thing if you’re a physician and you see only one of these things in your lifetime. He continued on his treatment for drowning for over an hour until she expired. The bottom line is that the autopsy revealed she had exsanguinated her entire blood contents. It’s not so much the controversy of her drowning. The doctor was right: she had suffered a salt-water drowning. Her drowning alone was probably enough to kill her. And the injury alone was certainly enough to kill her. The two together probably made her nonsalvageable, even with aggressive care. ’’
The language Guzman uses, the calm, clinical way he can describe a call, makes him seen unfeeling. Phrases like chest trauma, mechanism of injury, nonsalvageable are simply decorum. “It’s the way doctors talk, the way nurses talk. It’s the way we talk. It’s the only language we have to describe something. Maybe it helps us to remain detached. We can say, ‘Well, the mechanism of injury was such that we suspect internal injuries,’ or we could say, ‘She slammed her chest into the steering wheel and bent it back.’ It saves us from being so graphic.’’
When Guzman smiles, his twenty-six-year-old face — mustachioed and slightly cherubic — becomes a portrait of compassionate tolerance and mild good humor. Anger, disgust, hurt are emotions that rarely show, although certainly he feels them. The girl’s death still bothers him because she was so young and beautiful; it seems so pointless. “There’s more of a feeling of helplessness, more frustration, when these kind of things happen to somebody young. That’s not to say that all people don’t deserve the best care, but it always seems to be such a terrible waste and shame when tragedies occur with somebody young. Paramedics are more affected when it happens to the young than they are when it happens to an older person. You relate more to patients your own age. Not so much in a freak boat accident where you might exercise better judgment than she did sitting in the front of the boat like that. You would hope you know better. It’s the things you know you can’t control, like for example, when you see young people injured in auto accidents. Nobody thinks it will ever happen to them, but every paramedic has got stories of young people they’ve seen get killed. The car crashes they’ve had nothing to do with, minding their own business driving down the road.
“It’s a funny thing about first reactions. I myself have two speeds: slow and fast. You make that initial impression of how serious your patient is, whether you can go slowly at a nice, easy pace or very fast because a lot has to be done because somebody’s life or limb may hang in the balance. When I saw the young girl on the lawn, I switched into the fast mode. In cases like that, I don’t usually see the patient’s face until well into the run. I see it, but I don’t look at it. It wasn’t until well into the run to the hospital that I could see what she looked like. That’s when it starts getting hard. When I’m working fast, the patient’s very anonymous. You can detach yourself. But when you get to the hospital and the family arrives behind you and there’s a name associated with the patient, you can look at the patient and watch the scenario unfold.
“I rarely get so upset I can’t function. It’s only happened about twice in my career. Yet I’ll still get moved, have bouts of depression and anger. Different things affect me. I remember one case when I wasn’t even involved. I was working overtime at the hospital. The paramedics brought in this little old woman. She and her husband — they must have been as old as the hills — in their seventies or eighties. They had been married for eons. Anyway, they were walking, jaywalking across the street and weren’t paying attention. It was dark and a driver didn’t see them and his car hit the woman and broke her hip, her leg, and some internal injuries. Injuries that to you and me wouldn’t be fatal by any means — they would lay us up, but we wouldn’t die. It’s not the same with an old person. I remember watching them work on her in the emergency room and they were working very hard. They worked for hours on her, but she died. I remember watching her die. I was as upset then as I have ever been. I felt so sorry for her and her husband waiting outside.”
Guzman pauses, dark eyes glistening behind tinted glasses, then goes on. ‘‘Because I was the ‘tech’ [technician] on duty, I had to see him, talk to him. He was trying to make a phone call to their son. His eyes were bad and he couldn’t read the phone book, so I looked up the number and dialed the phone for him. He just seemed so helpless, so pathetic. You could tell he just lived and breathed for his wife. He had no idea she was dying. I knew she was dying and I couldn’t tell him.”
It is usually a relief to turn a patient over to the hospital. It only gets tough when paramedics release the patient to a doctor they don’t trust. ‘‘Physicians develop a reputation just like paramedics and anyone else. Sometimes if a good physician will blow it, I’ll think that’s a terrible thing but he’s a good doc, he probably knows he blew it and so I won’t feel too badly about it. But there are doctors I don’t trust, who I wouldn’t let look at me or my wife, Mona. It’s frustrating to bring critical patients to those doctors and know they ’re going to blow it. These doctors are all survivors. They know how to fudge on documentation, on charts to protect themselves. So we try to work around them. If we know a physician we don’t trust is on duty, we’ll do our damdest not to bring him any critical patients. What we ’ll do is fudge a little on where we are. The rules say we’ve got to go to the closest appropriate facility. Of course, you can only do that within limits. I mean, if you’re at one end of town and the only hospital at that end is your hospital, it’s pretty hard to say you ’re not going there. But sometimes when you’re in the middle, in that gray area of overlapping hospital boundaries, you can pick.
