 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
All he knows for sure is that he woke up beside Otay Reservoir, just north of the Mexican border, on a Friday evening in early November, and that now he’s in the county’s emergency mental hospital. He doesn’t know if he was knocked unconscious or was sleeping. How he got to the reservoir in the first place, and what he was doing there, is a mystery. When he came to, he was wearing dress slacks (with a rip in one knee), a white shirt, a black vest, a green military raincoat, and running shoes. In his pants pocket he had a single tube of Chapstick.
He hadn’t a cent to his name; in fact, even his name had eluded him. He walked to Brown Field, a man without a self, without a past, and from there an ambulance took him to a Chula Vista hospital. When they left him alone, he had never felt more empty, and there was just one thing to do. He slid his belt from around his waist, buckled it around his neck, and tried to hang himself.
“In a way. I wish they’d found no pulse.” says John Doe Number Three, the name given to him in the mental hospital. (There were two other John Does already on the men's ward.) “I get little pieces of memories, and they make me feel kind of sad. And I feel like just dumping it all down the tubes.’’
What do you do with a guy like this? You put him into County Mental Health (CMH), specifically, the men’s acute inpatient ward adjacent to University Hospital in Hillcrest. That’s as much of an answer as most of us want, but it’s really not an answer.
Staffers on the men’s ward at CMH asked themselves the same question 2076 times last year, every time another person was admitted, and the answers they came up with aren’t really answers either. What do you do with a guy like this? You dump him at CMH and pray you’re never in his shoes.

“The psychologist took some tests," continues John Doe Number Three, who thinks he’s twenty-one. “From drawings they can see what kind of person you are. He asked me to draw a picture of a human form, and also asked me to copy some pictures. From these he said I was some kind of depressive schizo-something. some kind of psychological mumbo jumbo . . . According to the psychologist, my memory will come back when my conscience allows it to come back. That’s kind of scary...."
Much about CMH and its patients is kind of scary. For instance, about a week after we talked, John Doe Number Three was released on his own. Hospital staffers had discovered what his name was and that he was from New York, and that he had recently been discharged by the Marine Corps. After they released him he headed for Travelers’ Aid, hoping to obtain a plane ticket home. But the fact that John Doe Number Three and others in need of major assistance are released daily by CMH isn’t the scary part; what’s frightening is that CMH dallies with so many people who need a degree of help that is beyond our capability as a people to provide.
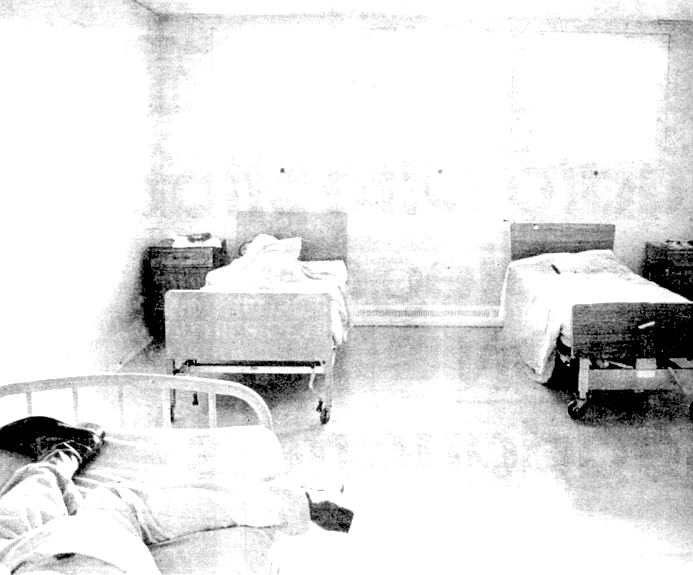
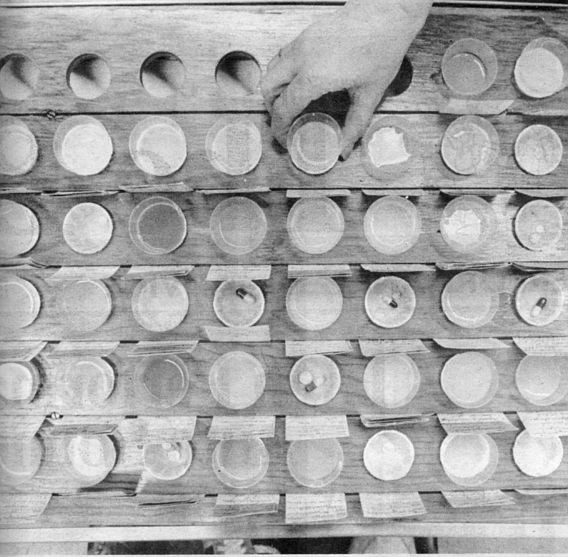
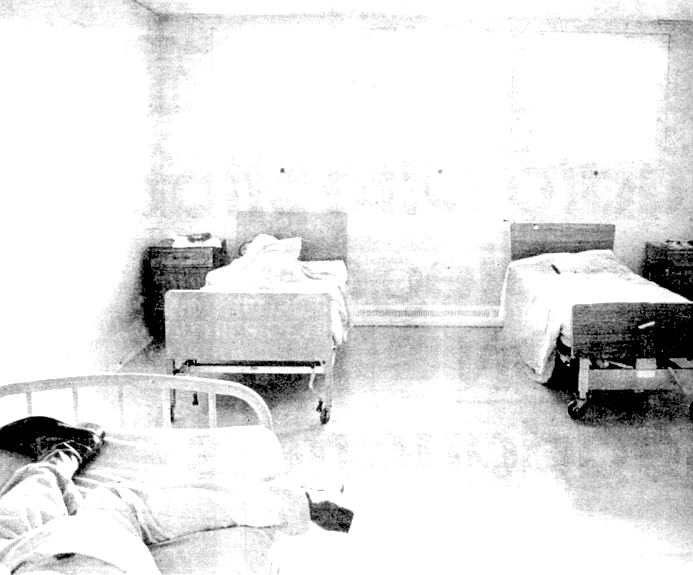
And yet there’s a place where the people in our society who are faring worse than most, those who’ve lost all or parts of themselves, are taken for “treatment.” It has ninety-two beds, fifty-four for men and thirty-eight for women, and it is full most of the time. Ninety-six percent of the people in it are committed involuntarily, usually by the police; the average stay is ten days. The criteria for commitment are that a person be considered a danger to himself or to others, or gravely disabled, meaning he can’t look out for himself. Once he no longer fits those criteria, he can no longer be detained. The Hillcrest facility is not a long-term hospital; the county runs one of those out in Santee, and the state still has its Pattons, Camarillos, and Atascaderos. Hillcrest is strictly a place where the out-of-control regain a grip, where the drug-crazed crash, where the suicidal calm down, where the berserk are momentarily restrained. “Diagnose ’em, test ’em, put ’em on the right course, and put ’em back into the community, that’s our job,” explains Nick Cote, a nursing supervisor. Other nurses put it more bluntly; “You get 'em off the street, dope ’em up, and throw ’em back out on the street,” says one. The “right course” for at feast eighty percent of the patients is some form of psychotropic medication — Thorazine, Haldol, Navane, Melaril. Prolixin, some of the world’s most powerful and mysterious drugs. Putting them back into the community poses a more difficult problem than calming them. For about half the patients released, it simply means giving them bus fare and pointing them toward the door. For the others, it means placing them in a board-and-care home, a kind of halfway house that is arguably just another institution with unlocked doors; or it means releasing them to a conservator, who ostensibly ensures they have food, clothing, shelter, and medical care; or it means giving them back to their family, a rare occurrence. Seldom does it mean releasing them to a “normal,” productive life. About three-fourths of them will be back to the hospital, sooner than later, with the exact same problems. “You know what this place is?” asks one disillusioned nurse’s assistant. “It’s a hotel at the next step from the grave.”
There’s more than a sliver of truth to that characterization, but it still falls far short of reality. Many of the ward’s patients have potentially productive lives ahead of them. Peter Baker, for instance, who came in because of an attempted suicide in late October. When I talked to him (his name, like that of all other patients in this story, has been changed) in early November, he was due to be released the next day. Baker was a twenty-seven-year-old cabdriver who’s recently lost his license (and his job) to a drunken driving conviction. Last spring he lost his girlfriend downtown to a hit-and-run driver who was never captured. “The coroner told me she was pregnant,” Baker said, a deep sigh escorting his sentences, his thick glasses magnifying his frightened eyes. He became unable to pay his rent, so he lost his apartment in Chula Vista. This is his second stint here in three months; the first time he was grabbed by police as he was going over the rail of the Coronado Bridge; this time he was only talking about suicide when he went to the marshal’s office to pay some overdue traffic tickets. “See, I’m not crazy or nothing,” explained Baker, “just suicidal.”
What do you do with a guy like this? At CMH you put him on Trazadone, an antidepressant, and sit him down in the daily group therapy sessions that run from ten to eleven in the morning, where the schizophrenics, manic depressives, and other suicidals chat about their problems. Other than that? “You walk around,” says Baker. “Think about what you’re going to do when you get out. Watch TV. Go outside. Ain’t much to do.”
“Are you being helped here?”
“In a way, yes. But they can’t help me psychologically.”
“They can’t help you at all?”
“Yeah, they can. They can get me another job.”
But when Baker leaves tomorrow, all they’ll be giving him is bus fare. He has no friends who will take him in, and his parents are dead. He hasn't talked to his girlfriend's parents since the funeral. “We were real close there for a while, but after she died, it's like we never knew each other. We became strangers again.” So his bus fare will take him straight to the Plasma Center in National City, where he'll sell his blood for eight dollars a pint. Then it's to the Rescue Mission, he guesses.
The acute care hospital fulfilled its mandate of getting Baker through his momentary' rough spot, but his problems were the same going out as they were coming in. Unlike most of his fellow patients. Baker can’t go onto the public dole because he doesn't have a real mental handicap. Most of the hospital’s customers collect more than $400 (some much more) a month in Supplemental Security Income (SSI) payments. Baker, having been self-employed as a cabdriver, isn’t entitled to unemployment compensation. Where Baker’s real problems begin, the responsibility of CMH ends. But hey, life's tough, right?
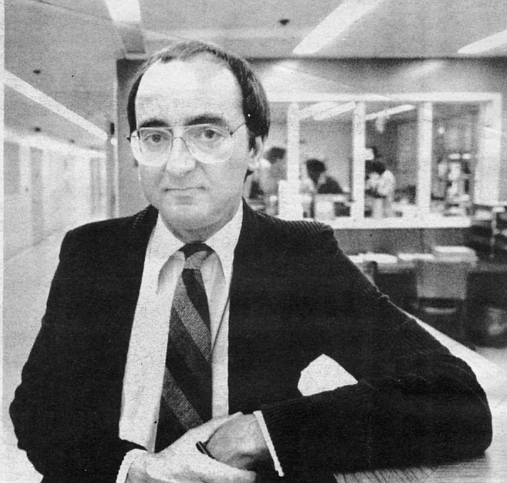
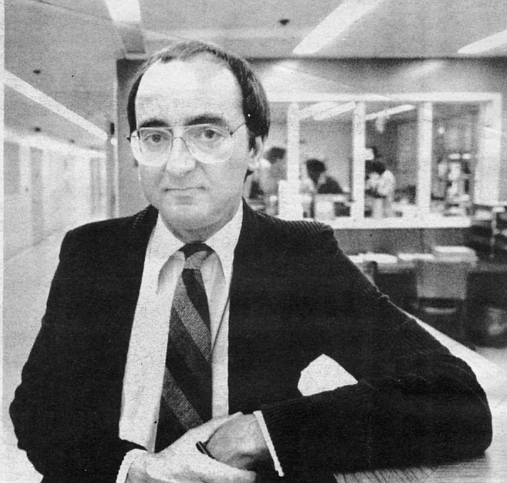
Baker's plight is disturbing for two reasons: increasing numbers of mpeople like him are turning up at the Hillcrest hospital, and the kind of help it can provide those people is extremely limited. Commented one nurse’s assistant, “It seems like the kind of people that really need help, can’t get it here.” I explained Baker’s case and its implications to Dr. W.W. Stadel, who, as administrator in charge of mental health programs for the county from 1949 to 1980, was known as the local “mental health czar.” Halfway through my recitation of the facts, a knowing smile broke across Dr. Stadel’s wise old face, showing that he already had the diagnosis. “What you’re describing is a social problem,” he said. “That’s for sociology to deal with, not psychiatry. ... I came through the Depression, and if you think that’s a problem now, you should have seen it then. This system just wasn't set up to handle that sort of thing.” So Peter Baker took his bus fare and headed for the Plasma Center, and Dr. Stadel and I sat down before the harbor view in his Hillcrest condo and talked about the beginnings of the county’s mental health care system.
When Dr. Stadel arrived in San Diego in 1949, each of California’s fifty-eight counties was sending its mentally ill citizens to the big state hospitals, a practice that in the postwar enlightenment was being described pejoratively as “warehousing.” San Diego was considered progressive because its public psychiatric evaluation center wasn’t located in the county jail, which was common elsewhere throughout the country. The center was a thirty-room building on Third Avenue in Hillcrest, on the site which the Hillcrest Receiving Home now occupies. When someone was formally accused of being mentally ill, a deputy district attorney reviewed the allegation and either rejected it or obtained a court order for the police to go out and pick up the accused. One psychiatrist and a couple of dozen nurses worked at the psychiatric evaluation center, where the person was held until it could be determined whether or not he or she had a mental illness. In four or five days, the person had a court hearing, after which he was either dis charged back home, released to a private psychiatrist, or committed to one of the state hospitals for treatment. But the idea that a mental patient had a right to treatment in his own community became acceptable, and in the early 1950s the county instituted a small outpatient clinic at the psychiatric evaluation center. Then in 1957, with the passage of the state’s landmark Short-Doyle Act, local treatment of the mentally ill became mandatory. San Diego County didn’t participate immediately in the program, which funneled state money into the counties for use in care of the mentally ill (initially the state and counties split the cost fifty-fifty, but now it’s ninety-ten, the state providing the major share); Dr. Stadel and his colleagues had already convinced the board of supervisors to build a short-term psychiatric hospital, which was completed in 1959. It was called the main psycho ward then; today it’s known by the generic CMH.
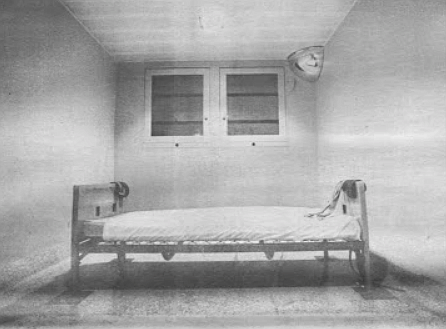
Patients’ rights groups, mental health professionals, and especially the CMH staff deplore the physical layout of the facility, but when it was built, it was state-of-the-art. (It’s going to be taken over in 1986 by University Hospital; a new mental hospital is due to be built at Rosecrans and Pacific Highway, the site of the old FedMart headquarters, where all the county’s health services will be based.) Like all government enterprises, public-funded mental health care is the outgrowth of whatever political and cultural philosophies dominate the times. In 1959 the mentally ill still suffered from the deeply rooted perception that they were social deviants. Many were part of the criminal justice system, and then as now, many were in fact criminals. Therefore, the building was constructed with maximum security in mind. All the massive doors automatically locked when closed. On the men’s ward there were ten seclusion rooms and fifteen bedrooms; on the women’s ward there were ten seclusion rooms, fifteen bedrooms, and later one of these became a shock room. Each ward had a spacious day room where the patients mingled, and they shared a small, outdoor courtyard. The grim atmosphere of the structure matched well the tools at hand: the straitjacket, leather restraints, and shock treatments. (The shock in those days was supplied by massive doses of insulin, which put the patient into a hypoglycemic coma; insulin was later supplanted by electricity.) Today the layout is exactly the same, except that some of the seclusion rooms have been commandeered for use as offices for the psychiatrists, psychologists, various therapists, and social workers now operating on the wards.
Essentially, though psychiatric professionals may argue this point, the treatment today takes the same approach it did in 1959. Its main characteristic is the institution of a structured environment where the stresses and irritations that caused the patient’s problems are removed, in theory, at least. “Initially, the primary thing,’’ explains Dr. Stadel, “was to interrupt the bad living pattern that caused the break that put ’em in there. It was a place to cool your heels." It still is just that, but the treatment differs markedly in two respects: shock treatment has been all but banned, and the psychotropic drugs have made the straitjackets and most of the leather restraints obsolete.
The drugs are generally credited with ushering in the revolution in mental health care that occurred in the 1960s and ’70s. They allowed formerly intransigent and dangerous people to function marginally outside of hospitals, and their use on a wide scale happened to coincide with the cultural change of heart that brought mental health care back to the local level. In the name of more humane, less restrictive treatment, the mentally ill population was “deinstitutionalized” and sent home. In 1967 then-Governor Ronald Reagan emptied out the state mental hospitals almost overnight.
In San Diego the effect was the relatively quick transformation of the main psycho ward in Hillcrest into a small piece of a multitiered system of inpatient and outpatient services. Hotlines, far-flung clinics, and a web of day-care and preventive programs were created. In 1971 the yearly CMH budget was $6,850,000. In 1981 it was $28,283,926. One place within this squirming octopus remained intact and relatively unchanged: the acute care hospital in Hillcrest. And now, with this year's CMH budget suffering its first decline ever, and continued declines assured, one of the few places considered safe from the red pencil is the Hillcrest hospital.