“But you can only do that so much and it’s really our only recourse. If a physician does something that we think is really terrible, actually detrimental to the patient, we can file a complaint to the emergency department. Nothing will ever happen, but at least . . . well, you never know. I can’t really say that, that’s cynical. There will be an investigation. It’s just tough because the first thing they ’ll say is, ‘What makes you, someone who’s had maybe a couple of years of experience, six months’ training as a paramedic, what makes you think you could possibly know what a doctor knows?’ ’’
Although Guzman says paramedics share very little in common, they must all have one thing: the ability to make decisions, quickly and confidently. A paramedic can come in any size, shape, shade, or gender, but they must have that one quality. Guzman doesn’t look like a paramedic. At least not like the paramedics of the old television show Emergency! He is short, barrelchested, and inclined toward pudginess. There was a time when he wanted to be a fireman. He went into the physical with folded paper taped to the soles of his feet and two pairs of socks in order to meet the minimum height requirement of five-foot-six. He taped ankle weights beneath his underwear to meet the minimum of 140 pounds. He got halfway through the training before his body told him it didn’t want to be a fireman.
Physical bravery is not part of the job. Guzman leaves that to cops and firemen. “I don’t get paid to risk my life for things like shootings or stab-bings. It’s also policy that in a shooting or stabbing, we wait until the police arrive and tell us the scene is secure. Otherwise, we could end up hostages or worse. So we don’t go in even when we know someone may be bleeding to death, because we have to think of our own safety and the safety of the people who aren’t involved first, and then the well-being of our patient.”
There have been times when Guzman has wondered what the hell he was doing wandering around deserted, dangerous neighborhoods. “I got scared mostly working at Southeast and Logan Heights. One time we got a call for this beating victim in front of a bar in Logan Heights. We got there and we tried to assess this drunk who had been hit over the head with a bottle or something. He was being real uncooperative, kind of belligerent. We were trying to ask him questions and people were coming out of the bar saying, ‘Leave him alone, he’ll be okay.’ We’re saying, ‘Why don’t you let us check him out?’ My partner Lynda and I were trying to be real low-key. They’re getting more excited so we call the police on our radio. This is outside the bar and the crowd is getting bigger. Then somebody throws a bottle at our feet. At that point we left — without the drunk. ‘Sorry, buddy, we gotta go.’
“We got back into the ambulance and I radio all this in, making it sound a little more dramatic. Boy, it didn’t take one minute for the whole place to be surrounded by police cars. Brought their paddy wagon in, closed the bar, and took everybody, including our patient. We drove back and everybody was gone.
“There have been some scary times, always late at night. There are some places in Southeast, like around the fire station at Thirty-sixth and Ocean View, that are really scary. I think that place is the most dangerous, most violent block in the city of San Diego or the county. You can just feel the tension in the air. At any time, day or night, there are always groups of people hanging out on the streets in front of liquor stores or on the curbs. You feel very uneasy, and going there at night is very frightening. On that street, I know I won’t — and I know most paramedics won’t — go into that area without the police. In Logan Heights, it’s around Chicano Park. It’s pretty scary there because there aren’t many residences. It’s all industrial and very dark. A very violent area.
“Still, people are a little more passive there [in Logan Heights]. I think maybe it’s their perception of us. For some reason, they don’t bother us. They’re glad to see us. They appreciate our efforts and think of us as basically the good guys. In Southeast San Diego, I don’t know if we’re viewed as an authority figure or what, but we seem to be resented. That’s an awful generalization because lots of times we go on calls and people are grateful for what we do, but we run into a lot more resentment and threats of violence in that area than we do in Logan Heights, even though both are low-income, minority areas.”
Working in places like Logan Heights and Southeast changes a paramedic. There, the most common calls are the result of abuse or crime — beatings, fights, alcoholic seizures. ‘‘When you see these kinds of people so often, when the problems are mostly those of abusing their own bodies through alcohol or poor nutrition, you can’t help but become bitter and start taking it a little personally when you keep being called out of bed. Many times these people are not nice individuals. Paramedics sometimes take a lot of verbal and even physical abuse. But medics are like everyone else. They need to be appreciated, maybe more than others. They like to be heroes and sometimes, some paramedics expect to be treated like heroes.
‘‘It’s become a battle to avoid becoming cynical and embracing pat answers for complex issues. It’s too easy to become cynical about human nature. The racial issue affects some more than others, but I think it affects everybody to some point. I won’t say working in Logan Heights and Southeast San Diego has made me prejudiced. I will say that it has made me more moderate, more realistic. Maybe even more pessimistic about life and people. I used to think of myself — jokingly — as a bleeding-heart liberal. It was probably fairly true, but after being in these areas I think I can consider myself more of a moderate. I don’t think I’m a bigot. Yet at the same time, I find myself having to work at considering each person as an individual instead of grouping people — and it’s not just by race. Now that I work in Ocean Beach I see all the longhairs who are all druggie-loads and hang out at the beach. The same thing is going to happen there. If I’m not careful when I look at a longhair or someone who’s slightly grungy, I’ll just assume they’re a drug fiend. Just like people did with hippies in the Sixties. Of course, then they all were.” Guzman laughs, remembering the days when he wore beads and long hair.