It’s 10:00 p.m. on a Friday night, and all of the forty-four patients on the men’s ward are in bed. Now is the time for the nursing assistants to give Nick Cote, the nursing supervisor, their reports on the progress of the patients they’re assigned to observe. Cote, a registered nurse, sits at a metal desk in a small office next to the nursing station. He jots down notes on a form as his staffers recite their reports.
Mr. Bauer: Still in poor contact, disorganized, refused to keep his slippers on, refused to keep his pajama top on. Still needs direction. Insight into his problems is still questionable.
Mr. Harper: Contact with reality poor, no socializing, cooperative on approach. Spends most of his time staring at himself and combing his hair in the bathroom.
Mr. Mitchell: Good control, contact is fair. Still angry with the Bank of America . . .
“I guess I’m like Martin Luther King,” James Mitchell told me as we sat together on a bench in the courtyard. ‘‘I dream.” A few weeks back Mr. Mitchell, who is fifty-three, waded into the fountain in front of the county courthouse on lower Broadway downtown, and his recurring dream played itself once again in his mind. Sitting on the bottom of San Diego Bay was this little baby who needed help. Helicopters swooped in and dropped down ropes, but the baby just couldn’t reach them. Then all of a sudden, out of the west, from the Silver Strand, walks Christ Himself upon the waters of the bay, and at the same time another Christ approaches from the east, come to save the baby. James Mitchell saw himself as one of those Christs while he waded around in the courthouse fountain. But that’s not what landed him here, in the psycho ward. It was that damn Bank of America, the one on Fifth and Market, that did that.
‘‘I was going to get even with this lady, who said I robbed the bank,” Mitchell explains, his eyes and voice widening with glee at the memory. He says he entered the bank wearing blue swimming trunks, a shirt, shoes, and a pistol holster he got in Tijuana, strapped around his waist. He wrote a counter check for $600. When the teller questioned it, he pulled a fried chicken leg out of the holster, and demanded the money. ‘‘I wasn’t pointing it at her, I was pointing it up. I’d never hurt nobody,” he assures. While waiting for the police to arrive, Mitchell stood off to one side and ate the drumstick. The next thing he knows, he’s domg time in CMH.
Mr. Lathrop: Hostile affect. . . He stated he had money arriving from relatives, and he'd have to stay here in order to get it.
Now, that’s been coming for two weeks. He’s using that as a ploy to stay here. He’s leaving tomorrow.
He claims his testes hurt, he has lower-back pain, and he thinks his arches are falling.
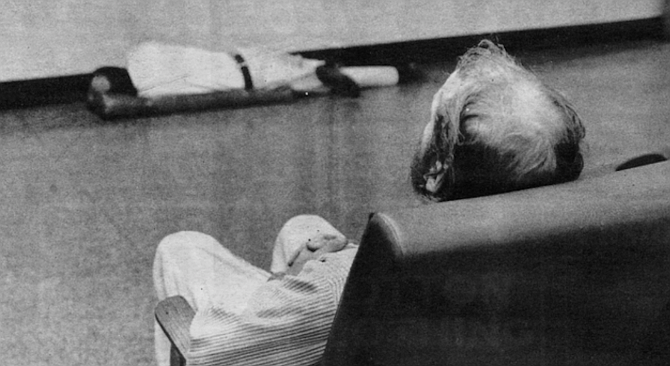
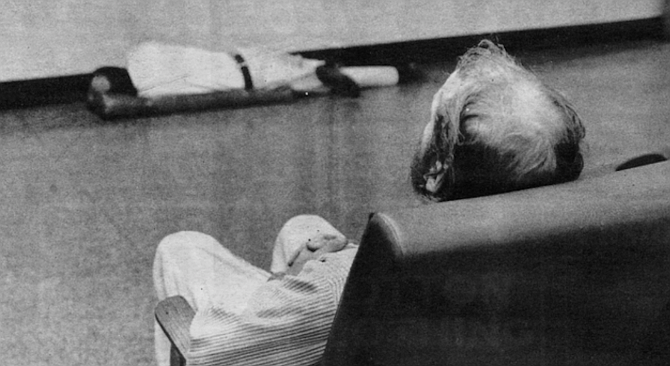
John Doe Number One: Spent most of the p.m. under the table, sleeping. Passive/aggressive on approach.
Mr. Gibson: Slept most of the shift, disheveled appearance, insight poor. Very seclusive, but friendly on approach.
Mr. Elliot: Disheveled, but friendly on approach, insight poor. I asked him where he lives and he said, “Room 101, right down the hall.
Mr. Martinez: He’s doing much better, not acting childish anymore. Good conversation, interaction. He’s asking what he can do to get out of here. I think he’s ready for discharge, myself.
Mr. Foster: His last BP was 152 over 96, but it was fluctuating. He took 2650 cc of fluids. Refused dinner, threw a spoon after Murphy. He’s in better control now, but he still mumbles, talks to himself. With religious overtones . . .
Before I could talk to Richard Foster, who was strapped to his bed in a seclusion room, male nurses wanted to change his pajamas. A blast of urine-heavy air had pounded us when the door was opened — he had peed himself. He was lying flat on his back in the iron frame bed, mumbling up to the ceiling. A wide leather strap looped around his left wrist and was fastened to another strap that ran completely around his waist, and down around the bottom of the bed. His right ankle was also clasped by a loop of leather that was buckled and locked to the foot of the bed. The two nurses released these restraints, and laid them aside. Then, according to their firm but courteous orders, Foster obligingly sat up or laid back and raised his hips as they first removed the soiled bedsheet, and then his light blue pajama bottoms. He wore no top. For a moment he lay there naked, a burly baby with a five-day growth of beard, babbling absently while his diapers were changed. At first it seemed pathetically funny that a forty-five-year-old man was allowing himself to be treated like a baby, but the humor was just a flicker. When they were finished changing him, he helped them replace the leather restraints, and he agreed to talk to me. He was lucid enough to sign his name to a release form. He slowly drew out each letter of his name in shaky script, and except for the mad jitters the signature looked to be straight out of a fifth-grade penmanship lesson.
When the nurses left and closed the door, Foster’s sickness enveloped and dominated the tiny room. His wide brown eyes were welded open, and he never once blinked. Long brown curls of hair squirted from his head. His pudgy torso was marked by bruises on his shoulder and ribs. He could listen in silence to my questions, piercing my gaze with his, but he was completely unable to answer intelligibly. He mouthed an unending and relentless river of disassembled thoughts, commands, prayers, and pieces of scripture. He could tell me nothing about himself or why he was strapped down, on the underbelly of human degradation.
Richard Foster is a regular at CMH. This time he was brought in from county jail, where he had spent just two days before the deputies decided they couldn’t handle him. Although the jail does have a recently opened psychiatric ward, Foster wasn't sent to it because it’s strictly a voluntary ward, and drugs cannot be administered there without the inmate’s consent. At CMH he was under twenty-four-hour guard, and one of the guards said a jailhouse deputy told him Foster had to leave the jail “or his life would be terminated, and not just by the inmates.’’ The guard said he's been eating his own excrement, throwing food, and generally creating havoc. He was being held for burglary. He’d evidently broken into a house, stolen a television set, walked directly out the front door and into the street, stopped the first car to come along, and offered to sell the set to the driver. Unfortunately for him, the driver was a cop, out of uniform. According to the guard, Foster had more than $800 on him when he was arrested. The nurses say he makes a respectable income on government relief. “Hell,” spat the guard, “he makes more money crazy than I do sane.” According to the nurses who attend him, the only therapy Foster isn’t beyond is general kindness, and drugs.
Mr. Jackson: Still delusional, refused dinner, refused fluids. Angry affect. He’s easily agitated.
Yeah, after he showered he still dressed bizarrely, with that towel over his pajamas but between his legs, like a kung fu.
Mr. Clemson: Fair contact, angry, flat, depressed affect, some interaction. He told me his father's spirit visits him here in the hospital. He was talking away to him.
Mr. Carlson: Doing much better, one hundred percent. The doctor told him he hadn’t reached his peak yet. Carlson said he wouldn’t reach it as long as he’s in here. But very conversational, polite.
No more bullying?
No. It’s amazing.
The miracle of Melaril.
He’s on Haldol.
The miracle of Haldol.
Mr. Davis: Soft-spoken, neat appearance, good insight, depressed affect. Appears to resist discharge. He told me, “Maybe I better not go, I’ll probably just take more pills and drink again. I feel like Mount St. Helens with my head ripped off."
Poor-me syndrome, huh?
Yeah, but a nice guy.
Very nice guy . . .
I too found Dennis Davis a very nice guy, but when we talked, he was no longer resisting discharge. This was his third stay at the hospital, and after being there ten days, he felt pretty well evened out. Davis is forty-six, with a long, well-groomed, beard, a balding pate, and gray-blue eyes. He lives downtown in the Las Flores Hotel on Fourth Avenue, across from the Golden West Hotel. He was brought in by the police after trying to throw himself out of a second-story window at the Las Flores. He’d popped several of his Thorazine pills and quaffed a fifth of vodka, behavior for which he thought he had an excellent excuse. “My oldest daughter either committed suicide or was deliberately overdosed on heroin in L.A. on October third,” he says. “It just knocked the stilts out from under me.”
He says he’d gone up to Los Angeles to have her cremated, and now he was about to go up again to place his three grandchildren, aged five, seven, and eleven, in a Seventh Day Adventist boarding school. “I have to explain to them why their momma isn’t coming home. Their father’s afraid to tell them. He said she just went away for a while.”
As we talk in the warm sun of the courtyard a pregnant woman comes out screaming from the women’s ward. “I lost my dollar!” she wails in a voice melted by utter despair. She sits on a bench and sobs while other patients watch impassively. Davis says that he’s spoken with her, and she told him she’s eight months pregnant “and her old man's been beating the hell out of her." She wails on the bench, and nobody moves to comfort her. “I just want a cigarette!” she shrieks, choking on her tears. “Why doesn’t anybody ever give me what I need?” A nurse’s assistant from the men’s ward bounds over to me and says, “You see what I been trying to tell you? Now where’s her nurse? You don’t see her out here trying to calm that poor lady down. She’s in there somewhere sittin’ on her ass.” He disappears back inside.
“Yeah,” says Davis as we watch the pregnant woman start to be encircled by other female patients, “you're supposed to know who your nurse is every day, but there have been days when they’ve never talked to me, and I haven’t known who it was.” Davis says that, like the pregnant lady who’s being comforted now by her peers, he too is helped less by doctors, nurses, or group therapy than by particular patients. “It’s hard to relate to staff members because they’re not alcoholics or drug addicts. That one guy over there, Jim, he has an alcohol and drug problem, he knows what I’ve been through. Same with this guy in the blue T-shirt. I’ve definitely gotten more help from them than I have from staff members.” Still, Davis is generally complimentary of the nurses, who he says “will do their damndest for you, most of them. But others just come in and do their eight hours, sitting on their can all day.”
The staffers themselves convey exactly the same impression. There are the disillusioned: “I’d say about ten of these people are really sick, and eighty of ’em aren’t. They’re lazy, never worked a day in their lives, and they come in here and play sick for a couple of days so they can get a paycheck. If you took half these people off medication and told ’em they couldn’t come back, they’d make it.” There are the cynical: “These folks are copping out on life, and we’re helping them.” There are the frustrated: “Who really cares about the patients? The citizens of San Diego? Hell no. Their families? They don’t care. The conservators? They don’t. I’ve got patients on extended care who’ve been here six months, and their conservators have never visited them. Don’t nobody really care; don’t nobody really give a damn.” There are the undaunted: “If there’s one out of fifty I can help, that’s enough for me.” There are the resigned: “For about fifty percent, there’s just no answer. No matter what medication or support — environmental, biological — psychiatry cannot help these people. We just don’t have the answer. But still, there’s some kind of obligation society has to take care of those who can’t take care of themselves. That’s why I’m here.” There’s a disorienting kind of double gravity at work at CMH. Though it’s only a short-term care facility, the impulse for most staff members is sincerely to try and help their charges. But how much help can you give in two weeks to a person whose whole life has gone haywire? Generally, say staff members, not much. And they even have to be careful not to try and help too much. ‘‘You can do a real disservice to people if you open up a big can of worms inside them and then just let them go out the door,” says one nursing supervisor.
In a way, the Hillcrest hospital is an indigent’s version of the Golden Door health spa: an expensive indulgence (at about $180 a day, per person, mostly picked up by the taxpayer) whose limited and short-term effectiveness is based on the creed of the quick fix. And like a health spa, the length of a person’s stay at CMH is determined not at all by his progress toward health, but by money, bureaucratic strictures, and the need to make room for those newly arriving. Without special circumstances, patients can’t be held longer than seventeen days, and they are routinely discharged simply because there is someone being admitted who is more needful of immediate care. CMH cannot turn away anybody who has been deemed gravely disabled or dangerous either to themselves or to others. ‘‘Instead of saying, ‘Come on in, we’ll help you with your problems,’ ” laments Jean Karr, chief nurse, ‘‘we ask about legalities, laws, rights. And when he leaves, he’s not really better, he’s just learned more about his legal possibilities within the system.”
But given all that should rightfully kill it, the urge to help is still strong among the staff. "Sometimes it’s just a job, and sometimes you can get motivated to really help,” says one nurse’s assistant. Call him Phil. ‘‘You can get motivated by realizing that a certain guy’s extremely dangerous, and shouldn’t see the light of day; I’ve seen murderers in here, who should stay for twenty-five years. You can also get motivated by seeing a guy you can help. Every now and then you get that rare individual who was basically functioning, and his world just dropped out from under him, and he ended up here. We can help that guy.” Phil is an ex-hospital corpsman not yet thirty; he says his Navy training overqualifies him for this job, which pays between five and six dollars per hour. Given the danger (assaults on and injuries to staff are common) and the responsibility (nurses lead group therapy sessions and have more contact, and perhaps even more influence, on patients than do doctors), none of the staff, including Phil, feels justly compensated. But it’s a job. And an education. ‘‘We have a guy in here who chopped off his own hand,” he says, still in awe. “They sewed it back on. He bit off a couple of his fingers. Bit ’em off." These incidents — other nurses tell of three men who cut off their own penises in the ward bathroom — are not looked upon from a clinical perspective by the staff, as might be the wont of a psychiatrist. The nurses are shocked by these things, and their reactions aren't sifted through an academic mesh. The patients seem to sense that the nurses don’t consciously set themselves apart with intellectual or emotional distance, and that in itself is therapeutic. For many patients, this human civility is the only workable therapy. Aside from drugs, of course.
Herman Billings, a small black man in his fifties, was admitted to the hospital on a recent Saturday afternoon. He was brought in by the police after they caught him jumping in front of cars on the street. He was generally calm and cooperative with the nurses and obviously in familiar surroundings, but when it came time for him to take his medication, which was almost immediately after he arrived at the nursing station, he would have none of it. ‘‘Now, Herman, doctor wants you to take this medicine,” explained the nurse in charge, holding out a little paper cup filled with Haldol and lilting her voice like a mother talking to a juvenile. Herman, shirtless and vulnerable, stands by himself near the nursing station and says he doesn't want no medicine.
‘‘I just want a shower, a shave, and some nourishment,” he says straightforwardly, trying to be reasonable.
‘‘Now, Herman, this medicine is good for you. If you don’t swallow it we’ll have to give it to you by injection.”
‘‘No ma’am, I don’t want none of that. I just want to get cleaned up a little.”
“Okay, Herman.” Someone goes to summon a couple of male nurses, and Herman, still standing alone, starts to moan like a cornered animal.
“Ohhh Gaaawd!” he yells in an unpanicked voice. ‘‘Thank Gaaawd! Mercy!” He stomps his foot. “Mercyyyyy!”
As the men approach calmly and try to reassure Herman, a desk clerk looks up at me and says, ‘‘Can you imagine what it was like before we had drugs? We used to have to wrap ’em in wet towels to control ’em.”
‘‘Man, all I want is a shower and a shave,” Herman beseeches the male nurses. They talk softly to him as the chief nurse comes out of the medication room with a syringe full of Haldol.
“Come on, Herman, it’s to help you.”
‘‘I don’t even know what it is. Please. Pleeeeeease!”
The men muscle him through the locker-room door and press him firmly against one of the tall beige lockers. ‘‘All right, all right. I’ll take it,” Herman yells, but they aren’t turning him loose now. The chief nurse undoes Herman’s pants and pulls them down, exposing his small ebony butt. Herman’s breath comes fast and shallow. The black male nurse presses his face into Herman’s and stares intensely into his eyes. ‘‘It’s cool, man, it’s cool,” he says soothingly.
‘‘Don’t tighten up, Herman,” commands the nurse with the needle. She slaps his butt once, twice.
"All right, I’ll take it,” Herman insists.
‘‘It’s cool, man.” The male nurse tightens his grip. The needle is in. Herman relaxes like a collapsing balloon.
He was released four days later on his own.