The job demands teamwork and a special bond between partners and between paramedics, a bond that is reinforced by a sometimes macabre sense of humor. They talk about ‘‘kill lists,” imaginary lists of the people they have personally killed. They complain about some dead guy not being able to take a joke. ‘ ‘He didn’t even die laughing.” And there’s the line about an old, perhaps terminally ill person being reluctant to go to the hospital: ‘‘Like a Roach Motel, they check in, but they don’t check out.”
‘‘The humor is absolutely necessary,” Guzman says. ‘‘We do have a macabre sense of humor. It’s a coping mechanism. The more stressful the call, the crazier I get afterwards. Everything’s silly.
‘‘The kill lists are just a part of the humor. We joke more about the ones we kill than the ones we save because most of the seriously ill still die and only a handful live. So often we get called out even when someone has already died. What happens so often is that people will die in bed, but stay nice and warm. The obvious signs of death won’t set in for quite a long time. In the morning, we’ll look at that patient and say he’s probably been dead for a couple of hours but he’s not cold yet so we’ve got to work him up. There’s a very strict set of guidelines for not initiating CPR, cardiopulmonary resuscitation. Things like rigor mortis have to set in, signs that the blood has pooled in the body or they have to be cold. Those things don’t happen if somebody’s in bed. They don’t happen for a couple of hours. So we go through the motions because we don’t make those judgments. That’s somebody on the kill list. They were long dead before you saw them. There was nothing you could do.
‘‘We only joke about the ones where there was nothing we could have done that would have made any difference. That makes them fair game for humor. If you had someone you really worked hard on, really fought for like this girl in the bay — although I knew in my heart she was going to die — you’ll work very hard because she was so young. We don’t joke about her. At least I don’t. There are people who would, but I don’t think it’s funny.”
The apartment complex on Del Monte Avenue in Ocean Beach was one of those typically nondescript buildings slapped up to house students and lower-income families. It makes no pretense at personality. Guzman and his partner, Tom Vrooman, roll quietly down the street looking for it. Finding it, they hurry through the open security gate, lugging a tackle box full of needles and drugs, an oxygen bottle, and their electrocardiograph machine. The inside of the complex is no more interesting. Two stories of apartments rimmed by walkways encircle a small, rectangular pool. Somewhere nearby an old woman waits, having called earlier complaining of pain. They find the apartment easily enough, but it is locked and the manager is gone. The living room drapes are open, however, and inside lies the woman propped against a bed. She is half sitting, half lying on the floor. Her head is slumped forward and she is leaning motionlessly against an end table covered with medicine bottles.
Guzman crawls through the window and opens the door. The apartment is small and dimly lit. An oscillating fan on the floor gently ruffles the short paisley nightgown of the old woman. Despite the fan and open windows, the air is warm and still. A sickly sweet odor of medicine and age hangs in the air. The paramedics are solicitous and concerned. They call her ‘‘honey ’’ and “dear.” The old woman moans and looks up; she is in terrible pain and cannot move. Her voice is low and raspy. Her name is Ivy. She fell and hurt her tailbone a week ago, but she didn’t want to bother her doctor. But the pain became too much, she couldn’t take it anymore.
Vrooman gently eases her into a more comfortable position and Guzman attaches wired pads to her chest to monitor her heart. Ivy looks fearfully at them and says she has black lung. She used to work in a glue factory until it went under. Vrooman nods, understanding now the reason for the scratchy breathing. The heart seems okay, but the medics are concerned about all the medicines nearby. There are at least seven prescriptions on the end table. “Ivy, do you take all these?” Ivy nods yes. She is seventy-two years old and very sick.
There isn’t much they can do for her but get her to a hospital for x-rays. Vrooman picks her up and gingerly lays her on the gurney. It is easy because Ivy must weigh less than ninety pounds. Ivy will not leave, however, until she has her purse and the paramedics close up and lock her apartment. The paramedics gather her things, turning off the lights and closing the windows. There is something unsettling about doing this, as if they are closing up for good, never to return. As they trundle Ivy through the door, she asks Guzman if the window screen he took off has been replaced. She is scared and it shows; there is suspicion she might never come back. She turns to Vrooman and tells him she has cancer in her chest.
Ed Guzman doesn’t know what happened to Ivy after they left the hospital. He left her with nurses in the emergency room and soon departed oil another call involving drunks in Ocean Beach. “To be honest, I don’t think about Ivy these days,” he says. “Except when I pass her apartment and see the ‘For Rent’ sign. Then I wonder.”
Comments