Ultimately, of course, it’s the psychiatrists at CMH who are in charge of the patients’ treatment. They determine who gets into the hospital, what kind of disorder he's suffering from, what drugs, if any, to administer, and when a patient is ready to be released. For fifteen years Dr. Socrates Pappas has worked at the hospital, and now he’s the supervising psychiatrist, with a small office that used to be a seclusion room just a few steps away from the nurses’ station. A humorous and nervous and approachable man, Pappas is the last one who’d claim much of a success rate in straightening out his patients’ lives. But when I questioned the benefits of the psychotropic drugs, his response was immediate: “Yes, the medication does help people. Without the drugs, many of them would be locked up. It’s better that they’re not locked up. That’s better. Families come in and say, ‘Doctor, if you’ll just give him his medicine, and if he’ll take it, I want him home.’ When he doesn’t take it, he throws the TV through the picture window, chokes dad, barricades himself in his room, hears voices. When he takes it, he may still have those urges, but he’s able not to act on them. He can live at home. That’s better."
Dr. Pappas estimates that only about ten percent of his patients really want to talk to him about their personal problems, “and the other ninety percent go back to wherever they were before they came in." Though he says he’s not a rebel, he holds personal beliefs about the treatment of the mentally ill that run counter to the system. If it were up to him, he might like to write down that somebody was a mean, nasty old cuss instead of a manic depressive with severe assaultive tendencies. “But the system, and the paperwork, demands those labels.” He even has personal doubts about committing and detaining people against their will. Some in his profession, and even on his ward, believe that totally structuring a patient's environment and relieving him of every responsibility is the ultimate dehumanization, and that in the long run it works against that person’s mental health. So what do you do with people who have serious psychological problems? If they don’t seek help voluntarily says Pappas, maybe we should try just leaving them alone. “If the voices tell him to break a window and he does, arrest him. Make him responsible for what he hears.’’ Though it sounds like a radical theory, how much less effective than the current system could it be?
As we talked, it became clear that Pappas was edgy about something. The conversation worked its way around to violence on the ward, and the psychiatrist boasted that working fifteen years in a place considered more dangerous than a jailhouse, he had yet to be attacked. Then came this: thirteen days before, Pappas was awakened in the night by the telephone. The man on the other end of the line was a former patient in the hospital who didn’t like the way Pappas had treated him, and he told the doctor that he knew where he lived, what car he drove, what his schedule was, and that he’d better get a bulletproof vest because in two weeks the doctor was going to be killed. Pappas had never been threatened like that before, and he took it seriously enough to call the police. After the psychiatrist told the story several different times to incredulous but sympathetic detectives, a patrolman was dispatched to talk to him at CMH. Pappas told Sgt. Rice the story, who listened politely and then said what the doctor had heard umpteen times before: there was nothing the police could do. But then Sgt. Rice did offer a solution, of sorts. He said that if Pappas should receive a threatening call like that two more times, he should get his phone number changed, “because no citizen should have to put up with that kind of thing.’’ We both laughed at the absurdity of such a solution. It wasn’t until later that I realized the policeman had given Dr. Pappas the same prescription that his own hospital dispenses in little paper cups every day.

All he knows for sure is that he woke up beside Otay Reservoir, just north of the Mexican border, on a Friday evening in early November, and that now he’s in the county’s emergency mental hospital. He doesn’t know if he was knocked unconscious or was sleeping. How he got to the reservoir in the first place, and what he was doing there, is a mystery. When he came to, he was wearing dress slacks (with a rip in one knee), a white shirt, a black vest, a green military raincoat, and running shoes. In his pants pocket he had a single tube of Chapstick.
He hadn’t a cent to his name; in fact, even his name had eluded him. He walked to Brown Field, a man without a self, without a past, and from there an ambulance took him to a Chula Vista hospital. When they left him alone, he had never felt more empty, and there was just one thing to do. He slid his belt from around his waist, buckled it around his neck, and tried to hang himself.
“In a way. I wish they’d found no pulse.” says John Doe Number Three, the name given to him in the mental hospital. (There were two other John Does already on the men's ward.) “I get little pieces of memories, and they make me feel kind of sad. And I feel like just dumping it all down the tubes.’’
What do you do with a guy like this? You put him into County Mental Health (CMH), specifically, the men’s acute inpatient ward adjacent to University Hospital in Hillcrest. That’s as much of an answer as most of us want, but it’s really not an answer.
Staffers on the men’s ward at CMH asked themselves the same question 2076 times last year, every time another person was admitted, and the answers they came up with aren’t really answers either. What do you do with a guy like this? You dump him at CMH and pray you’re never in his shoes.

“The psychologist took some tests," continues John Doe Number Three, who thinks he’s twenty-one. “From drawings they can see what kind of person you are. He asked me to draw a picture of a human form, and also asked me to copy some pictures. From these he said I was some kind of depressive schizo-something. some kind of psychological mumbo jumbo . . . According to the psychologist, my memory will come back when my conscience allows it to come back. That’s kind of scary...."
Much about CMH and its patients is kind of scary. For instance, about a week after we talked, John Doe Number Three was released on his own. Hospital staffers had discovered what his name was and that he was from New York, and that he had recently been discharged by the Marine Corps. After they released him he headed for Travelers’ Aid, hoping to obtain a plane ticket home. But the fact that John Doe Number Three and others in need of major assistance are released daily by CMH isn’t the scary part; what’s frightening is that CMH dallies with so many people who need a degree of help that is beyond our capability as a people to provide.
And yet there’s a place where the people in our society who are faring worse than most, those who’ve lost all or parts of themselves, are taken for “treatment.” It has ninety-two beds, fifty-four for men and thirty-eight for women, and it is full most of the time. Ninety-six percent of the people in it are committed involuntarily, usually by the police; the average stay is ten days. The criteria for commitment are that a person be considered a danger to himself or to others, or gravely disabled, meaning he can’t look out for himself. Once he no longer fits those criteria, he can no longer be detained. The Hillcrest facility is not a long-term hospital; the county runs one of those out in Santee, and the state still has its Pattons, Camarillos, and Atascaderos. Hillcrest is strictly a place where the out-of-control regain a grip, where the drug-crazed crash, where the suicidal calm down, where the berserk are momentarily restrained. “Diagnose ’em, test ’em, put ’em on the right course, and put ’em back into the community, that’s our job,” explains Nick Cote, a nursing supervisor. Other nurses put it more bluntly; “You get 'em off the street, dope ’em up, and throw ’em back out on the street,” says one. The “right course” for at feast eighty percent of the patients is some form of psychotropic medication — Thorazine, Haldol, Navane, Melaril. Prolixin, some of the world’s most powerful and mysterious drugs. Putting them back into the community poses a more difficult problem than calming them. For about half the patients released, it simply means giving them bus fare and pointing them toward the door. For the others, it means placing them in a board-and-care home, a kind of halfway house that is arguably just another institution with unlocked doors; or it means releasing them to a conservator, who ostensibly ensures they have food, clothing, shelter, and medical care; or it means giving them back to their family, a rare occurrence. Seldom does it mean releasing them to a “normal,” productive life. About three-fourths of them will be back to the hospital, sooner than later, with the exact same problems. “You know what this place is?” asks one disillusioned nurse’s assistant. “It’s a hotel at the next step from the grave.”
There’s more than a sliver of truth to that characterization, but it still falls far short of reality. Many of the ward’s patients have potentially productive lives ahead of them. Peter Baker, for instance, who came in because of an attempted suicide in late October. When I talked to him (his name, like that of all other patients in this story, has been changed) in early November, he was due to be released the next day. Baker was a twenty-seven-year-old cabdriver who’s recently lost his license (and his job) to a drunken driving conviction. Last spring he lost his girlfriend downtown to a hit-and-run driver who was never captured. “The coroner told me she was pregnant,” Baker said, a deep sigh escorting his sentences, his thick glasses magnifying his frightened eyes. He became unable to pay his rent, so he lost his apartment in Chula Vista. This is his second stint here in three months; the first time he was grabbed by police as he was going over the rail of the Coronado Bridge; this time he was only talking about suicide when he went to the marshal’s office to pay some overdue traffic tickets. “See, I’m not crazy or nothing,” explained Baker, “just suicidal.”
What do you do with a guy like this? At CMH you put him on Trazadone, an antidepressant, and sit him down in the daily group therapy sessions that run from ten to eleven in the morning, where the schizophrenics, manic depressives, and other suicidals chat about their problems. Other than that? “You walk around,” says Baker. “Think about what you’re going to do when you get out. Watch TV. Go outside. Ain’t much to do.”
“Are you being helped here?”
“In a way, yes. But they can’t help me psychologically.”
“They can’t help you at all?”
“Yeah, they can. They can get me another job.”
But when Baker leaves tomorrow, all they’ll be giving him is bus fare. He has no friends who will take him in, and his parents are dead. He hasn't talked to his girlfriend's parents since the funeral. “We were real close there for a while, but after she died, it's like we never knew each other. We became strangers again.” So his bus fare will take him straight to the Plasma Center in National City, where he'll sell his blood for eight dollars a pint. Then it's to the Rescue Mission, he guesses.
The acute care hospital fulfilled its mandate of getting Baker through his momentary' rough spot, but his problems were the same going out as they were coming in. Unlike most of his fellow patients. Baker can’t go onto the public dole because he doesn't have a real mental handicap. Most of the hospital’s customers collect more than $400 (some much more) a month in Supplemental Security Income (SSI) payments. Baker, having been self-employed as a cabdriver, isn’t entitled to unemployment compensation. Where Baker’s real problems begin, the responsibility of CMH ends. But hey, life's tough, right?
Baker's plight is disturbing for two reasons: increasing numbers of mpeople like him are turning up at the Hillcrest hospital, and the kind of help it can provide those people is extremely limited. Commented one nurse’s assistant, “It seems like the kind of people that really need help, can’t get it here.” I explained Baker’s case and its implications to Dr. W.W. Stadel, who, as administrator in charge of mental health programs for the county from 1949 to 1980, was known as the local “mental health czar.” Halfway through my recitation of the facts, a knowing smile broke across Dr. Stadel’s wise old face, showing that he already had the diagnosis. “What you’re describing is a social problem,” he said. “That’s for sociology to deal with, not psychiatry. ... I came through the Depression, and if you think that’s a problem now, you should have seen it then. This system just wasn't set up to handle that sort of thing.” So Peter Baker took his bus fare and headed for the Plasma Center, and Dr. Stadel and I sat down before the harbor view in his Hillcrest condo and talked about the beginnings of the county’s mental health care system.
When Dr. Stadel arrived in San Diego in 1949, each of California’s fifty-eight counties was sending its mentally ill citizens to the big state hospitals, a practice that in the postwar enlightenment was being described pejoratively as “warehousing.” San Diego was considered progressive because its public psychiatric evaluation center wasn’t located in the county jail, which was common elsewhere throughout the country. The center was a thirty-room building on Third Avenue in Hillcrest, on the site which the Hillcrest Receiving Home now occupies. When someone was formally accused of being mentally ill, a deputy district attorney reviewed the allegation and either rejected it or obtained a court order for the police to go out and pick up the accused. One psychiatrist and a couple of dozen nurses worked at the psychiatric evaluation center, where the person was held until it could be determined whether or not he or she had a mental illness. In four or five days, the person had a court hearing, after which he was either dis charged back home, released to a private psychiatrist, or committed to one of the state hospitals for treatment. But the idea that a mental patient had a right to treatment in his own community became acceptable, and in the early 1950s the county instituted a small outpatient clinic at the psychiatric evaluation center. Then in 1957, with the passage of the state’s landmark Short-Doyle Act, local treatment of the mentally ill became mandatory. San Diego County didn’t participate immediately in the program, which funneled state money into the counties for use in care of the mentally ill (initially the state and counties split the cost fifty-fifty, but now it’s ninety-ten, the state providing the major share); Dr. Stadel and his colleagues had already convinced the board of supervisors to build a short-term psychiatric hospital, which was completed in 1959. It was called the main psycho ward then; today it’s known by the generic CMH.
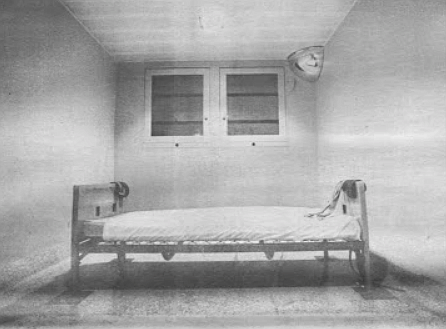
Patients’ rights groups, mental health professionals, and especially the CMH staff deplore the physical layout of the facility, but when it was built, it was state-of-the-art. (It’s going to be taken over in 1986 by University Hospital; a new mental hospital is due to be built at Rosecrans and Pacific Highway, the site of the old FedMart headquarters, where all the county’s health services will be based.) Like all government enterprises, public-funded mental health care is the outgrowth of whatever political and cultural philosophies dominate the times. In 1959 the mentally ill still suffered from the deeply rooted perception that they were social deviants. Many were part of the criminal justice system, and then as now, many were in fact criminals. Therefore, the building was constructed with maximum security in mind. All the massive doors automatically locked when closed. On the men’s ward there were ten seclusion rooms and fifteen bedrooms; on the women’s ward there were ten seclusion rooms, fifteen bedrooms, and later one of these became a shock room. Each ward had a spacious day room where the patients mingled, and they shared a small, outdoor courtyard. The grim atmosphere of the structure matched well the tools at hand: the straitjacket, leather restraints, and shock treatments. (The shock in those days was supplied by massive doses of insulin, which put the patient into a hypoglycemic coma; insulin was later supplanted by electricity.) Today the layout is exactly the same, except that some of the seclusion rooms have been commandeered for use as offices for the psychiatrists, psychologists, various therapists, and social workers now operating on the wards.
Essentially, though psychiatric professionals may argue this point, the treatment today takes the same approach it did in 1959. Its main characteristic is the institution of a structured environment where the stresses and irritations that caused the patient’s problems are removed, in theory, at least. “Initially, the primary thing,’’ explains Dr. Stadel, “was to interrupt the bad living pattern that caused the break that put ’em in there. It was a place to cool your heels." It still is just that, but the treatment differs markedly in two respects: shock treatment has been all but banned, and the psychotropic drugs have made the straitjackets and most of the leather restraints obsolete.
The drugs are generally credited with ushering in the revolution in mental health care that occurred in the 1960s and ’70s. They allowed formerly intransigent and dangerous people to function marginally outside of hospitals, and their use on a wide scale happened to coincide with the cultural change of heart that brought mental health care back to the local level. In the name of more humane, less restrictive treatment, the mentally ill population was “deinstitutionalized” and sent home. In 1967 then-Governor Ronald Reagan emptied out the state mental hospitals almost overnight.
In San Diego the effect was the relatively quick transformation of the main psycho ward in Hillcrest into a small piece of a multitiered system of inpatient and outpatient services. Hotlines, far-flung clinics, and a web of day-care and preventive programs were created. In 1971 the yearly CMH budget was $6,850,000. In 1981 it was $28,283,926. One place within this squirming octopus remained intact and relatively unchanged: the acute care hospital in Hillcrest. And now, with this year's CMH budget suffering its first decline ever, and continued declines assured, one of the few places considered safe from the red pencil is the Hillcrest hospital.
It’s 10:00 p.m. on a Friday night, and all of the forty-four patients on the men’s ward are in bed. Now is the time for the nursing assistants to give Nick Cote, the nursing supervisor, their reports on the progress of the patients they’re assigned to observe. Cote, a registered nurse, sits at a metal desk in a small office next to the nursing station. He jots down notes on a form as his staffers recite their reports.
Mr. Bauer: Still in poor contact, disorganized, refused to keep his slippers on, refused to keep his pajama top on. Still needs direction. Insight into his problems is still questionable.
Mr. Harper: Contact with reality poor, no socializing, cooperative on approach. Spends most of his time staring at himself and combing his hair in the bathroom.
Mr. Mitchell: Good control, contact is fair. Still angry with the Bank of America . . .
“I guess I’m like Martin Luther King,” James Mitchell told me as we sat together on a bench in the courtyard. ‘‘I dream.” A few weeks back Mr. Mitchell, who is fifty-three, waded into the fountain in front of the county courthouse on lower Broadway downtown, and his recurring dream played itself once again in his mind. Sitting on the bottom of San Diego Bay was this little baby who needed help. Helicopters swooped in and dropped down ropes, but the baby just couldn’t reach them. Then all of a sudden, out of the west, from the Silver Strand, walks Christ Himself upon the waters of the bay, and at the same time another Christ approaches from the east, come to save the baby. James Mitchell saw himself as one of those Christs while he waded around in the courthouse fountain. But that’s not what landed him here, in the psycho ward. It was that damn Bank of America, the one on Fifth and Market, that did that.
‘‘I was going to get even with this lady, who said I robbed the bank,” Mitchell explains, his eyes and voice widening with glee at the memory. He says he entered the bank wearing blue swimming trunks, a shirt, shoes, and a pistol holster he got in Tijuana, strapped around his waist. He wrote a counter check for $600. When the teller questioned it, he pulled a fried chicken leg out of the holster, and demanded the money. ‘‘I wasn’t pointing it at her, I was pointing it up. I’d never hurt nobody,” he assures. While waiting for the police to arrive, Mitchell stood off to one side and ate the drumstick. The next thing he knows, he’s domg time in CMH.
Mr. Lathrop: Hostile affect. . . He stated he had money arriving from relatives, and he'd have to stay here in order to get it.
Now, that’s been coming for two weeks. He’s using that as a ploy to stay here. He’s leaving tomorrow.
He claims his testes hurt, he has lower-back pain, and he thinks his arches are falling.
John Doe Number One: Spent most of the p.m. under the table, sleeping. Passive/aggressive on approach.
Mr. Gibson: Slept most of the shift, disheveled appearance, insight poor. Very seclusive, but friendly on approach.
Mr. Elliot: Disheveled, but friendly on approach, insight poor. I asked him where he lives and he said, “Room 101, right down the hall.
Mr. Martinez: He’s doing much better, not acting childish anymore. Good conversation, interaction. He’s asking what he can do to get out of here. I think he’s ready for discharge, myself.
Mr. Foster: His last BP was 152 over 96, but it was fluctuating. He took 2650 cc of fluids. Refused dinner, threw a spoon after Murphy. He’s in better control now, but he still mumbles, talks to himself. With religious overtones . . .
Before I could talk to Richard Foster, who was strapped to his bed in a seclusion room, male nurses wanted to change his pajamas. A blast of urine-heavy air had pounded us when the door was opened — he had peed himself. He was lying flat on his back in the iron frame bed, mumbling up to the ceiling. A wide leather strap looped around his left wrist and was fastened to another strap that ran completely around his waist, and down around the bottom of the bed. His right ankle was also clasped by a loop of leather that was buckled and locked to the foot of the bed. The two nurses released these restraints, and laid them aside. Then, according to their firm but courteous orders, Foster obligingly sat up or laid back and raised his hips as they first removed the soiled bedsheet, and then his light blue pajama bottoms. He wore no top. For a moment he lay there naked, a burly baby with a five-day growth of beard, babbling absently while his diapers were changed. At first it seemed pathetically funny that a forty-five-year-old man was allowing himself to be treated like a baby, but the humor was just a flicker. When they were finished changing him, he helped them replace the leather restraints, and he agreed to talk to me. He was lucid enough to sign his name to a release form. He slowly drew out each letter of his name in shaky script, and except for the mad jitters the signature looked to be straight out of a fifth-grade penmanship lesson.
When the nurses left and closed the door, Foster’s sickness enveloped and dominated the tiny room. His wide brown eyes were welded open, and he never once blinked. Long brown curls of hair squirted from his head. His pudgy torso was marked by bruises on his shoulder and ribs. He could listen in silence to my questions, piercing my gaze with his, but he was completely unable to answer intelligibly. He mouthed an unending and relentless river of disassembled thoughts, commands, prayers, and pieces of scripture. He could tell me nothing about himself or why he was strapped down, on the underbelly of human degradation.
Richard Foster is a regular at CMH. This time he was brought in from county jail, where he had spent just two days before the deputies decided they couldn’t handle him. Although the jail does have a recently opened psychiatric ward, Foster wasn't sent to it because it’s strictly a voluntary ward, and drugs cannot be administered there without the inmate’s consent. At CMH he was under twenty-four-hour guard, and one of the guards said a jailhouse deputy told him Foster had to leave the jail “or his life would be terminated, and not just by the inmates.’’ The guard said he's been eating his own excrement, throwing food, and generally creating havoc. He was being held for burglary. He’d evidently broken into a house, stolen a television set, walked directly out the front door and into the street, stopped the first car to come along, and offered to sell the set to the driver. Unfortunately for him, the driver was a cop, out of uniform. According to the guard, Foster had more than $800 on him when he was arrested. The nurses say he makes a respectable income on government relief. “Hell,” spat the guard, “he makes more money crazy than I do sane.” According to the nurses who attend him, the only therapy Foster isn’t beyond is general kindness, and drugs.
Mr. Jackson: Still delusional, refused dinner, refused fluids. Angry affect. He’s easily agitated.
Yeah, after he showered he still dressed bizarrely, with that towel over his pajamas but between his legs, like a kung fu.
Mr. Clemson: Fair contact, angry, flat, depressed affect, some interaction. He told me his father's spirit visits him here in the hospital. He was talking away to him.
Mr. Carlson: Doing much better, one hundred percent. The doctor told him he hadn’t reached his peak yet. Carlson said he wouldn’t reach it as long as he’s in here. But very conversational, polite.
No more bullying?
No. It’s amazing.
The miracle of Melaril.
He’s on Haldol.
The miracle of Haldol.
Mr. Davis: Soft-spoken, neat appearance, good insight, depressed affect. Appears to resist discharge. He told me, “Maybe I better not go, I’ll probably just take more pills and drink again. I feel like Mount St. Helens with my head ripped off."
Poor-me syndrome, huh?
Yeah, but a nice guy.
Very nice guy . . .
I too found Dennis Davis a very nice guy, but when we talked, he was no longer resisting discharge. This was his third stay at the hospital, and after being there ten days, he felt pretty well evened out. Davis is forty-six, with a long, well-groomed, beard, a balding pate, and gray-blue eyes. He lives downtown in the Las Flores Hotel on Fourth Avenue, across from the Golden West Hotel. He was brought in by the police after trying to throw himself out of a second-story window at the Las Flores. He’d popped several of his Thorazine pills and quaffed a fifth of vodka, behavior for which he thought he had an excellent excuse. “My oldest daughter either committed suicide or was deliberately overdosed on heroin in L.A. on October third,” he says. “It just knocked the stilts out from under me.”
He says he’d gone up to Los Angeles to have her cremated, and now he was about to go up again to place his three grandchildren, aged five, seven, and eleven, in a Seventh Day Adventist boarding school. “I have to explain to them why their momma isn’t coming home. Their father’s afraid to tell them. He said she just went away for a while.”
As we talk in the warm sun of the courtyard a pregnant woman comes out screaming from the women’s ward. “I lost my dollar!” she wails in a voice melted by utter despair. She sits on a bench and sobs while other patients watch impassively. Davis says that he’s spoken with her, and she told him she’s eight months pregnant “and her old man's been beating the hell out of her." She wails on the bench, and nobody moves to comfort her. “I just want a cigarette!” she shrieks, choking on her tears. “Why doesn’t anybody ever give me what I need?” A nurse’s assistant from the men’s ward bounds over to me and says, “You see what I been trying to tell you? Now where’s her nurse? You don’t see her out here trying to calm that poor lady down. She’s in there somewhere sittin’ on her ass.” He disappears back inside.
“Yeah,” says Davis as we watch the pregnant woman start to be encircled by other female patients, “you're supposed to know who your nurse is every day, but there have been days when they’ve never talked to me, and I haven’t known who it was.” Davis says that, like the pregnant lady who’s being comforted now by her peers, he too is helped less by doctors, nurses, or group therapy than by particular patients. “It’s hard to relate to staff members because they’re not alcoholics or drug addicts. That one guy over there, Jim, he has an alcohol and drug problem, he knows what I’ve been through. Same with this guy in the blue T-shirt. I’ve definitely gotten more help from them than I have from staff members.” Still, Davis is generally complimentary of the nurses, who he says “will do their damndest for you, most of them. But others just come in and do their eight hours, sitting on their can all day.”
The staffers themselves convey exactly the same impression. There are the disillusioned: “I’d say about ten of these people are really sick, and eighty of ’em aren’t. They’re lazy, never worked a day in their lives, and they come in here and play sick for a couple of days so they can get a paycheck. If you took half these people off medication and told ’em they couldn’t come back, they’d make it.” There are the cynical: “These folks are copping out on life, and we’re helping them.” There are the frustrated: “Who really cares about the patients? The citizens of San Diego? Hell no. Their families? They don’t care. The conservators? They don’t. I’ve got patients on extended care who’ve been here six months, and their conservators have never visited them. Don’t nobody really care; don’t nobody really give a damn.” There are the undaunted: “If there’s one out of fifty I can help, that’s enough for me.” There are the resigned: “For about fifty percent, there’s just no answer. No matter what medication or support — environmental, biological — psychiatry cannot help these people. We just don’t have the answer. But still, there’s some kind of obligation society has to take care of those who can’t take care of themselves. That’s why I’m here.” There’s a disorienting kind of double gravity at work at CMH. Though it’s only a short-term care facility, the impulse for most staff members is sincerely to try and help their charges. But how much help can you give in two weeks to a person whose whole life has gone haywire? Generally, say staff members, not much. And they even have to be careful not to try and help too much. ‘‘You can do a real disservice to people if you open up a big can of worms inside them and then just let them go out the door,” says one nursing supervisor.
In a way, the Hillcrest hospital is an indigent’s version of the Golden Door health spa: an expensive indulgence (at about $180 a day, per person, mostly picked up by the taxpayer) whose limited and short-term effectiveness is based on the creed of the quick fix. And like a health spa, the length of a person’s stay at CMH is determined not at all by his progress toward health, but by money, bureaucratic strictures, and the need to make room for those newly arriving. Without special circumstances, patients can’t be held longer than seventeen days, and they are routinely discharged simply because there is someone being admitted who is more needful of immediate care. CMH cannot turn away anybody who has been deemed gravely disabled or dangerous either to themselves or to others. ‘‘Instead of saying, ‘Come on in, we’ll help you with your problems,’ ” laments Jean Karr, chief nurse, ‘‘we ask about legalities, laws, rights. And when he leaves, he’s not really better, he’s just learned more about his legal possibilities within the system.”
But given all that should rightfully kill it, the urge to help is still strong among the staff. "Sometimes it’s just a job, and sometimes you can get motivated to really help,” says one nurse’s assistant. Call him Phil. ‘‘You can get motivated by realizing that a certain guy’s extremely dangerous, and shouldn’t see the light of day; I’ve seen murderers in here, who should stay for twenty-five years. You can also get motivated by seeing a guy you can help. Every now and then you get that rare individual who was basically functioning, and his world just dropped out from under him, and he ended up here. We can help that guy.” Phil is an ex-hospital corpsman not yet thirty; he says his Navy training overqualifies him for this job, which pays between five and six dollars per hour. Given the danger (assaults on and injuries to staff are common) and the responsibility (nurses lead group therapy sessions and have more contact, and perhaps even more influence, on patients than do doctors), none of the staff, including Phil, feels justly compensated. But it’s a job. And an education. ‘‘We have a guy in here who chopped off his own hand,” he says, still in awe. “They sewed it back on. He bit off a couple of his fingers. Bit ’em off." These incidents — other nurses tell of three men who cut off their own penises in the ward bathroom — are not looked upon from a clinical perspective by the staff, as might be the wont of a psychiatrist. The nurses are shocked by these things, and their reactions aren't sifted through an academic mesh. The patients seem to sense that the nurses don’t consciously set themselves apart with intellectual or emotional distance, and that in itself is therapeutic. For many patients, this human civility is the only workable therapy. Aside from drugs, of course.
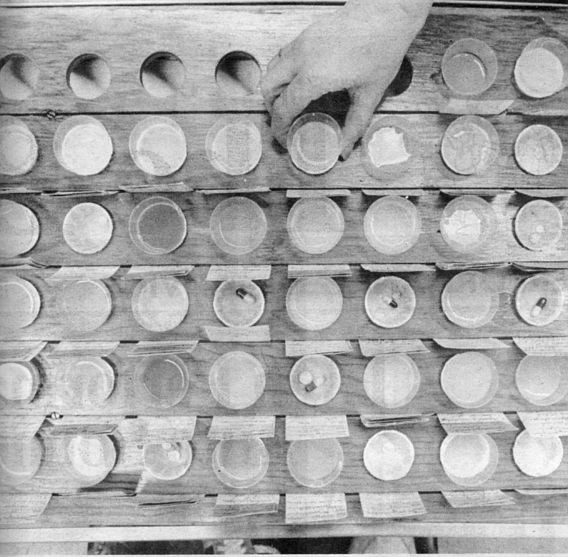
Herman Billings, a small black man in his fifties, was admitted to the hospital on a recent Saturday afternoon. He was brought in by the police after they caught him jumping in front of cars on the street. He was generally calm and cooperative with the nurses and obviously in familiar surroundings, but when it came time for him to take his medication, which was almost immediately after he arrived at the nursing station, he would have none of it. ‘‘Now, Herman, doctor wants you to take this medicine,” explained the nurse in charge, holding out a little paper cup filled with Haldol and lilting her voice like a mother talking to a juvenile. Herman, shirtless and vulnerable, stands by himself near the nursing station and says he doesn't want no medicine.
‘‘I just want a shower, a shave, and some nourishment,” he says straightforwardly, trying to be reasonable.
‘‘Now, Herman, this medicine is good for you. If you don’t swallow it we’ll have to give it to you by injection.”
‘‘No ma’am, I don’t want none of that. I just want to get cleaned up a little.”
“Okay, Herman.” Someone goes to summon a couple of male nurses, and Herman, still standing alone, starts to moan like a cornered animal.
“Ohhh Gaaawd!” he yells in an unpanicked voice. ‘‘Thank Gaaawd! Mercy!” He stomps his foot. “Mercyyyyy!”
As the men approach calmly and try to reassure Herman, a desk clerk looks up at me and says, ‘‘Can you imagine what it was like before we had drugs? We used to have to wrap ’em in wet towels to control ’em.”
‘‘Man, all I want is a shower and a shave,” Herman beseeches the male nurses. They talk softly to him as the chief nurse comes out of the medication room with a syringe full of Haldol.
“Come on, Herman, it’s to help you.”
‘‘I don’t even know what it is. Please. Pleeeeeease!”
The men muscle him through the locker-room door and press him firmly against one of the tall beige lockers. ‘‘All right, all right. I’ll take it,” Herman yells, but they aren’t turning him loose now. The chief nurse undoes Herman’s pants and pulls them down, exposing his small ebony butt. Herman’s breath comes fast and shallow. The black male nurse presses his face into Herman’s and stares intensely into his eyes. ‘‘It’s cool, man, it’s cool,” he says soothingly.
‘‘Don’t tighten up, Herman,” commands the nurse with the needle. She slaps his butt once, twice.
"All right, I’ll take it,” Herman insists.
‘‘It’s cool, man.” The male nurse tightens his grip. The needle is in. Herman relaxes like a collapsing balloon.
He was released four days later on his own.
Ultimately, of course, it’s the psychiatrists at CMH who are in charge of the patients’ treatment. They determine who gets into the hospital, what kind of disorder he's suffering from, what drugs, if any, to administer, and when a patient is ready to be released. For fifteen years Dr. Socrates Pappas has worked at the hospital, and now he’s the supervising psychiatrist, with a small office that used to be a seclusion room just a few steps away from the nurses’ station. A humorous and nervous and approachable man, Pappas is the last one who’d claim much of a success rate in straightening out his patients’ lives. But when I questioned the benefits of the psychotropic drugs, his response was immediate: “Yes, the medication does help people. Without the drugs, many of them would be locked up. It’s better that they’re not locked up. That’s better. Families come in and say, ‘Doctor, if you’ll just give him his medicine, and if he’ll take it, I want him home.’ When he doesn’t take it, he throws the TV through the picture window, chokes dad, barricades himself in his room, hears voices. When he takes it, he may still have those urges, but he’s able not to act on them. He can live at home. That’s better."
Dr. Pappas estimates that only about ten percent of his patients really want to talk to him about their personal problems, “and the other ninety percent go back to wherever they were before they came in." Though he says he’s not a rebel, he holds personal beliefs about the treatment of the mentally ill that run counter to the system. If it were up to him, he might like to write down that somebody was a mean, nasty old cuss instead of a manic depressive with severe assaultive tendencies. “But the system, and the paperwork, demands those labels.” He even has personal doubts about committing and detaining people against their will. Some in his profession, and even on his ward, believe that totally structuring a patient's environment and relieving him of every responsibility is the ultimate dehumanization, and that in the long run it works against that person’s mental health. So what do you do with people who have serious psychological problems? If they don’t seek help voluntarily says Pappas, maybe we should try just leaving them alone. “If the voices tell him to break a window and he does, arrest him. Make him responsible for what he hears.’’ Though it sounds like a radical theory, how much less effective than the current system could it be?
As we talked, it became clear that Pappas was edgy about something. The conversation worked its way around to violence on the ward, and the psychiatrist boasted that working fifteen years in a place considered more dangerous than a jailhouse, he had yet to be attacked. Then came this: thirteen days before, Pappas was awakened in the night by the telephone. The man on the other end of the line was a former patient in the hospital who didn’t like the way Pappas had treated him, and he told the doctor that he knew where he lived, what car he drove, what his schedule was, and that he’d better get a bulletproof vest because in two weeks the doctor was going to be killed. Pappas had never been threatened like that before, and he took it seriously enough to call the police. After the psychiatrist told the story several different times to incredulous but sympathetic detectives, a patrolman was dispatched to talk to him at CMH. Pappas told Sgt. Rice the story, who listened politely and then said what the doctor had heard umpteen times before: there was nothing the police could do. But then Sgt. Rice did offer a solution, of sorts. He said that if Pappas should receive a threatening call like that two more times, he should get his phone number changed, “because no citizen should have to put up with that kind of thing.’’ We both laughed at the absurdity of such a solution. It wasn’t until later that I realized the policeman had given Dr. Pappas the same prescription that his own hospital dispenses in little paper cups every day.
Comments